Clin Endosc.
2023 Jul;56(4):490-498. 10.5946/ce.2022.130.
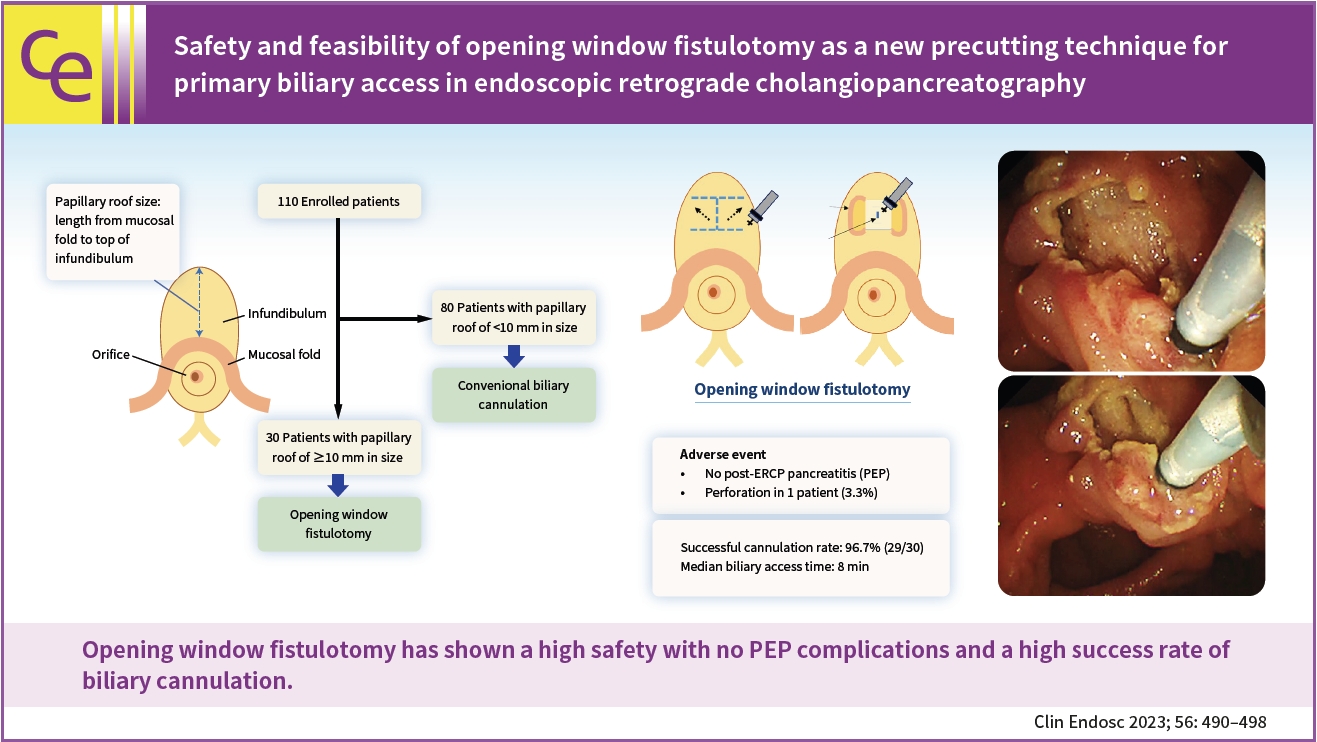
Safety and feasibility of opening window fistulotomy as a new precutting technique for primary biliary access in endoscopic retrograde cholangiopancreatography
- Affiliations
-
- 1Department of Gastroenterology, Aichi Cancer Center Hospital, Nagoya, Japan
- KMID: 2544572
- DOI: http://doi.org/10.5946/ce.2022.130
Abstract
- Background/Aims
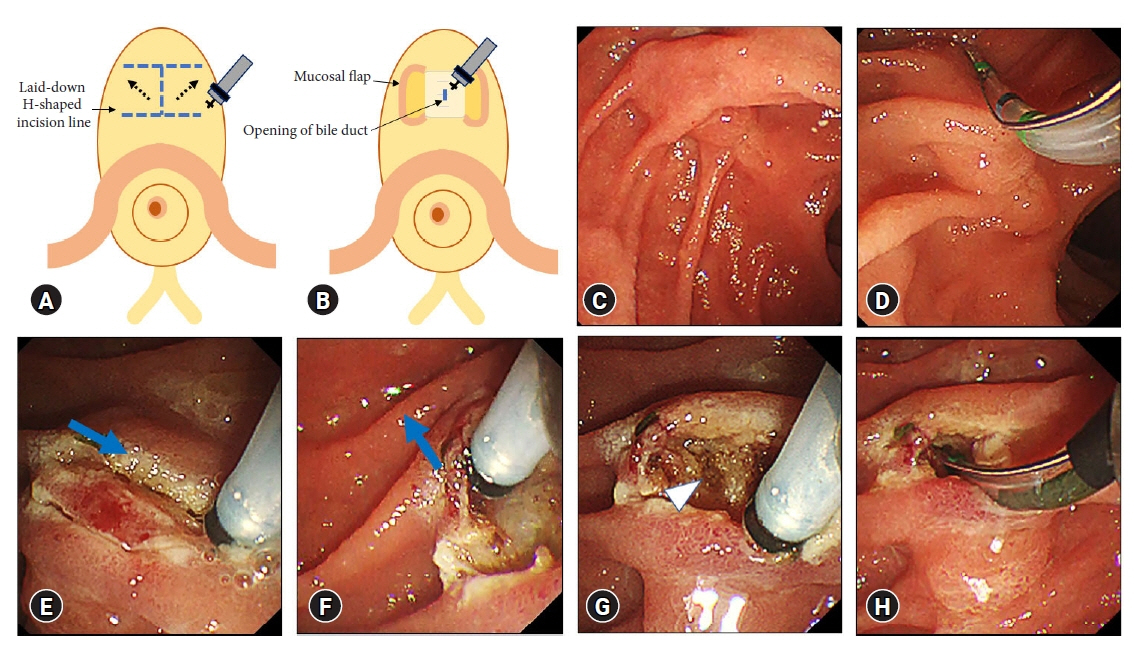
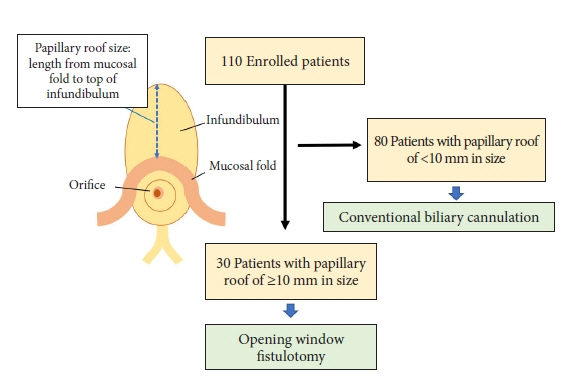
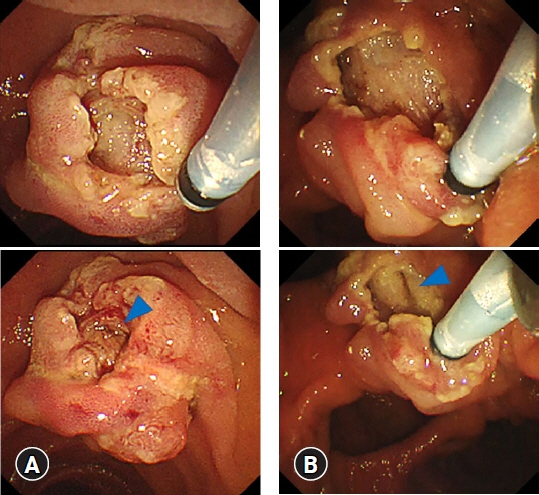
Post-endoscopic retrograde cholangiopancreatography pancreatitis (PEP) is the most common and serious complication of endoscopic retrograde cholangiopancreatography. To prevent this event, a unique precutting method, termed opening window fistulotomy, was performed in patients with a large infundibulum as the primary procedure for biliary cannulation, whereby a suprapapillary laid-down H-shaped incision was made without touching the orifice. This study aimed to assess the safety and feasibility of this novel technique.
Methods
One hundred and ten patients were prospectively enrolled in this study. Patients with a papillary roof size ≥10 mm underwent opening window fistulotomy for primary biliary access. In addition, the incidence of complications and success rate of biliary cannulation were evaluated.
Results
The median size of the papillary roof was 6 mm (range, 3–20 mm). Opening window fistulotomy was performed in 30 patients (27.3%), none of whom displayed PEP. Duodenal perforation was recorded in one patient (3.3%), which was resolved by conservative treatment. The cannulation rate was high (96.7%, 29/30 patients). The median duration of biliary access was 8 minutes (range, 3–15 minutes).
Conclusions
Opening window fistulotomy demonstrated its feasibility for primary biliary access by achieving great safety with no PEP complications and a high success rate for biliary cannulation.
Keyword
Figure
Reference
-
1. Bailey AA, Bourke MJ, Williams SJ, et al. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008; 40:296–301.2. Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. Gastrointest Endosc. 2005; 61:112–125.3. Larkin CJ, Huibregtse K. Precut sphincterotomy: indications, pitfalls, and complications. Curr Gastroenterol Rep. 2001; 3:147–153.4. Williams EJ, Taylor S, Fairclough P, et al. Are we meeting the standards set for endoscopy?: results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut. 2007; 56:821–829.5. Cheng CL, Sherman S, Watkins JL, et al. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006; 101:139–147.6. Dumonceau JM, Andriulli A, Elmunzer BJ, et al. Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) guideline: updated June 2014. Endoscopy. 2014; 46:799–815.7. Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001; 54:425–434.8. Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998; 48:1–10.9. Masci E, Mariani A, Curioni S, et al. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: a meta-analysis. Endoscopy. 2003; 35:830–834.10. Masci E, Toti G, Mariani A, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001; 96:417–423.11. Testoni PA, Mariani A, Giussani A, et al. Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterol. 2010; 105:1753–1761.12. Wang P, Li ZS, Liu F, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009; 104:31–40.13. Kaffes AJ, Sriram PV, Rao GV, et al. Early institution of pre-cutting for difficult biliary cannulation: a prospective study comparing conventional vs. a modified technique. Gastrointest Endosc. 2005; 62:669–674.14. Mariani A, Di Leo M, Giardullo N, et al. Early precut sphincterotomy for difficult biliary access to reduce post-ERCP pancreatitis: a randomized trial. Endoscopy. 2016; 48:530–535.15. Testoni PA, Giussani A, Vailati C, et al. Precut sphincterotomy, repeated cannulation and post-ERCP pancreatitis in patients with bile duct stone disease. Dig Liver Dis. 2011; 43:792–796.16. Choudhary A, Winn J, Siddique S, et al. Effect of precut sphincterotomy on post-endoscopic retrograde cholangiopancreatography pancreatitis: a systematic review and meta-analysis. World J Gastroenterol. 2014; 20:4093–4101.17. Jang SI, Kim DU, Cho JH, et al. Primary needle-knife fistulotomy versus conventional cannulation method in a high-risk cohort of post-endoscopic retrograde cholangiopancreatography pancreatitis. Am J Gastroenterol. 2020; 115:616–624.18. Jin YJ, Jeong S, Lee DH. Utility of needle-knife fistulotomy as an initial method of biliary cannulation to prevent post-ERCP pancreatitis in a highly selected at-risk group: a single-arm prospective feasibility study. Gastrointest Endosc. 2016; 84:808–813.19. Mavrogiannis C, Liatsos C, Romanos A, et al. Needle-knife fistulotomy versus needle-knife precut papillotomy for the treatment of common bile duct stones. Gastrointest Endosc. 1999; 50:334–339.20. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393.21. Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996; 335:909–918.22. Sherman S, Ruffolo TA, Hawes RH, et al. Complications of endoscopic sphincterotomy: a prospective series with emphasis on the increased risk associated with sphincter of Oddi dysfunction and nondilated bile ducts. Gastroenterology. 1991; 101:1068–1075.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comments on ‘Safety and feasibility of opening window fistulotomy as a new precutting technique for primary biliary access in endoscopic retrograde cholangiopancreatography’
- Optimal Use of Wire-Assisted Techniques and Precut Sphincterotomy
- Endoscopic Ultrasound-Guided Biliary Access, with Focus on Technique and Practical Tips
- Endoscopic Guided Biliary Drainage: How Can We Achieve Efficient Biliary Drainage?
- The Usefulness of Cap-assisted Endoscopic Retrograde Cholangiopancreatography for Cannulation Complicated by a Periampullary Diverticulum