J Korean Med Sci.
2023 Jul;38(28):e212. 10.3346/jkms.2023.38.e212.
Associations of Perioperative Red Blood Cell Transfusion With Outcomes of Kidney Transplantation in Korea Over a 16-Year Period
- Affiliations
-
- 1Department of Laboratory Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Laboratory Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 3Research Institute, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 4Department of Laboratory Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2544473
- DOI: http://doi.org/10.3346/jkms.2023.38.e212
Abstract
- Background
This study investigated the associations between transfusion of different types of red blood cell (RBC) preparations and kidney allograft outcomes after kidney transplantation (KT) over a 16-year period in Korea using a nationwide population-based cohort.
Methods
We investigated the reported use of RBCs during hospitalization for KT surgery, rejection, and graft failure status using nationwide data from the National Health Information Database (2002–2017). The associations between the type of perioperative RBC product and transplant outcomes were evaluated among four predefined groups: no RBC transfusion, filtered RBCs, washed RBCs, and packed RBCs (pRBCs).
Results
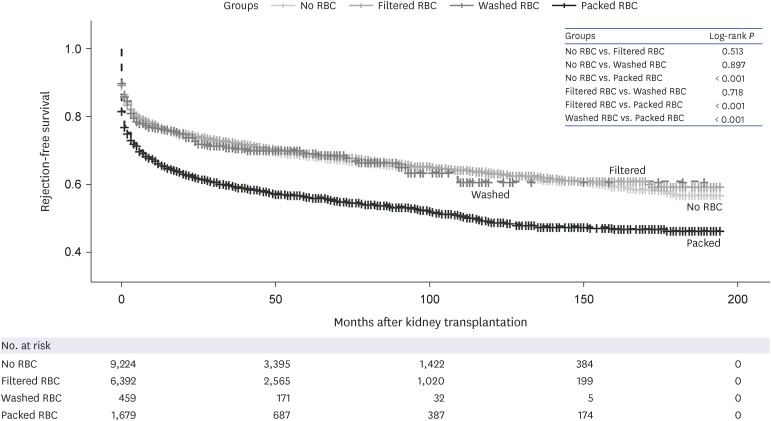
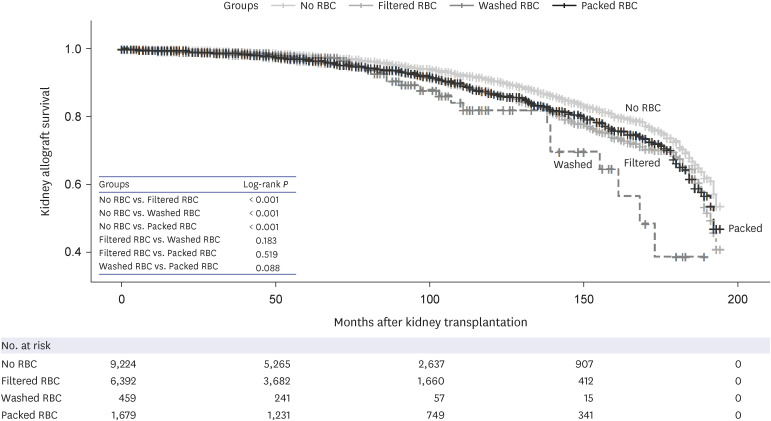
A total of 17,754 KT patients was included, among which 8,530 (48.0%) received some type of RBC transfusion. Of the patients who received RBC transfusion, 74.9%, 19.7%, and 5.4% received filtered RBCs, pRBCs, or washed RBCs, respectively. Regardless of the type of RBC products, the proportions of acute rejection and graft failure was significantly greater in patients receiving transfusion (P < 0.001). Cox proportional hazards regression analyses showed that the filtered RBC and pRBC groups were significantly associated with both rejection and graft failure. The washed RBC group also had hazard ratios greater than 1.0 for rejection and graft failure, but the association was not significant. Rejection-free survival of the pRBC group was significantly lower than that of the other groups (P < 0.001, log-rank test), and graft survival for the no RBC transfusion group was significantly greater than in the other groups (P < 0.001, log-rank test).
Conclusion
Perioperative RBC transfusion was associated with poor graft outcomes. Notably, transfusion of pRBCs significantly increased transplant rejection. Therefore, careful consideration of indications for RBC transfusion and selection of the appropriate type of RBCs is necessary, especially for patients at high risk of rejection or graft failure.
Figure
Reference
-
1. Johansen KL, Chertow GM, Foley RN, Gilbertson DT, Herzog CA, Ishani A, et al. US Renal Data System 2020 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2021; 77(4):Suppl 1. A7–A8. PMID: 33752804.2. Stauffer ME, Fan T. Prevalence of anemia in chronic kidney disease in the United States. PLoS One. 2014; 9(1):e84943. PMID: 24392162.3. Koo BN, Kwon MA, Kim SH, Kim JY, Moon YJ, Park SY, et al. Korean clinical practice guideline for perioperative red blood cell transfusion from Korean Society of Anesthesiologists. Korean J Anesthesiol. 2019; 72(2):91–118. PMID: 30513567.4. Vanrenterghem Y, Ponticelli C, Morales JM, Abramowicz D, Baboolal K, Eklund B, et al. Prevalence and management of anemia in renal transplant recipients: a European survey. Am J Transplant. 2003; 3(7):835–845. PMID: 12814475.5. Akalin E. A new treatment option for highly sensitized patients awaiting kidney transplantation. Am J Kidney Dis. 2018; 71(4):458–460. PMID: 29352605.6. Snyder EL. Prevention of HLA alloimmunization: role of leukocyte depletion and UV-B irradiation. Yale J Biol Med. 1990; 63(5):419–427. PMID: 2293501.7. Scornik JC, Meier-Kriesche HU. Blood transfusions in organ transplant patients: mechanisms of sensitization and implications for prevention. Am J Transplant. 2011; 11(9):1785–1791. PMID: 21883910.8. Balasubramaniam GS, Morris M, Gupta A, Mesa IR, Thuraisingham R, Ashman N. Allosensitization rate of male patients awaiting first kidney grafts after leuko-depleted blood transfusion. Transplantation. 2012; 93(4):418–422. PMID: 22228416.9. Fidler S, Swaminathan R, Lim W, Ferrari P, Witt C, Christiansen FT, et al. Peri-operative third party red blood cell transfusion in renal transplantation and the risk of antibody-mediated rejection and graft loss. Transpl Immunol. 2013; 29(1-4):22–27. PMID: 24090807.10. Hong D, Wu S, Pu L, Wang F, Wang J, Wang Z, et al. Abdominal aortic calcification is not superior over other vascular calcification in predicting mortality in hemodialysis patients: a retrospective observational study. BMC Nephrol. 2013; 14(1):120. PMID: 23738982.11. Leffell MS, Kim D, Vega RM, Zachary AA, Petersen J, Hart JM, et al. Red blood cell transfusions and the risk of allosensitization in patients awaiting primary kidney transplantation. Transplantation. 2014; 97(5):525–533. PMID: 24300013.12. Ferrandiz I, Congy-Jolivet N, Del Bello A, Debiol B, Trébern-Launay K, Esposito L, et al. Impact of early blood transfusion after kidney transplantation on the incidence of donor-specific anti-HLA antibodies. Am J Transplant. 2016; 16(9):2661–2669. PMID: 26998676.13. Lee K, Lee S, Jang EJ, Kim GH, Yoo S, Lee M, et al. The association between peri-transplant RBC transfusion and graft failure after kidney transplantation: a nationwide cohort study. J Clin Med. 2021; 10(16):3750. PMID: 34442041.14. Kim B, Kang M, Lee JK, Lee HS, Park Y. Perioperative blood usage and therapeutic plasma exchange in kidney transplantation during a 16-year period in South Korea. Blood Transfus. 2021; 19(2):102–112. PMID: 32530400.15. Gaiffe E, Vernerey D, Bardiaux L, Leroux F, Meurisse A, Bamoulid J, et al. Early post-transplant red blood cell transfusion is associated with an increased risk of transplant failure: a nationwide French study. Front Immunol. 2022; 13:854850. PMID: 35711440.16. Bianchi M, Vaglio S, Pupella S, Marano G, Facco G, Liumbruno GM, et al. Leucoreduction of blood components: an effective way to increase blood safety? Blood Transfus. 2016; 14(2):214–227. PMID: 26710353.17. Sharma RR, Marwaha N. Leukoreduced blood components: advantages and strategies for its implementation in developing countries. Asian J Transfus Sci. 2010; 4(1):3–8. PMID: 20376259.18. Cheol Seong S, Kim YY, Khang YH, Heon Park J, Kang HJ, Lee H, et al. Data resource profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46(3):799–800. PMID: 27794523.19. Kim B, Kang M, Kim Y, Lee HS, Kim B, Lee JJ, et al. De novo cancer incidence after kidney transplantation in South Korea from 2002 to 2017. J Clin Med. 2021; 10(16):3530. PMID: 34441826.20. Lee HS, Kang M, Kim B, Park Y. Outcomes of kidney transplantation over a 16-year period in Korea: an analysis of the National Health Information Database. PLoS One. 2021; 16(2):e0247449. PMID: 33606787.21. Massicotte-Azarniouch D, Sood MM, Fergusson DA, Chassé M, Tinmouth A, Knoll GA. Blood transfusion and adverse graft-related events in kidney transplant patients. Kidney Int Rep. 2021; 6(4):1041–1049. PMID: 33912754.22. Hassan S, Regan F, Brown C, Harmer A, Anderson N, Beckwith H, et al. Shared alloimmune responses against blood and transplant donors result in adverse clinical outcomes following blood transfusion post-renal transplantation. Am J Transplant. 2019; 19(6):1720–1729. PMID: 30582278.23. Jalalonmuhali M, Carroll RP, Tsiopelas E, Clayton P, Coates PT. Development of de novo HLA donor specific antibodies (HLA-DSA), HLA antibodies (HLA-Ab) and allograft rejection post blood transfusion in kidney transplant recipients. Hum Immunol. 2020; 81(7):323–329. PMID: 32327243.24. O’Brien FJ, Lineen J, Kennedy CM, Phelan PJ, Kelly PO, Denton MD, et al. Effect of perioperative blood transfusions on long term graft outcomes in renal transplant patients. Clin Nephrol. 2012; 77(6):432–437. PMID: 22595384.25. Cardigan R, New HV, Tinegate H, Thomas S. Washed red cells: theory and practice. Vox Sang. 2020; 115(8):606–616. PMID: 32633823.26. West LJ, Pollock-Barziv SM, Dipchand AI, Lee KJ, Cardella CJ, Benson LN, et al. ABO-incompatible heart transplantation in infants. N Engl J Med. 2001; 344(11):793–800. PMID: 11248154.27. Aston A, Cardigan R, Bashir S, Proffitt S, New H, Brown C, et al. Washing red cells after leucodepletion does not decrease human leukocyte antigen sensitization risk in patients with chronic kidney disease. Pediatr Nephrol. 2014; 29(10):2005–2011. PMID: 24777534.28. Richie RE, Niblack GD, Johnson HK, Green WF, MacDonell RC, Turner BI, et al. Factors influencing the outcome of kidney transplants. Ann Surg. 1983; 197(6):672–677. PMID: 6344816.29. Jung HY, Kim SH, Seo MY, Cho SY, Yang Y, Choi JY, et al. Characteristics and clinical significance of de novo donor-specific anti-HLA antibodies after kidney transplantation. J Korean Med Sci. 2018; 33(34):e217. PMID: 30127706.30. Kim HW, Kang SW, Lee HY, Choi DH, Shim WH, Kim SI, et al. Correlates of the severity of coronary atherosclerosis in long-term kidney transplant patients. J Korean Med Sci. 2010; 25(5):706–711. PMID: 20436705.31. Kwon CH, Lee SK, Ha J. Trend and outcome of Korean patients receiving overseas solid organ transplantation between 1999 and 2005. J Korean Med Sci. 2011; 26(1):17–21. PMID: 21218024.32. Oh HW, Jang EJ, Kim GH, Yoo S, Lee H, Lim TY, et al. Effect of institutional kidney transplantation case-volume on post-transplant graft failure: a retrospective cohort study. J Korean Med Sci. 2019; 34(40):e260. PMID: 31625292.33. Gafter-Gvili A, Gafter U. Posttransplantation anemia in kidney transplant recipients. Acta Haematol. 2019; 142(1):37–43. PMID: 30970356.34. Chhabra D, Grafals M, Skaro AI, Parker M, Gallon L. Impact of anemia after renal transplantation on patient and graft survival and on rate of acute rejection. Clin J Am Soc Nephrol. 2008; 3(4):1168–1174. PMID: 18463170.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent trends in perioperative blood transfusion during elective kidney transplantation
- Recent perioperative blood transfusion in elective kidney transplantation
- Clinical impact of early blood transfusion after kidney transplantation
- Clinical impact of early blood transfusion after kidney transplantation
- Transfusion status in liver and kidney transplantation recipients: results from nationwide claims database