J Korean Med Sci.
2023 Jun;38(24):e181. 10.3346/jkms.2023.38.e181.
Comparison of Clinical Manifestations of Kawasaki Disease According to SARS-CoV-2 Antibody Positivity
- Affiliations
-
- 1Department of Pediatrics, Jeonbuk National University Children’s Hospital, Jeonju, Korea
- 2Research Institute of Clinical Medicine of Jeonbuk National University, Jeonju, Korea
- KMID: 2543964
- DOI: http://doi.org/10.3346/jkms.2023.38.e181
Abstract
- Background
Kawasaki disease (KD) is the most common cause of acquired heart disease in paediatric patients, with infectious agents being the main cause. This study aimed to determine whether there are differences in the clinical manifestations of KD between patients with and without severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibodies.
Methods
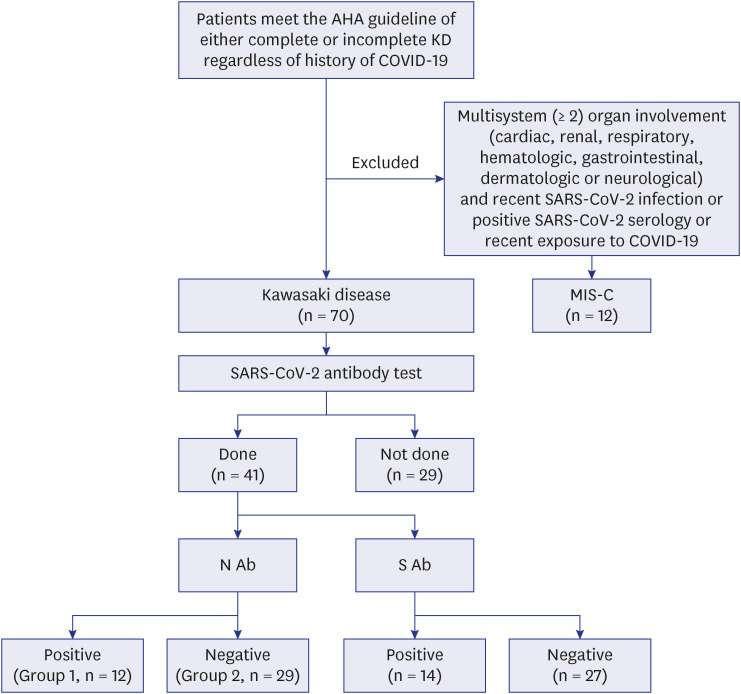
From January 1, 2021 to August 15, 2022, 82 patients with analysable echocardiographic data were diagnosed with KD. Twelve patients with multisystem inflammatory syndrome in children were excluded. Serologic tests were performed by chemiluminescence immunoassay for both the nucleocapsid (N) and the spike (S) proteins in blood samples. Among the 70 patients diagnosed with KD at Jeonbuk University Children’s Hospital, the SARS-CoV-2 antibody test was performed in 41 patients.
Results
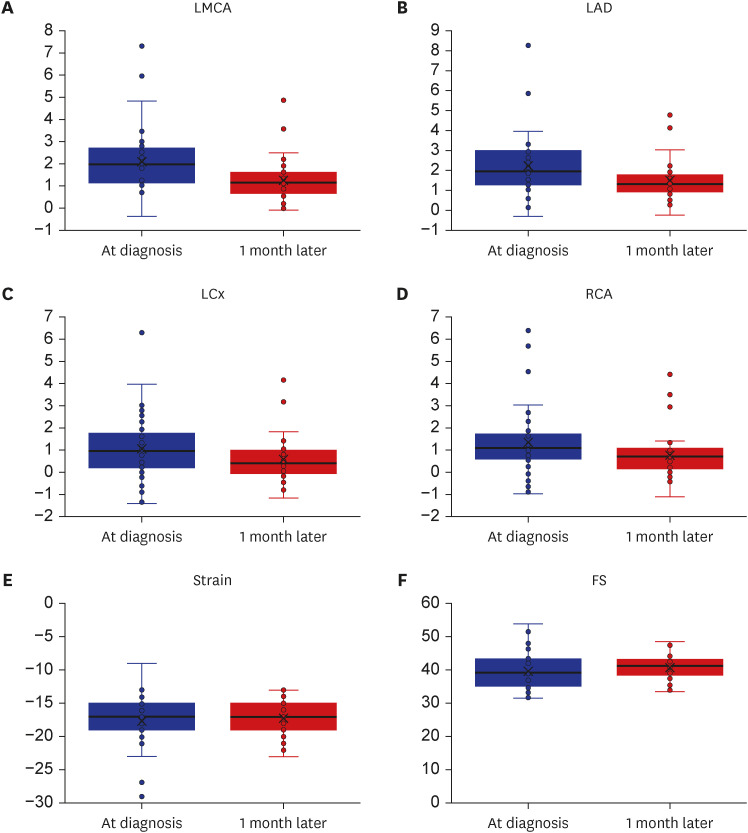
The SARS-CoV-2 antibody test results for the N antigen were positive in 12 patients, while those for S protein were positive in 14 patients. N antigen SARS-CoV-2 antibodypositive KD was different from N antigen SARS-CoV-2 antibody-negative KD in terms of sex (male predominance in the positive group, 83.3% vs. female predominance in the negative group 62.1%, P = 0.008) and the incidence of refractory KD (41.7% vs. 10.3%, P = 0.034). The pro-B-type natriuretic peptide level was lower in the N-antigen SARS-CoV-2 antibody-positive KD group than that in the negative group (518.9 ± 382.6, 1,467.0 ± 2,417.6, P = 0.049). No significant differences in the echocardiographic findings between both groups were noted. In the multi-variable analysis, SARS-CoV-2 antibody (N antigen) was the only predictor of refractory KD (odds ratio, 13.70; 95% confidence interval, 1.63–115.44; P = 0.016).
Conclusion
High incidence of intravenous immunoglobulin-refractory KD may occur in up to 40% of the patients having recent history of coronavirus disease 2019. For patients having KD with N-type SARS-CoV-2 antibody positivity, adjunctive treatment, such as corticosteroids, can be considered as the first line of treatment.
Figure
Reference
-
1. Soni PR, Noval Rivas M, Arditi M. A comprehensive update on Kawasaki disease vasculitis and myocarditis. Curr Rheumatol Rep. 2020; 22(2):6. PMID: 32020498.2. Ishii M, Ebato T, Kato H. History and future of treatment for acute stage Kawasaki disease. Korean Circ J. 2020; 50(2):112–119. PMID: 31845551.3. Tacke CE, Breunis WB, Pereira RR, Breur JM, Kuipers IM, Kuijpers TW. Five years of Kawasaki disease in the Netherlands: a national surveillance study. Pediatr Infect Dis J. 2014; 33(8):793–797. PMID: 24463809.4. Dergun M, Kao A, Hauger SB, Newburger JW, Burns JC. Familial occurrence of Kawasaki syndrome in North America. Arch Pediatr Adolesc Med. 2005; 159(9):876–881. PMID: 16143748.5. Rodó X, Ballester J, Curcoll R, Boyard-Micheau J, Borràs S, Morguí JA. Revisiting the role of environmental and climate factors on the epidemiology of Kawasaki disease. Ann N Y Acad Sci. 2016; 1382(1):84–98. PMID: 27603178.6. Rowley AH, Baker SC, Shulman ST, Rand KH, Tretiakova MS, Perlman EJ, et al. Ultrastructural, immunofluorescence, and RNA evidence support the hypothesis of a “new” virus associated with Kawasaki disease. J Infect Dis. 2011; 203(7):1021–1030. PMID: 21402552.7. Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MB, et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020; 383(4):334–346. PMID: 32598831.8. Kim H, Shim JY, Ko JH, Yang A, Shim JW, Kim DS, et al. Multisystem inflammatory syndrome in children related to COVID-19: the first case in Korea. J Korean Med Sci. 2020; 35(43):e391. PMID: 33169560.9. Lee PY, Day-Lewis M, Henderson LA, Friedman KG, Lo J, Roberts JE, et al. Distinct clinical and immunological features of SARS-CoV-2-induced multisystem inflammatory syndrome in children. J Clin Invest. 2020; 130(11):5942–5950. PMID: 32701511.10. Kim BJ, Choi A, Kim HS, Oh JH, Lee JY, Kim S, et al. Changes in the clinical characteristics of Kawasaki disease after coronavirus disease (COVID-19) pandemic: a database analysis. J Korean Med Sci. 2022; 37(20):e141. PMID: 35607738.11. Jo DS. Kawasaki disease during COVID-19 pandemic in Korea - data were added but are needed more. J Korean Med Sci. 2022; 37(20):e170. PMID: 35607745.12. Esmaeilzadeh H, Mortazavi N, Salehi A, Fatemian H, Dehghani SM, Vali M, et al. Effect of COVID-19 on Kawasaki disease: decrease age of onset and increase skin manifestation. BMC Pediatr. 2021; 21(1):571. PMID: 34903208.13. McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017; 135(17):e927–e999. PMID: 28356445.14. Loke YH, Berul CI, Harahsheh AS. Multisystem inflammatory syndrome in children: is there a linkage to Kawasaki disease? Trends Cardiovasc Med. 2020; 30(7):389–396. PMID: 32702413.15. Dallaire F, Dahdah N. New equations and a critical appraisal of coronary artery Z scores in healthy children. J Am Soc Echocardiogr. 2011; 24(1):60–74. PMID: 21074965.16. Pettersen MD, Du W, Skeens ME, Humes RA. Regression equations for calculation of z scores of cardiac structures in a large cohort of healthy infants, children, and adolescents: an echocardiographic study. J Am Soc Echocardiogr. 2008; 21(8):922–934. PMID: 18406572.17. Kobayashi T, Inoue Y, Takeuchi K, Okada Y, Tamura K, Tomomasa T, et al. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation. 2006; 113(22):2606–2612. PMID: 16735679.18. World Health Organization. WHO coronavirus (COVID-19) dashboard. Updated 2022. Accessed November 24, 2022. https://covid19.who.int/?gclid=CjwKCAjwvNaYBhA3EiwACgndgvBaZFTI6ouUgP-qzqhArIS5Y0ebO6gwzUVbaMYP6x6gO0wIQBum4xoCFxIQAvD_BwE .19. Sharma C, Ganigara M, Galeotti C, Burns J, Berganza FM, Hayes DA, et al. Multisystem inflammatory syndrome in children and Kawasaki disease: a critical comparison. Nat Rev Rheumatol. 2021; 17(12):731–748. PMID: 34716418.20. Toubiana J, Poirault C, Corsia A, Bajolle F, Fourgeaud J, Angoulvant F, et al. Kawasaki-like multisystem inflammatory syndrome in children during the COVID-19 pandemic in Paris, France: prospective observational study. BMJ. 2020; 369:m2094. PMID: 32493739.21. Bartsch YC, Wang C, Zohar T, Fischinger S, Atyeo C, Burke JS, et al. Humoral signatures of protective and pathological SARS-CoV-2 infection in children. Nat Med. 2021; 27(3):454–462. PMID: 33589825.22. Carter MJ, Fish M, Jennings A, Doores KJ, Wellman P, Seow J, et al. Peripheral immunophenotypes in children with multisystem inflammatory syndrome associated with SARS-CoV-2 infection. Nat Med. 2020; 26(11):1701–1707. PMID: 32812012.23. Swartz MD, DeSantis SM, Yaseen A, Brito FA, Valerio-Shewmaker MA, Messiah SE, et al. Antibody duration after infection from SARS-CoV-2 in the Texas Coronavirus Antibody Response Survey. J Infect Dis. 2023; 227(2):193–201. PMID: 35514141.24. Han MS, Um J, Lee EJ, Kim KM, Chang SH, Lee H, et al. Antibody responses to SARS-CoV-2 in children With COVID-19. J Pediatric Infect Dis Soc. 2022; 11(6):267–273. PMID: 35275210.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in SARS-CoV-2 antibody titers 6 months after the booster dose of BNT162b2 COVID-19 vaccine among health care workers
- SARS-CoV-2 Antibodies in Children with Chronic Disease from a Pediatric Gastroenterology Outpatient Clinic
- Clinical Usefulness of SARS-CoV-2 Antibody Test
- Three Cases of SARS-CoV-2 Infection with Cold Antibody of Undetermined Specificity in Antibody Screening in Transfusion Labs
- Experimental Animal Models of Coronavirus Infections: Strengths and Limitations