J Korean Med Sci.
2023 Jun;38(23):e180. 10.3346/jkms.2023.38.e180.
Effect of Wearing Personal Protective Equipment (PPE) for COVID-19 Treatment on Blood Culture Contamination: Implication for Optimal PPE Strategies
- Affiliations
-
- 1Department of Laboratory Medicine, Seoul National University Hospital, Seoul, Korea
- 2Department of Laboratory Medicine, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2543882
- DOI: http://doi.org/10.3346/jkms.2023.38.e180
Abstract
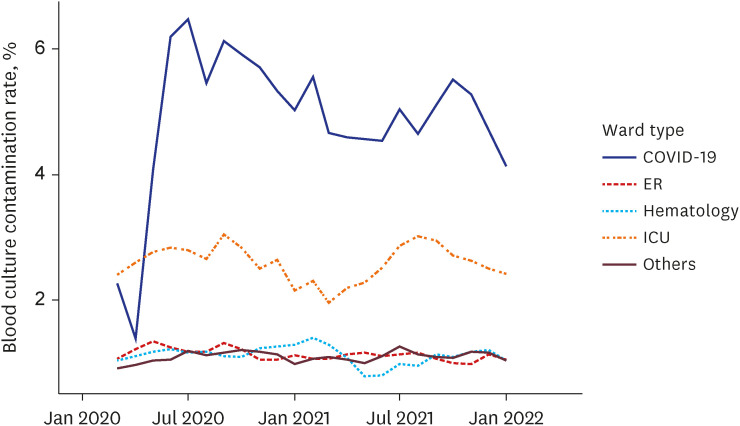
- The personal protective equipment (PPE) used to minimize exposure to hazards can hinder healthcare workers from performing sophisticated procedures. We retrospectively reviewed 77,535 blood cultures (202,012 pairs) performed in 28,502 patients from January 2020 to April 2022. The contamination rate of all blood cultures was significantly elevated in the coronavirus disease 2019 ward at 4.68%, compared to intensive care units at 2.56%, emergency rooms at 1.13%, hematology wards at 1.08%, and general wards at 1.07% (All of P < 0.001). This finding implies that wearing PPE might interfere with adherence to the aseptic technique. Therefore, a new PPE policy is needed that considers the balance between protecting healthcare workers and medical practices.
Figure
Reference
-
1. Doern GV, Carroll KC, Diekema DJ, Garey KW, Rupp ME, Weinstein MP, et al. Practical guidance for clinical microbiology laboratories: a comprehensive update on the problem of blood culture contamination and a discussion of methods for addressing the problem. Clin Microbiol Rev. 2019; 33(1):e00009-19. PMID: 31666280.
Article2. CLSI. Principles and Procedures for Blood Cultures. 2nd ed. Wayne, PA, USA: Clinical and Laboratory Standards Institute;2022.3. WHO. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages: interim guidance. Updated 2020. Accessed October 18, 2022. https://apps.who.int/iris/handle/10665/338033 .4. Sepulveda J, Westblade LF, Whittier S, Satlin MJ, Greendyke WG, Aaron JG, et al. Bacteremia and blood culture utilization during COVID-19 surge in New York City. J Clin Microbiol. 2020; 58(8):e00875-20. PMID: 32404482.
Article5. Ohki R, Fukui Y, Morishita N, Iwata K. Increase of blood culture contamination during COVID-19 pandemic. A retrospective descriptive study. Am J Infect Control. 2021; 49(11):1359–1361. PMID: 34464662.
Article6. Abelenda-Alonso G, Puig-Asensio M, Jiménez-Martínez E, García-Lerma E, Hornero A, Gutiérrez C, et al. Impact of the coronavirus disease 2019 (COVID-19) pandemic on infection control practices in a university hospital. Infect Control Hosp Epidemiol. 2022; 44(1):135–138. PMID: 35591775.
Article7. Zhu NJ, Rawson TM, Mookerjee S, Price JR, Davies F, Otter J, et al. Changing patterns of bloodstream infections in the community and acute care across 2 coronavirus disease 2019 epidemic waves: a retrospective analysis using data linkage. Clin Infect Dis. 2022; 75(1):e1082–e1091. PMID: 34596212.
Article8. Sacchetti B, Travis J, Steed LL, Webb G. Effects of COVID-19 on blood culture contamination at a tertiary care academic medical center. Microbiol Spectr. 2022; 10(2):e0027722. PMID: 35352957.
Article9. WHO. WHO coronavirus (COVID-19) dashboard. Updated 2022. Accessed October 18, 2022. https://covid19.who.int/region/wpro/country/kr .10. Park SH. Personal protective equipment for healthcare workers during the COVID-19 pandemic. Infect Chemother. 2020; 52(2):165–182. PMID: 32618146.
Article11. Park DH, Lee E, Jung J, Kang CK, Song KH, Choe PG, et al. Changes in anxiety level and personal protective equipment use among healthcare workers exposed to COVID-19. J Korean Med Sci. 2022; 37(16):e126. PMID: 35470600.
Article12. Sanchez Novas D, Fernández MS, García Guzzo ME, Aguilar Avila LT, Domenech G, Bolla FE, et al. Self-contamination following removal of two personal protective equipment suits: a randomized, controlled, crossover simulation trial. J Hosp Infect. 2022; 119:155–162. PMID: 34606932.
Article13. Olaru ID, Ferrand RA, Magwenzi MT, Robertson V, Musenyereki V, Kranzer K. Risk assessment for rationalizing the use of personal protective equipment for SARS-CoV2 in healthcare settings with special focus on low- and middle-income settings. Clin Microbiol Infect. 2021; 27(2):169–171. PMID: 33190791.
Article14. Wilson SJ, Sellu D, Uy A, Jaffer MA. Subjective effects of double gloves on surgical performance. Ann R Coll Surg Engl. 1996; 78(1):20–22. PMID: 8659967.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Impact of Operating Room Nurses' Attitudes toward Wearing Personal Protective Equipment, Physical Discomfort, and Obsession with COVID-19 on Perceived Psychosocial Stress during the COVID-19 Pandemic: A Cross-sectional Study
- Personal Protective Equipment for Healthcare Workers during the COVID-19 Pandemic
- The Evaluation of Personal Protective Equipment Usage Habit of Mining Employees Using Structural Equation Modeling
- Personal Protective Equipment Availability and Utilization Among Interventionalists
- The Use of Personal Protective Equipment among Frontline Nurses in a Nationally Designated COVID-19 Hospital during the Pandemic