J Korean Med Sci.
2023 Jun;38(23):e178. 10.3346/jkms.2023.38.e178.
Incidence and Mortality Trends in Critically Ill Children: A Korean Population-Based Study
- Affiliations
-
- 1Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Pediatrics, Jeonbuk National University Children’s Hospital, Jeonju, Korea
- 3Department of Pediatrics, Chungnam National University Hospital, Daejeon, Korea
- 4Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2543870
- DOI: http://doi.org/10.3346/jkms.2023.38.e178
Abstract
- Background
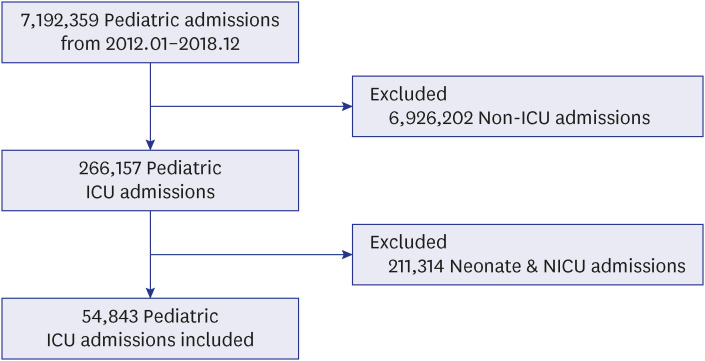
Monitoring mortality trends can help design ways to improve survival, but observation of national mortality trends in critically ill children is lacking for the Korean population Methods: We analyzed the incidence and mortality trends of children younger than 18 years admitted to an intensive care unit (ICU) from 2012 to 2018 using the Korean National Health Insurance database. Neonates and neonatal ICU admissions were excluded. Multivariable logistic regression analyses were performed to estimate the odds ratio of in-hospital mortality according to admission year. Trends in incidence and in-hospital mortality of subgroups according to admission department, age, presence of intensivists, admissions to pediatric ICU, mechanical ventilation, and use of vasopressors were evaluated.
Results
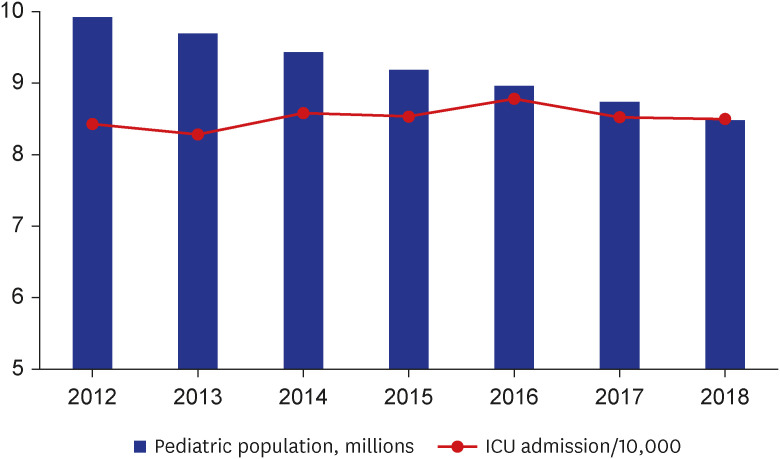
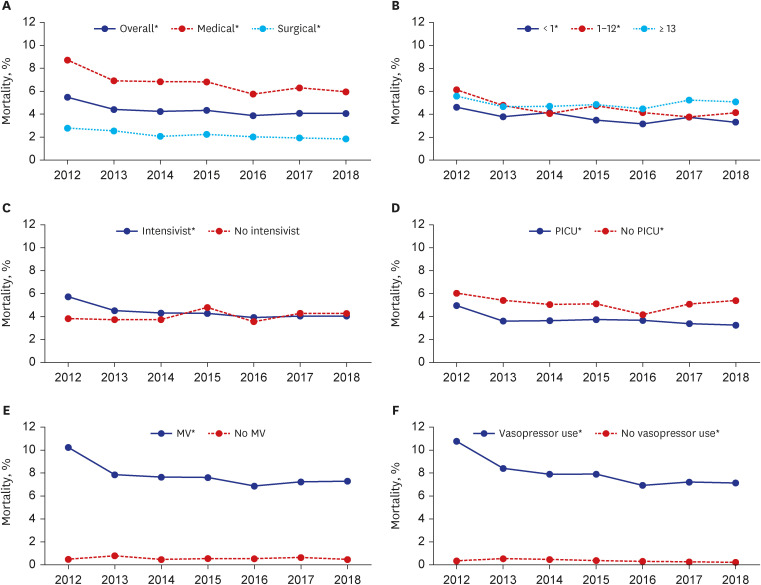
The overall mortality of critically ill children was 4.4%. There was a significant decrease in mortality from 5.5% in 2012 to 4.1% in 2018 (Pfor trend < 0.001). The incidence of ICU admission in children remained around 8.5/10,000 population years (Pfor trend = 0.069). In-hospital mortality decreased by 9.2% yearly in adjusted analysis (P < 0.001). The presence of dedicated intensivists (Pfor trend < 0.001, mortality decrease from 5.7% to 4.0%) and admission to pediatric ICU (Pfor trend < 0.001, mortality decrease from 5.0% to 3.2%) were associated with significant decreasing trends in mortality.
Conclusion
Mortality among critically ill children improved during the study period, and the improving trend was prominent in children with high treatment requirements. Varying mortality trends, according to ICU organizations, highlight that advances in medical knowledge should be supported structurally.
Keyword
Figure
Reference
-
1. Zimmerman JE, Kramer AA, Knaus WA. Changes in hospital mortality for United States intensive care unit admissions from 1988 to 2012. Crit Care. 2013; 17(2):R81. PMID: 23622086.
Article2. Moran JL, Bristow P, Solomon PJ, George C, Hart GK. Australian and New Zealand Intensive Care Society Database Management Committee (ADMC). Mortality and length-of-stay outcomes, 1993-2003, in the binational Australian and New Zealand intensive care adult patient database. Crit Care Med. 2008; 36(1):46–61. PMID: 18090383.
Article3. Sands R, Manning JC, Vyas H, Rashid A. Characteristics of deaths in paediatric intensive care: a 10-year study. Nurs Crit Care. 2009; 14(5):235–240. PMID: 19706074.
Article4. Burns JP, Sellers DE, Meyer EC, Lewis-Newby M, Truog RD. Epidemiology of death in the PICU at five U.S. teaching hospitals. Crit Care Med. 2014; 42(9):2101–2108. PMID: 24979486.
Article5. Gupta P, Gossett J, Rao Rettiganti M. 60: Trends in mortality rates in pediatric intensive care units in the United States from 2004 to 2015. Crit Care Med. 2018; 46(1):30.
Article6. Namachivayam P, Shann F, Shekerdemian L, Taylor A, van Sloten I, Delzoppo C, et al. Three decades of pediatric intensive care: Who was admitted, what happened in intensive care, and what happened afterward. Pediatr Crit Care Med. 2010; 11(5):549–555. PMID: 20124947.
Article7. Hannegård Hamrin T, Eksborg S. Risks for death after admission to pediatric intensive care (PICU)-a comparison with the general population. PLoS One. 2022; 17(10):e0265792. PMID: 36206205.
Article8. Feudtner C, Silveira MJ, Christakis DA. Where do children with complex chronic conditions die? Patterns in Washington State, 1980-1998. Pediatrics. 2002; 109(4):656–660. PMID: 11927711.
Article9. Tilford JM, Roberson PK, Lensing S, Fiser DH. Differences in pediatric ICU mortality risk over time. Crit Care Med. 1998; 26(10):1737–1743. PMID: 9781733.
Article10. Gemke RJ. Centralisation of paediatric intensive care to improve outcome. Lancet. 1997; 349(9060):1187–1188. PMID: 9130935.
Article11. Ramnarayan P, Thiru K, Parslow RC, Harrison DA, Draper ES, Rowan KM. Effect of specialist retrieval teams on outcomes in children admitted to paediatric intensive care units in England and Wales: a retrospective cohort study. Lancet. 2010; 376(9742):698–704. PMID: 20708255.
Article12. Kim DY, Lee MH, Lee SY, Yang BR, Kim HA. Survival rates following medical intensive care unit admission from 2003 to 2013: an observational study based on a representative population-based sample cohort of Korean patients. Medicine (Baltimore). 2019; 98(37):e17090. PMID: 31517831.13. Lee JW, Youn SW, Shin YS, Park SI, Kim DC, Koh Y. Major obstacles to implement a full-time intensivist in Korean adult ICUs: a questionnaire survey. Korean J Crit Care Med. 2016; 31(2):111–117.
Article14. Han ER, Chung EK. The perception of medical residents and faculty members on resident duty hour regulation. Korean J Med Educ. 2020; 32(1):67–72. PMID: 32130852.
Article15. Jung JH, Sol IS, Kim MJ, Kim YH, Kim KW, Sohn MH. Validation of pediatric index of mortality 3 for predicting mortality among patients admitted to a pediatric intensive care unit. Acute Crit Care. 2018; 33(3):170–177. PMID: 31723881.
Article16. Lee OJ, Jung M, Kim M, Yang HK, Cho J. Validation of the pediatric index of mortality 3 in a single pediatric intensive care unit in Korea. J Korean Med Sci. 2017; 32(2):365–370. PMID: 28049251.
Article17. Jung M, Park H, Kang D, Park J, Jeon K, Chung CR, et al. Age-specific distribution of diagnosis and outcomes of children admitted to ICUs: a population-based cohort study. Pediatr Crit Care Med. 2019; 20(7):e301–e310. PMID: 31162369.18. Shime N, Kawasaki T, Saito O, Akamine Y, Toda Y, Takeuchi M, et al. Incidence and risk factors for mortality in paediatric severe sepsis: results from the national paediatric intensive care registry in Japan. Intensive Care Med. 2012; 38(7):1191–1197. PMID: 22527068.
Article19. Quan H, Moskal L, Forster AJ, Brien S, Walker R, Romano PS, et al. International variation in the definition of ‘main condition’ in ICD-coded health data. Int J Qual Health Care. 2014; 26(5):511–515. PMID: 24990594.
Article20. Choi J, Choi AY, Park E, Moon S, Son MH, Cho J. Trends in incidences and survival rates in pediatric in-hospital cardiopulmonary resuscitation: a Korean population-based study. J Am Heart Assoc. 2023; 12(3):e028171. PMID: 36695322.
Article21. Ibiebele I, Algert CS, Bowen JR, Roberts CL. Pediatric admissions that include intensive care: a population-based study. BMC Health Serv Res. 2018; 18(1):264. PMID: 29631570.
Article22. Killien E, Hartman M, Watson RS. O055/#336: Epidemiology of intensive care admissions in children in the United States, 2010 and 2015. Pediatr Crit Care Med. 2021; 22(Supplement 1 3S):34.
Article23. Siddiqui NU, Ashraf Z, Jurair H, Haque A. Mortality patterns among critically ill children in a pediatric intensive care unit of a developing country. Indian J Crit Care Med. 2015; 19(3):147–150. PMID: 25810609.
Article24. El Halal MG, Barbieri E, Filho RM, Trotta EA, Carvalho PR. Admission source and mortality in a pediatric intensive care unit. Indian J Crit Care Med. 2012; 16(2):81–86. PMID: 22988362.
Article25. Jung M, Park H, Kang D, Park E, Jeon K, Chung CR, et al. The effect of bed-to-nurse ratio on hospital mortality of critically ill children on mechanical ventilation: a nationwide population-based study. Ann Intensive Care. 2020; 10(1):159. PMID: 33257997.
Article26. Coulthard MG, Varghese V, Harvey LP, Gillen TC, Kimble RM, Ware RS. A review of children with severe trauma admitted to pediatric intensive care in Queensland, Australia. PLoS One. 2019; 14(2):e0211530. PMID: 30730910.
Article27. Fiser DH, Tilford JM, Roberson PK. Relationship of illness severity and length of stay to functional outcomes in the pediatric intensive care unit: a multi-institutional study. Crit Care Med. 2000; 28(4):1173–1179. PMID: 10809301.
Article28. Shann F, Pearson G. Paediatric intensive care - specialisation reduces mortality. Anaesthesia. 1999; 54(8):809–810. PMID: 10460538.
Article29. Peltoniemi OM, Rautiainen P, Kataja J, Ala-Kokko T. Pediatric Intensive care in PICUs and adult ICUs: a 2-year cohort study in Finland. Pediatr Crit Care Med. 2016; 17(2):e43–e49. PMID: 26669639.30. Carson SS, Stocking C, Podsadecki T, Christenson J, Pohlman A, MacRae S, et al. Effects of organizational change in the medical intensive care unit of a teaching hospital: a comparison of ‘open’ and ‘closed’ formats. JAMA. 1996; 276(4):322–328. PMID: 8656546.
Article31. Li TC, Phillips MC, Shaw L, Cook EF, Natanson C, Goldman L. On-site physician staffing in a community hospital intensive care unit. Impact on test and procedure use and on patient outcome. JAMA. 1984; 252(15):2023–2027. PMID: 6481908.
Article32. Pollack MM, Katz RW, Ruttimann UE, Getson PR. Improving the outcome and efficiency of intensive care: the impact of an intensivist. Crit Care Med. 1988; 16(1):11–17. PMID: 3338276.33. Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004; 32(3):858–873. PMID: 15090974.
Article34. Marra A, Ely EW, Pandharipande PP, Patel MB. The ABCDEF bundle in critical care. Crit Care Clin. 2017; 33(2):225–243. PMID: 28284292.
Article35. Acute Respiratory Distress Syndrome Network. Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342(18):1301–1308. PMID: 10793162.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Value of the Total Lymphocyte Count as a Risk Index of Hospital Infection in Critically Ill Patients
- Prehospital transport of critically ill children via 119 emergency medical service providers: problems and improvement plan
- APACHE II Score and Multiple Organ Failure Score as Predictors of Mortality Rate of Critically Ill Patients
- Trend of Intensive Care Unit Admission in Neurology-Neurosurgery Adult Patients in South Korea : A Nationwide Population-Based Cohort Study
- Interfacility transport of critically ill children