J Korean Neurosurg Soc.
2023 Jul;66(4):446-455. 10.3340/jkns.2022.0200.
Role of Adjunctive Tranexamic Acid in Facilitating Resolution of Chronic Subdural Hematoma after Surgery
- Affiliations
-
- 1Department of Neurosurgery, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea
- KMID: 2543536
- DOI: http://doi.org/10.3340/jkns.2022.0200
Abstract
Objective
: Chronic subdural hematoma (CSDH) is a common neurosurgical disease and generally treated with burr-hole surgery alone. Tranexamic acid (TXA) is an antifibrinolytic agent that potentially reduces recurrence rates and the residual hematoma volume. However, the role of postoperative TXA medication remains unclear to date. This study aimed to verify the effectiveness of adjunctive TXA in the view of early hematoma resolution.
Methods
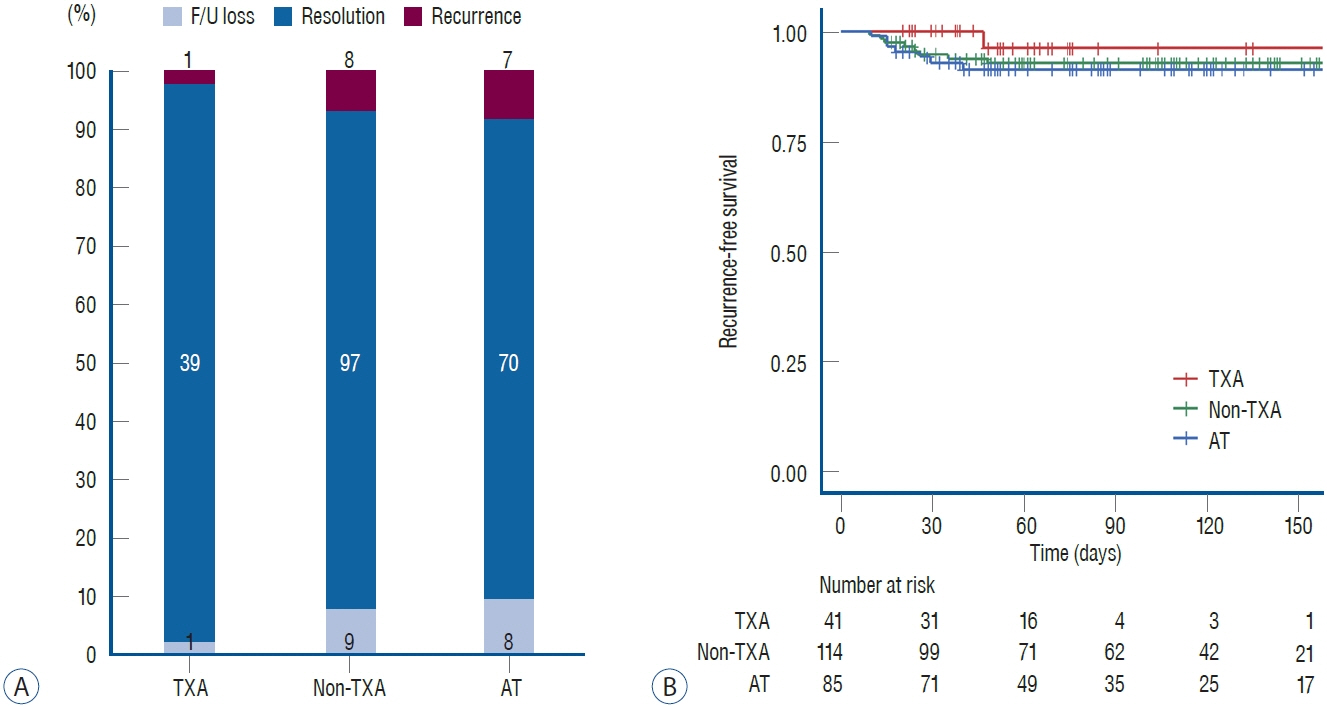
: Between January 2018 and September 2021, patients with CSDH who underwent burr-hole trephination in a single tertiary institute were reviewed. The study population was divided into three groups, TXA, non-TXA, and antithrombotics (AT) groups, according to the medical history of cardio-cerebrovascular disease and TXA administration. The primary endpoint was CSDH recurrence, defined as re-appearance or re-accumulation of CSDH requiring neurosurgical interventions. The secondary outcome was CSDH resolution, defined as complete or near-complete resorption of the CSDH. The CSDH resolution time and serial changes of hematoma thickness were also investigated.
Results
: A total of 240 patients was included in the analysis consisting of 185 male and 55 female, with a median age of 74 years. During the median imaging follow-up period of 75 days, 222 patients were reached to the primary or secondary endpoint. TXA was administered as an adjunctive therapy in 41 patients (TXA group, 16.9%) while 114 patients were included in the non-TXA group (47.9%) and 85 were in the AT group. The recurrence rate was the lowest in the TXA group (2.4%), followed by non-TXA (7.0%) and AT (8.2%) groups. However, there was no statistical significance due to the small number of patients with recurrence. CSDH resolution was achieved in 206 patients, and the median estimated time to resolution was significantly faster in the TXA group (p<0.001). Adjunctive TXA administration was a significant positive factor for achieving CSDH resolution (p<0.001). The hematoma thickness was comparable among the three groups at the initial time and after surgery. However, CSDH thickness in the TXA group decreased abruptly in a month and showed a significant difference from that in the other groups (p<0.001). There was no TXA-related adverse event.
Conclusion
: The adjunctive use of TXA after CSDH surgery significantly facilitated the resorption of residual CSDH and resulted in the early CSDH resolution. Adjunctive TXA may be an effective treatment option to reduce recurrence by enhancing CSDH resolution in the selective patients.
Figure
Reference
-
References
1. Cheriyan T, Maier SP 2nd, Bianco K, Slobodyanyuk K, Rattenni RN, Lafage V, et al. Efficacy of tranexamic acid on surgical bleeding in spine surgery: a meta-analysis. Spine J. 15:752–761. 2015.
Article2. Cofano F, Pesce A, Vercelli G, Mammi M, Massara A, Minardi M, et al. Risk of recurrence of chronic subdural hematomas after surgery: a multicenter observational cohort study. Front Neurol. 11:560269. 2020.
Article3. de Faria JL, da Silva Brito J, Costa E Silva LT, Kilesse CTSM, de Souza NB, Pereira CU, et al. Tranexamic acid in neurosurgery: a controversy indication-review. Neurosurg Rev. 44:1287–1298. 2021.
Article4. Edlmann E, Giorgi-Coll S, Whitfield PC, Carpenter KLH, Hutchinson PJ. Pathophysiology of chronic subdural haematoma: inflammation, angiogenesis and implications for pharmacotherapy. J Neuroinflammation. 14:108. 2017.
Article5. Edlmann E, Holl DC, Lingsma HF, Bartek J Jr, Bartley A, Duerinck J, et al. Systematic review of current randomised control trials in chronic subdural haematoma and proposal for an international collaborative approach. Acta Neurochir (Wien). 162:763–776. 2020.
Article6. Holl DC, Volovici V, Dirven CMF, Peul WC, van Kooten F, Jellema K, et al. Pathophysiology and nonsurgical treatment of chronic subdural hematoma: from past to present to future. World Neurosurg. 116:402–411.e2. 2018.
Article7. Huang J, Gao C, Dong J, Zhang J, Jiang R. Drug treatment of chronic subdural hematoma. Expert Opin Pharmacother. 21:435–444. 2020.
Article8. Iorio-Morin C, Blanchard J, Richer M, Mathieu D. Tranexamic acid in chronic subdural hematomas (TRACS): study protocol for a randomized controlled trial. Trials. 17:235. 2016.
Article9. Kageyama H, Toyooka T, Tsuzuki N, Oka K. Nonsurgical treatment of chronic subdural hematoma with tranexamic acid. J Neurosurg. 119:332–337. 2013.
Article10. Kolias AG, Chari A, Santarius T, Hutchinson PJ. Chronic subdural haematoma: modern management and emerging therapies. Nat Rev Neurol. 10:570–578. 2014.
Article11. Kutty RK, Peethambaran AK, Anilkumar M. Conservative treatment of chronic subdural hematoma in HIV-associated thrombocytopenia with tranexamic acid. J Int Assoc Provid AIDS Care. 16:211–214. 2017.
Article12. Lee KS. How to treat chronic subdural hematoma? Past and now. J Korean Neurosurg Soc. 62:144–152. 2019.
Article13. Lodewijkx R, Immenga S, van den Berg R, Post R, Westerink LG, Nabuurs RJA, et al. Tranexamic acid for chronic subdural hematoma. Br J Neurosurg. 35:564–569. 2021.
Article14. Mehta V, Harward SC, Sankey EW, Nayar G, Codd PJ. Evidence based diagnosis and management of chronic subdural hematoma: a review of the literature. J Clin Neurosci. 50:7–15. 2018.
Article15. Mikkelsen R, Anker-Møller T, Hvas AM, Sunde N. A case of tranexamic acid as adjunctive treatment for chronic subdural hematoma with multiple recurrences. Am J Case Rep. 18:995–999. 2017.
Article16. Nakaguchi H, Tanishima T, Yoshimasu N. Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg. 95:256–262. 2001.
Article17. Ng W, Jerath A, Wąsowicz M. Tranexamic acid: a clinical review. Anaesthesiol Intensive Ther. 47:339–350. 2015.
Article18. Ngaage DL, Bland JM. Lessons from aprotinin: is the routine use and inconsistent dosing of tranexamic acid prudent? Meta-analysis of randomised and large matched observational studies. Eur J Cardiothorac Surg. 37:1375–1383. 2010.
Article19. Oh HJ, Seo Y, Choo YH, Kim YI, Kim KH, Kwon SM, et al. Clinical characteristics and current managements for patients with chronic subdural hematoma : a retrospective multicenter pilot study in the Republic of Korea. J Korean Neurosurg Soc. 65:255–268. 2022.
Article20. Oka K, Toyooka T, Kageyama H, Tsuzuki N. Effectiveness of antifibrinolytic therapy after surgery for chronic subdural hematoma. J Neurosurg. 119:A550. 2013.21. Qiu S, Zhuo W, Sun C, Su Z, Yan A, Shen L. Effects of atorvastatin on chronic subdural hematoma: a systematic review. Medicine (Baltimore). 96:e7290. 2017.22. Ryu SM, Yeon JY, Kong DS, Hong SC. Risk of recurrent chronic subdural hematoma associated with early warfarin resumption: a matched cohort study. World Neurosurg. 120:e855–e862. 2018.
Article23. Scerrati A, Visani J, Ricciardi L, Dones F, Rustemi O, Cavallo MA, et al. To drill or not to drill, that is the question: nonsurgical treatment of chronic subdural hematoma in the elderly. A systematic review. Neurosurg Focus. 49:E7. 2020.
Article24. Soleman J, Nocera F, Mariani L. The conservative and pharmacological management of chronic subdural haematoma. Swiss Med Wkly. 147:w14398. 2017.25. Stary JM, Hutchins L, Vega RA. Tranexamic acid for recurring subdural hematomas following surgical evacuation: a clinical case series. J Neurol Surg A Cent Eur Neurosurg. 77:422–426. 2016.
Article26. Tanweer O, Frisoli FA, Bravate C, Harrison G, Pacione D, Kondziolka D, et al. Tranexamic acid for treatment of residual subdural hematoma after bedside twist-drill evacuation. World Neurosurg. 91:29–33. 2016.
Article27. Wan KR, Qiu L, Saffari SE, Khong WXL, Ong JCL, See AA, et al. An open label randomized trial to assess the efficacy of tranexamic acid in reducing post-operative recurrence of chronic subdural haemorrhage. J Clin Neurosci. 82:147–154. 2020.
Article28. Wang X, Song J, He Q, You C. Pharmacological treatment in the management of chronic subdural hematoma. Front Aging Neurosci. 13:684501. 2021.
Article29. Workewych A, Callum J, Saarela O, Montanera W, Cusimano MD. Tranexamic acid in the treatment of residual chronic subdural hematoma: a single-centre, randomized controlled trial (TRACE). J Neurotrauma. 35:A244–A245. 2018.30. Xu FF, Chen JH, Leung GK, Hao SY, Xu L, Hou ZG, et al. Quantitative computer tomography analysis of post-operative subdural fluid volume predicts recurrence of chronic subdural haematoma. Brain Inj. 28:1121–1126. 2014.31. Yamada T, Natori Y. Prospective study on the efficacy of orally administered tranexamic acid and goreisan for the prevention of recurrence after chronic subdural hematoma burr hole surgery. World Neurosurg. 134:e549–e553. 2020.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous Resolution of Chronic Subdural Hematoma : Close Observation as a Treatment Strategy
- Chronic Subdural Hematoma Superimposed on Posttraumatic Subdural Hygroma: A Report of Three Cases
- Bilateral Acute Subdural Hematoma Following Evacuation of Chronic Subdural Hematoma
- Spontaneously Rapid Resolution of Acute Subdural Hemorrhage with Severe Midline Shift
- Spontaneous Resolution of Chronic Subdural Hematoma in Children: Case Report