J Cerebrovasc Endovasc Neurosurg.
2023 Jun;25(2):132-142. 10.7461/jcen.2023.E2022.10.009.
Discontinuation of antiplatelet therapy after stent-assisted coil embolization for cerebral aneurysms
- Affiliations
-
- 1Department of Neurosurgery, CHA Bundang Medical Center, CHA University, School of Medicine, Seongnam, Korea
- KMID: 2543509
- DOI: http://doi.org/10.7461/jcen.2023.E2022.10.009
Abstract
Objective
Dual antiplatelet therapy (DAPT) is usually temporarily used after stent-assisted coil embolization (SACE), and is commonly converted to mono antiplatelet therapy (MAPT) for indefinitely. In this study, we aimed to find the possibility of discontinuing MAPT, and to determine the proper period of DAPT use.
Methods
We used the Standard Sample Cohort DB dataset from the National Health Insurance Sharing Service. Among approximately 1 million people in the dataset, SACE was performed in 214 patients whose data this study analyzed. The relationship between discontinuation of antiplatelet therapy and intracranial hemorrhage or cerebral infarction was analyzed using multiple logistic regression, considering all confounding variables. The survival rate according to the continuation of antiplatelet therapy was obtained using Kaplan-Meier analysis, and the difference in survival rate according to the continuation of antiplatelet therapy was verified using the log-rank test. The hazard ratio according to continuation of antiplatelet therapy was obtained using the Cox proportional hazards model. The analysis was conducted by applying the same statistical method to the duration of DAPT use.
Results
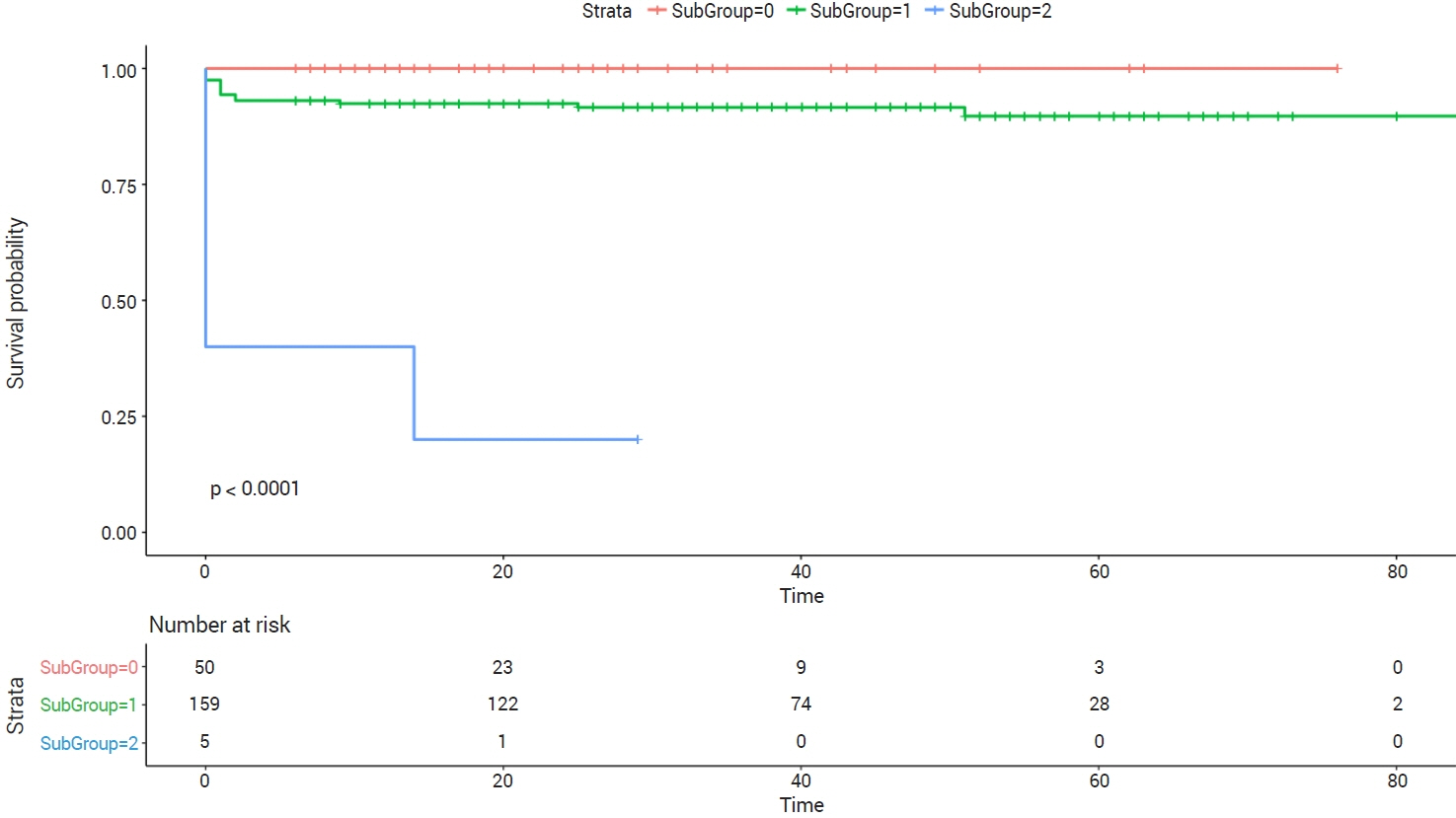
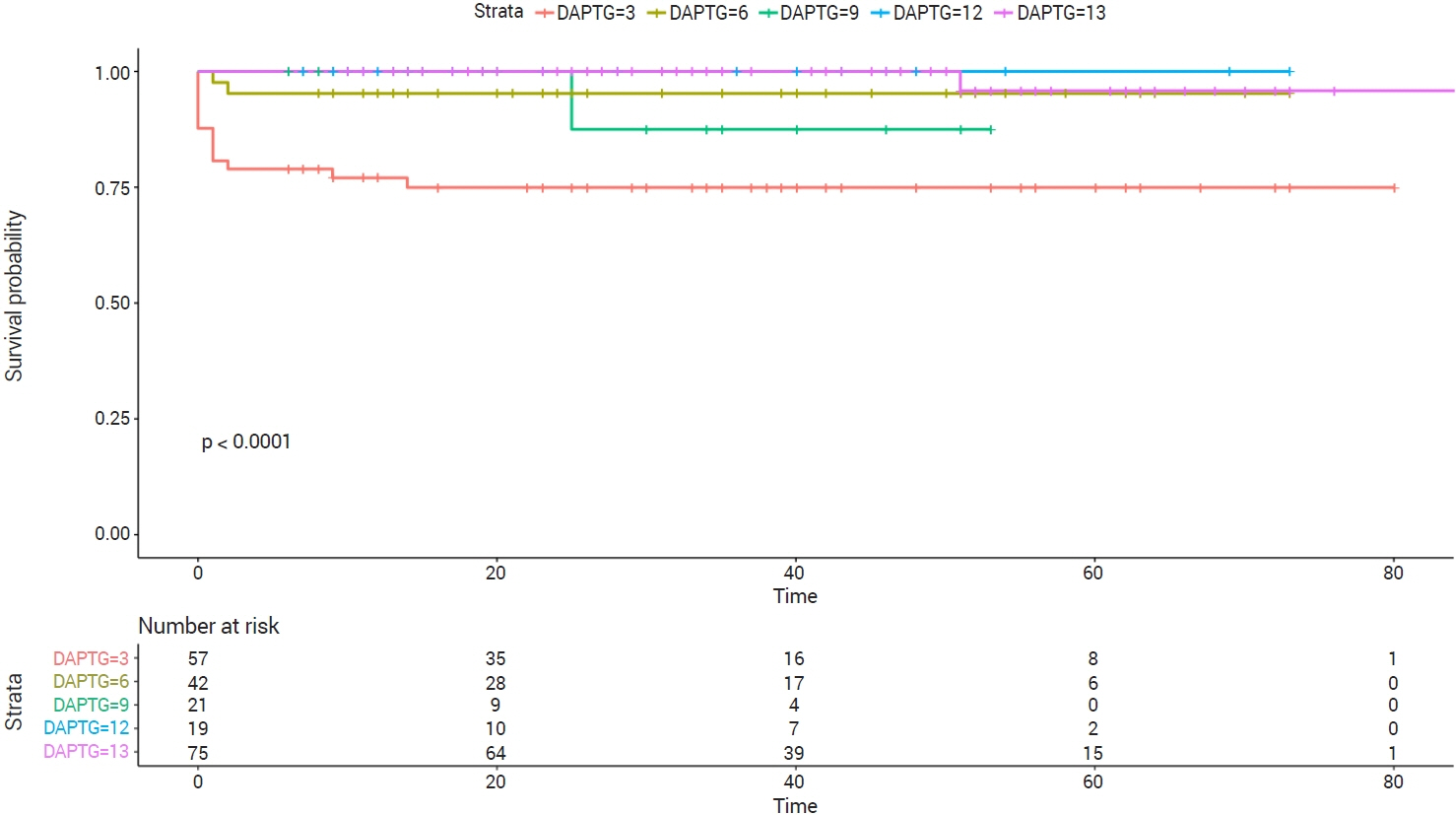
Among 214 patients who underwent SACE, 50, 159 and five patients continued, discontinued and did not use antiplatelet therapy (except at the time of procedure), respectively. In multiple logistic regression analysis, discontinuation of antiplatelet agents (including aspirin) and the period of DAPT use did not affect the occurrence of intracranial hemorrhage or cerebral infarction, considering various confounding factors. In the survival analysis according to the continuation of antiplatelet agents, patients who continued to use antiplatelet agents had a higher survival rate than those in other groups (p=0.00). The survival rate was higher in the rest of the group than in the group that received DAPT for three months (p=0.00).
Conclusions
Continuation of antiplatelet agents or the period of DAPT use did not affect the occurrence of intracranial hemorrhage or cerebral infarction. Considering the survival rate, it would be better to maintain at least three months of antiplatelet therapy and it might be recommended to continue DAPT use for 12 months.
Figure
Reference
-
1. Bendok BR, Parkinson RJ, Hage ZA, Adel JG, Gounis MJ. The effect of vascular reconstruction device-assisted coiling on packing density, effective neck coverage, and angiographic outcome: an in vitro study. Neurosurgery. 2007; Oct. 61(4):835–40. discussion 840-1.2. Bodily KD, Cloft HJ, Lanzino G, Fiorella DJ, White PM, Kallmes DF. Stent-assisted coiling in acutely ruptured intracranial aneurysms: a qualitative, systematic review of the literature. AJNR Am J Neuroradiol. 2011; Aug. 32(7):1232–6.
Article3. Chalouhi N, Jabbour P, Singhal S, Drueding R, Starke RM, Dalyai RT, et al. Stent-assisted coiling of intracranial aneurysms: predictors of complications, recanalization, and outcome in 508 cases. Stroke. 2013; May. 44(5):1348–53.4. Cho YD, Lee JY, Seo JH, Lee SJ, Kang HS, Kim JE, et al. Does stent implantation improve the result of repeat embolization in recanalized aneurysms? Neurosurgery. 2012; Dec. 71(2 Suppl Operative):ons253–9. discussion ons259.
Article5. García-Rodríguez LA, Gaist D, Morton J, Cookson C, González-Pérez A. Antithrombotic drugs and risk of hemorrhagic stroke in the general population. Neurology. 2013; Aug. 81(6):566–74.
Article6. García Rodríguez LA, Martín-Pérez M, Hennekens CH, Rothwell PM, Lanas A. Bleeding risk with long-term lowdose aspirin: a systematic review of observational studies. PLoS One. 2016; Aug. 11(8):e0160046.
Article7. Goto S, Izumi T, Nishihori M, Imai T, Araki Y, Kanamori F, et al. Antiplatelet therapy discontinuation after stent-assisted coil embolization for intracranial aneurysms: a single-center, long-term, retrospective, observational study. J Neurosurg. 2022; Aug. 1–8.
Article8. Hart RG, Halperin JL, McBride R, Benavente O, Man-SonHing M, Kronmal RA. Aspirin for the primary prevention of stroke and other major vascular events: meta-analysis and hypotheses. Arch Neurol. 2000; Mar. 57(3):326–32.
Article9. He J, Whelton PK, Vu B, Klag MJ. Aspirin and risk of hemorrhagic stroke: a meta-analysis of randomized controlled trials. Jama. 1998; Dec. 280(22):1930–5.10. Hetts SW, Turk A, English JD, Dowd CF, Mocco J, Prestigiacomo C, et al. Stent-assisted coiling versus coiling alone in unruptured intracranial aneurysms in the matrix and platinum science trial: safety, efficacy, and mid-term outcomes. AJNR Am J Neuroradiol. 2014; Apr. 35(4):698–705.
Article11. Hong N, Cho YD, Kim HS, Pang CH, Yoo DH, Kim JE, et al. Is it safe to discontinue antiplatelet medication after stent-assisted coil embolization? If so, when is the best time? J Neuroradiol. 2022; Mar. S0150-9861(22)00105-5.
Article12. Hwang G, Kim JG, Song KS, Lee YJ, Villavicencio JB, Suroto NS, et al. Delayed ischemic stroke after stent-assisted coil placement in cerebral aneurysm: characteristics and optimal duration of preventative dual antiplatelet therapy. Radiology. 2014; Oct. 273(1):194–201.
Article13. Kim KS, Fraser JF, Grupke S, Cook AM. Management of antiplatelet therapy in patients undergoing neuroendovascular procedures. J Neurosurg. 2018; Oct. 129(4):890–905.
Article14. Kim TG, Yu S. Big data analysis of the risk of intracranial hemorrhage in Korean populations taking low-dose aspirin. J Stroke Cerebrovasc Dis. 2021; Aug. 30(8):105917.
Article15. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021; Jul. 52(7):e364–467.
Article16. McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med. 2006; Aug. 119(8):624–38.
Article17. Mocco J, Fargen KM, Albuquerque FC, Bendok BR, Boulos AS, Carpenter JS, et al. Delayed thrombosis or stenosis following enterprise-assisted stent-coiling: is it safe? Midterm results of the interstate collaboration of enterprise stent coiling. Neurosurgery. 2011; Oct. 69(4):908–13. discussion 913-4.
Article18. Oxley TJ, Dowling RJ, Mitchell PJ, Davis S, Yan B. Antiplatelet resistance and thromboembolic complications in neurointerventional procedures. Front Neurol. 2011; Dec. 2:83.
Article19. Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ, et al. Stent-assisted coiling of intracranial aneurysms: clinical and angiographic results in 216 consecutive aneurysms. Stroke. 2010; Jan. 41(1):110–5.20. Shoda K, Enomoto Y, Egashira Y, Kinoshita T, Mizutani D, Iwama T. Long-term complications after stent assist coiling dependent on clopidogrel response. BMC Neurol. 2021; Jun. 21(1):247.
Article21. Thrift AG, McNeil JJ, Forbes A, Donnan GA; Melbourne Risk Factor Study (MERFS) Group. Risk factors for cerebral hemorrhage in the era of well-controlled hypertension. Stroke. 1996; Nov. 27(11):2020–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two cases of acute ischemic stroke associated with strut exposure in the cerebral artery lumen after stent-assisted coil embolization
- Stent-assisted Coil Embolization of Cerebral Aneurysms: Review Article
- Feasibility of single antiplatelet therapy after stent assisted coiling for ruptured intracranial aneurysms
- Selective Temporary Stent-Assisted Coil Embolization for Intracranial Wide-Necked Small Aneurysms Using Solitaire AB Retrievable Stent
- A Complicated Case of Endovascular Stent Assisted Coil Embolization of an Aneurysm