Korean J Gastroenterol.
2023 Jun;81(6):270-275. 10.4166/kjg.2023.036.
Rare Complication of Strongyloidiasis in Vietnam: A Case of Venous Thromboembolism and Duodenal Obstruction
- Affiliations
-
- 1Department of Internal Medicine, Faculty of Medicine University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam
- 2Department of Gastroenterology, Cho Ray Hospital, Ho Chi Minh City, Vietnam
- 3Department of Pathology Cho Ray Hospital, Ho Chi Minh City, Vietnam
- KMID: 2543448
- DOI: http://doi.org/10.4166/kjg.2023.036
Abstract
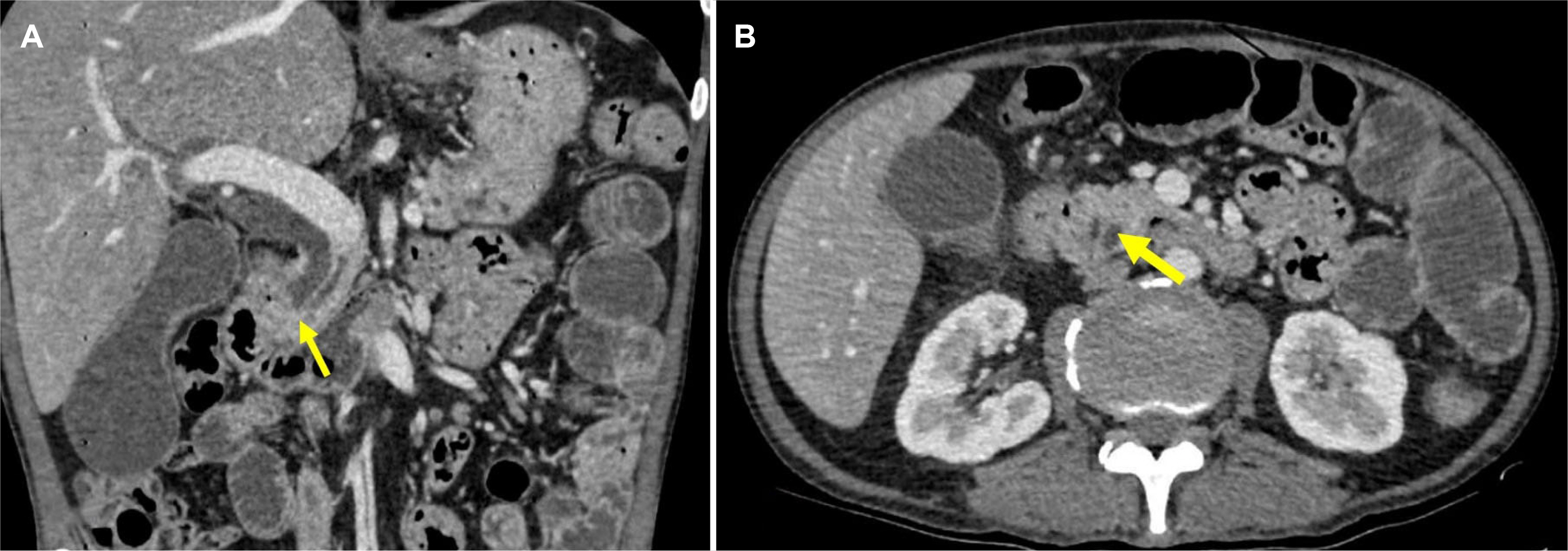
- Strongyloidiasis, a chronic helminth infection caused by the parasitic nematode Strongyloides stercoralis, has various clinical manifestations. Although rare, duodenal obstructions and venous thromboembolism are possible complications of strongyloidiasis. This paper presents the case of a 47-year-old Vietnamese male with a history of right lower limb edema, anorexia, nausea, vomiting, diarrhea, and abdominal discomfort lasting for four months. Venous Doppler ultrasound detected a thrombus in the right femoral vein, while an abdominal CT scan revealed a mass lesion suggestive of a lower bile duct tumor. Esophageogastroduodenoscopy showed a friable duodenal cap mucosa with multiple ulcers and edematous mucosa of the second part of the duodenum that caused a partial lumen obstruction. The final histological examination of the biopsy specimen revealed chronic duodenitis with larvae consistent with Strongyloides stercoralis. The patient was treated with Ivermectin for two weeks and anticoagulation therapy for three months. After treatment and a six-month follow-up, the patient's gastrointestinal symptoms and leg swelling resolved completely. This is the first documented case of a patient in Vietnam with strongyloidiasis who presented with venous thromboembolism and duodenal obstruction. (Korean J Gastroenterol 2023;81:270-275)
Figure
Reference
-
1. Juchems MS, Niess JH, Leder G, et al. 2008; Strongyloides stercoralis: a rare cause of obstructive duodenal stenosis. Digestion. 77:141–144. DOI: 10.1159/000128597. PMID: 18446028.
Article2. Malézieux-Picard A, Saint-Paul MC, Dellamonica J, et al. 2017; Severe intestinal obstruction due to Strongyloides stercoralis in a pregnant woman. Med Mal Infect. 47:429–431. DOI: 10.1016/j.medmal.2017.05.007. PMID: 28651833.
Article3. Yazdanpanah F, Saba H, Rahmani R, Schreiber ZJ, Hindy P. 2020; Strongyloides hyperinfection presenting as a gastric outlet obstruction. Cureus. 12:e6603. DOI: 10.7759/cureus.6603. PMID: 32064185. PMCID: PMC7008763.
Article4. Cruz RJ Jr, Vincenzi R, Ketzer BM. 2010; Duodenal obstruction - an unusual presentation of Strongyloides stercoralis enteritis: a case report. World J Emerg Surg. 5:23. DOI: 10.1186/1749-7922-5-23. PMID: 20698992. PMCID: PMC2925357.
Article5. Cohen J, Spry CJ. 1979; Strongyloides stercoralis infection and small intestinal lymphoma. Parasite Immunol. 1:167–178. DOI: 10.1111/j.1365-3024.1979.tb00704.x. PMID: 317839.
Article6. Zeitler K, Jariwala R, Restrepo-Jaramillo R, et al. 2018; Successful use of subcutaneous ivermectin for the treatment of Strongyloides stercoralis hyperinfection in the setting of small bowel obstruction and paralytic ileus in the immunocompromised population. BMJ Case Rep. 2018:bcr2017223138. DOI: 10.1136/bcr-2017-223138. PMID: 29866667. PMCID: PMC5990086.7. Patra AA, Nath P, Pati GK, et al. 2019; Strongyloides infection presenting as proximal small intestinal obstruction. ACG Case Rep J. 6:e00124. DOI: 10.14309/crj.0000000000000124. PMID: 31616778. PMCID: PMC6722340.
Article8. Rothe K, Katchanov J, Schneider J, et al. 2020; Strongyloides stercoralis hyperinfection syndrome presenting as mechanical ileus after short-course oral steroids for chronic obstructive pulmonary disease (COPD) exacerbation. Parasitol Int. 76:102087. DOI: 10.1016/j.parint.2020.102087. PMID: 32087332.
Article9. Aslam A, Barlas U, Yassan LJ, Lodhi M. 2022; An unusual case of gastric outlet obstruction and melena. Clin J Gastroenterol. 15:374–380. DOI: 10.1007/s12328-021-01584-3. PMID: 35064555.
Article10. Beltrán Rosel A, Sanjoaquín Conde I, Pérez Muñoz A, Alcalá PM, Marta CB, Irigoyen von Sierakowski A. 2020; Strongyloides stercoralis: a rare and severe presentation in a pregnant woman. New Microbiol. 43:44–46. PMID: 31814031.11. Kakati B, Dang S, Heif M, Caradine K, McKnight W, Aduli F. 2011; Strongyloides duodenitis: case report and review of literature. J Natl Med Assoc. 103:60–63. DOI: 10.1016/s0027-9684(15)30246-7. PMID: 21329250.
Article12. Kishimoto K, Hokama A, Hirata T, et al. 2008; Endoscopic and histopathological study on the duodenum of Strongyloides stercoralis hyperinfection. World J Gastroenterol. 14:1768–1773. DOI: 10.3748/wjg.14.1768. PMID: 18350608. PMCID: PMC2695917.
Article13. Franco AR, Mendo R, Figueiredo P, Albuquerque AC. An unusual cause of duodenal obstruction: Watch your feet! GE Port J Gastroenterol. 2022; Oct. 21. doi: https://doi.org/10.1159/000526040. DOI: 10.1159/000526040.
Article14. Zyngier FR, Lemme A, Pereira EG, Leal BB, Liberal MH. 1983; Surgical perpetuation of serious infection with Strongyloides stercoralis. Trans R Soc Trop Med Hyg. 77:425. DOI: 10.1016/0035-9203(83)90182-7. PMID: 6414126.
Article15. Baaten GG, Sonder GJ, van Gool T, Kint JA, van den Hoek A. 2011; Travel-related schistosomiasis, strongyloidiasis, filariasis, and toxocariasis: the risk of infection and the diagnostic relevance of blood eosinophilia. BMC Infect Dis. 11:84. DOI: 10.1186/1471-2334-11-84. PMID: 21466667. PMCID: PMC3079652.
Article16. Hindy P, Parvin R, Hanna K, Gress F. 2011; Strongyloidiasis presenting as duodenal obstruction in a patient infected with human T-cell lymphotropic virus type 1. Gastrointest Endosc. 74:439–441. DOI: 10.1016/j.gie.2010.11.035. PMID: 21704987.
Article17. Li W, Chattree A. 2019; Small-bowel obstruction due to Strongyloides stercoralis infection. Clin Gastroenterol Hepatol. 17:A41–A42. DOI: 10.1016/j.cgh.2018.03.017. PMID: 29559358.
Article18. Martyn E, Gration B, Somasundaram C, Chiodini PL. 2019; Strongyloides, HTLV-1 and small bowel obstruction. BMJ Case Rep. 12:e232461. DOI: 10.1136/bcr-2019-232461. PMID: 31822534. PMCID: PMC6904184.19. Harish K, Sunilkumar R, Varghese T, Feroze M. 2005; Strongyloidiasis presenting as duodenal obstruction. Trop Gastroenterol. 26:201–202. DOI: 10.1016/j.gie.2010.11.035. PMID: 16737052.20. Waters M, Krajden S, Kim C, et al. 2019; Case report: Two cases of strongyloidiasis presenting with thrombotic events. Am J Trop Med Hyg. 101:418–421. DOI: 10.4269/ajtmh.19-0347. PMID: 31218995. PMCID: PMC6685577.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Annular Pancreas with a Duodenal Web: a Rare Presentation with Simultaneous Intrinsic and Extrinsic Duodenal Obstruction
- Clinical Year in Review of Venous Thromboembolism
- A case of strongyloidiasis accompanied by duodenal ulcer
- Duodenal Bezoar: A Rare Cause of Acute Pancreatitis
- Sciatic Nerve Palsy Due to Hematoma Following Anticoagulation Therapy for Prevention of Venous Thromboembolism after Total Hip Arthroplasty - A Case Report -