Korean J Gastroenterol.
2023 Jun;81(6):265-269. 10.4166/kjg.2023.026.
Five-year Progress of Gastric MALT Lymphoma Presenting as Gastric Outlet Obstruction
- Affiliations
-
- 1Departments of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Departments of Hospital Pathology, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2543447
- DOI: http://doi.org/10.4166/kjg.2023.026
Abstract
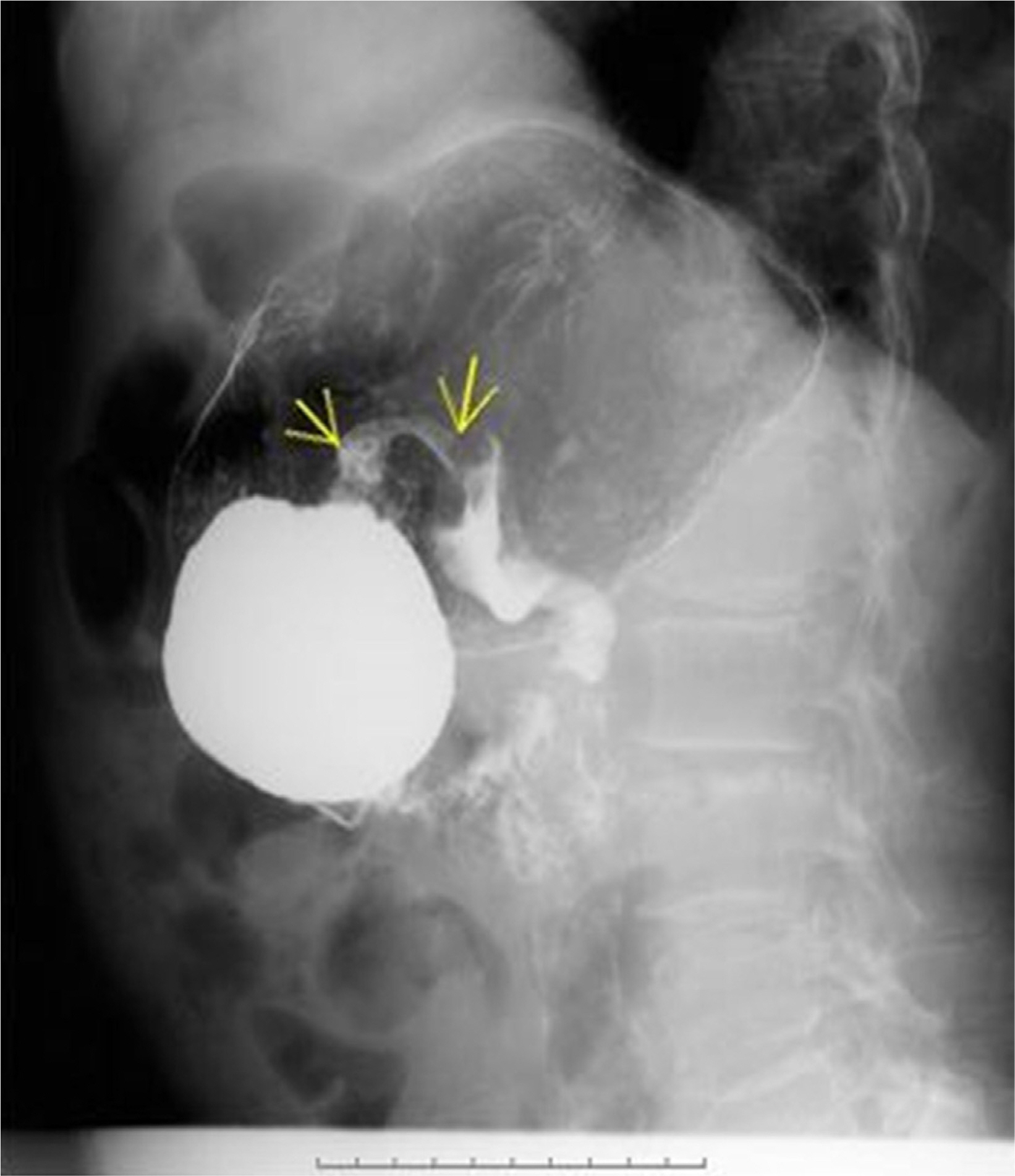
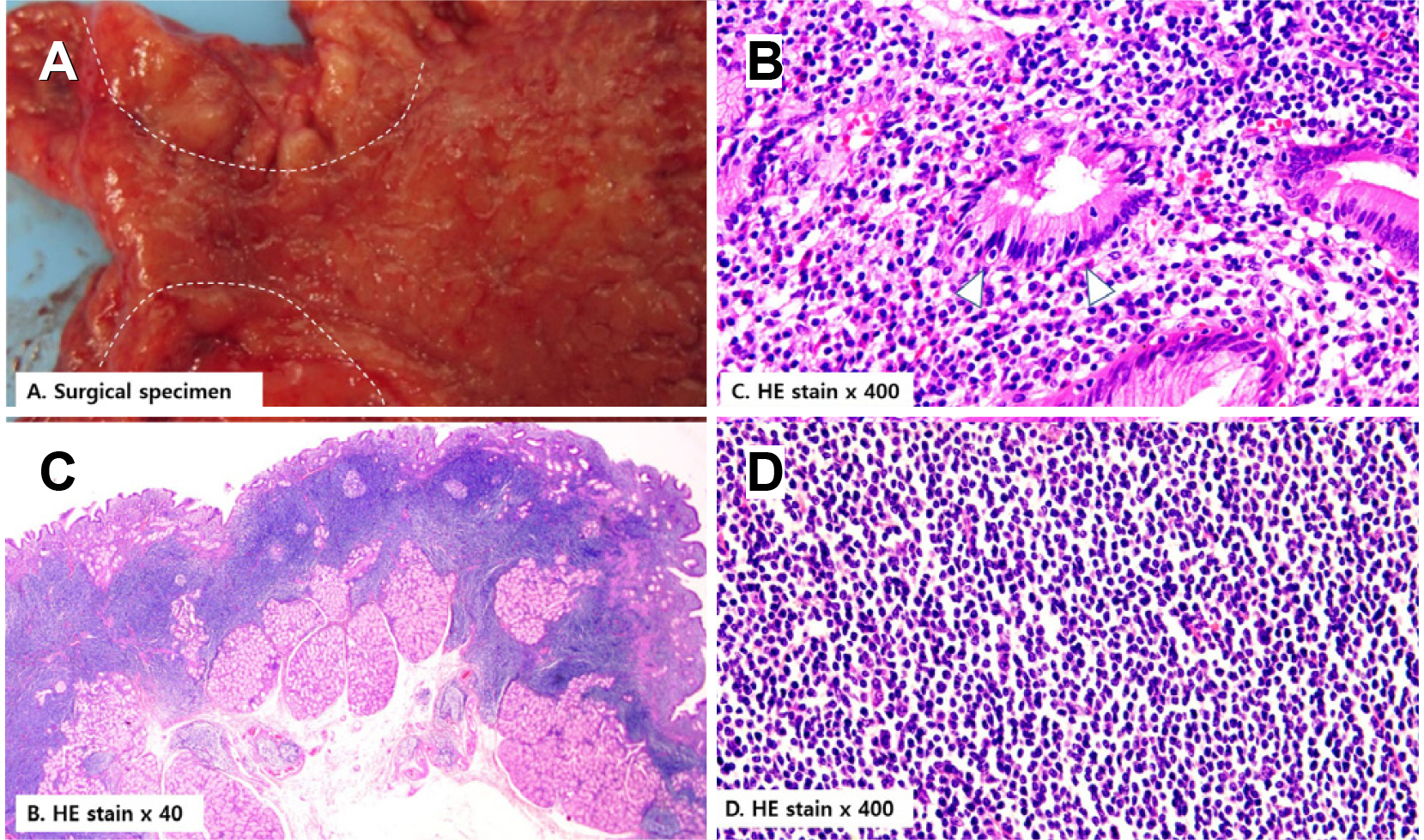
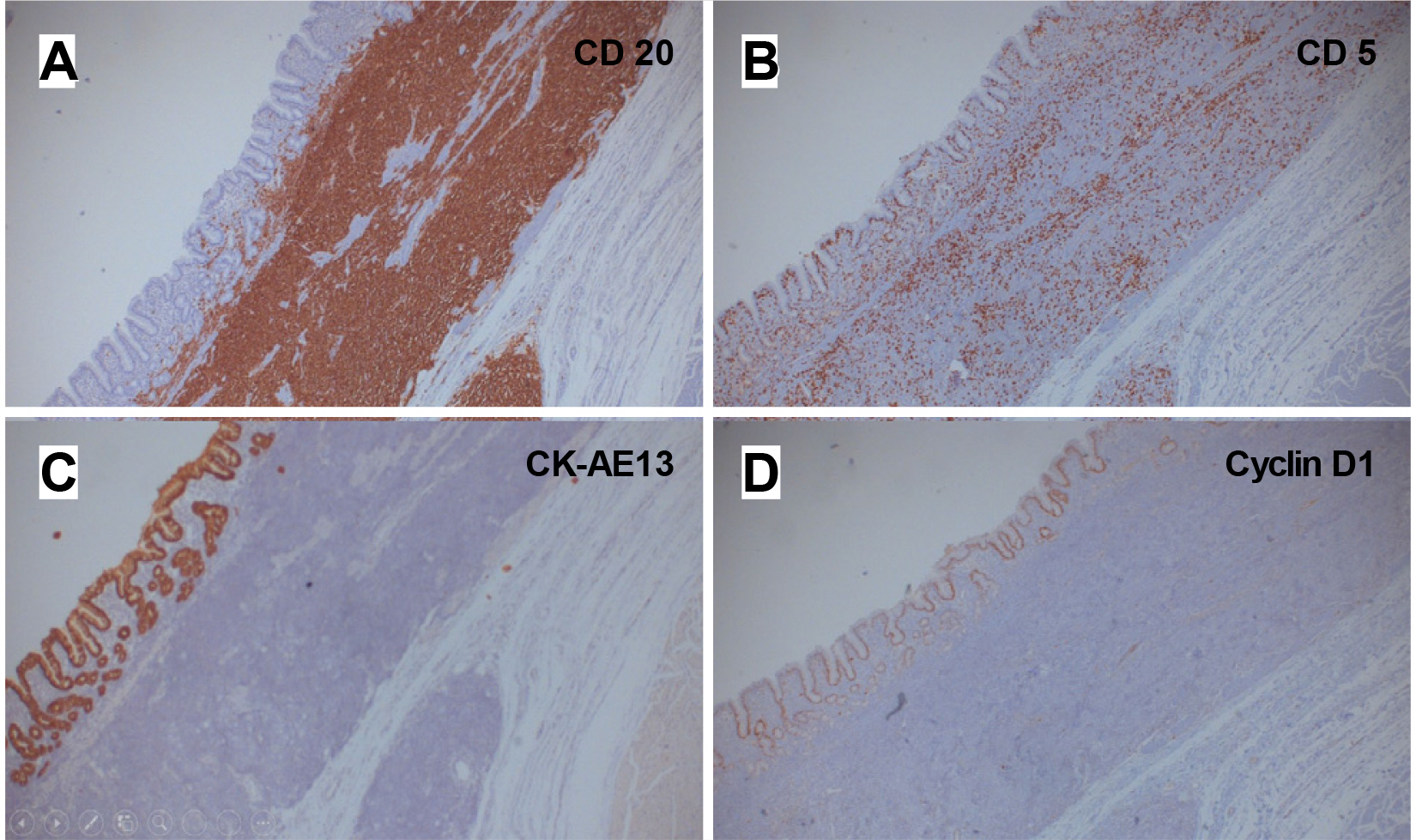
- This paper reports a 70-year-old female with gastric extranodal marginal zone B cell lymphoma of mucosa-associated lymphoid tissue (gastric MALT lymphoma) as a rare case of gastric outlet obstruction. Five years earlier, she initially presented with weight loss and anemia. Esophagogastroduodenoscopy (EGD) revealed multiple gastric and duodenal ulcers with a pyloric deformity, while histology revealed chronic active inflammation and a Helicobacter pylori (H. pylori) infection. Three years earlier, she underwent EGD per the National Cancer Screening Program and was diagnosed with antral and duodenal ulcers. A forceps biopsy specimen from one of the ulcers showed the findings of gastric MALT lymphoma, but she did not visit the hospital for proper management. She visited complaining of a loss of appetite. EGD revealed a gastric outlet obstruction (GOO) caused by antral deformity and pyloric narrowing. A staged workup with CT and PET revealed full-layered, encircling antral wall thickening and several enlarged mesenteric lymph nodes. She was finally diagnosed with a gastric MALT lymphoma at Ann Arbor stage I1E with translocation t(11;18). She was treated with palliative surgery for GOO and systemic chemotherapy with a CHOP regimen. This paper reports a gastric MALT lymphoma that progressed from superficial mucosal lesions to an overt mass with regional lymph node metastasis for five years. (Korean J Gastroenterol 2023;81:265 -269)
Keyword
Figure
Reference
-
1. Isaacson P, Wright DH. 1983; Malignant lymphoma of mucosa-associated lymphoid tissue. A distinctive type of B-cell lymphoma. Cancer. 52:1410–1416. DOI: 10.1002/1097-0142(19831015)52:8<1410::aid-cncr2820520813>3.0.co;2-3. PMID: 6193858.
Article2. Wang YG, Zhao LY, Liu CQ, et al. 2016; Clinical characteristics and prognostic factors of primary gastric lymphoma: A retrospective study with 165 cases. Medicine (Baltimore). 95:e4250. DOI: 10.1097/MD.0000000000004250. PMID: 27495029. PMCID: PMC4979783.3. Zaki M, Schubert ML. 1995; Helicobacter pylori and gastric lymphoma. Gastroenterology. 108:610–612. DOI: 10.1016/0016-5085(95)90098-5.
Article4. Park HS, Kim YJ, Yang WI, Suh CO, Lee YC. 2010; Treatment outcome of localized Helicobacter pylori-negative low-grade gastric MALT lymphoma. World J Gastroenterol. 16:2158–2562. DOI: 10.3748/wjg.v16.i17.2158. PMID: 20440857. PMCID: PMC2864842.
Article5. Zullo A, Hassan C, Cristofari F, et al. 2010; Effects of Helicobacter pylori eradication on early stage gastric mucosa-associated lymphoid tissue lymphoma. Clin Gastroenterol Hepatol. 8:105–110. DOI: 10.1016/j.cgh.2009.07.017. PMID: 19631287.
Article6. Kim JS, Park JC, Lee JY, et al. 2021; Long-term clinical outcomes of gastric MALT lymphoma: A nationwide multicenter study in Korea. Front Oncol. 11:681689. DOI: 10.3389/fonc.2021.681689. PMID: 34722238. PMCID: PMC8551628.
Article7. Malfertheiner P, Megraud F, O'Morain C, et al. 2007; Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report. Gut. 56:772–781. DOI: 10.1136/gut.2006.101634. PMID: 17170018. PMCID: PMC1954853.
Article8. Nakamura S, Hojo M. 2022; Diagnosis and treatment for gastric mucosa-associated lymphoid tissue (MALT) lymphoma. J Clin Med. 12:120. DOI: 10.3390/jcm12010120. PMID: 36614921. PMCID: PMC9820981.
Article9. Moleiro J, Ferreira S, Lage P, Dias Pereira A. 2016; Gastric malt lymphoma: Analysis of a series of consecutive patients over 20 years. United European Gastroenterol J. 4:395–402. DOI: 10.1177/2050640615612934. PMID: 27403306. PMCID: PMC4924435.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Helicobacter pylori-negative Gastric Mucosa-associated Lymphoid Tissue Lymphoma
- Role of Chemotherapy in Gastric Marginal Zone B-Cell Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT) Type
- A Man with Dysphagia after Cervical Esophagogastrostomy: A Case Report
- Gastrointestinal Lymphoma
- Endoscopic Diagnosis of Gastric MALT Lymphoma