Korean J Gastroenterol.
2023 Jun;81(6):259-264. 10.4166/kjg.2023.019.
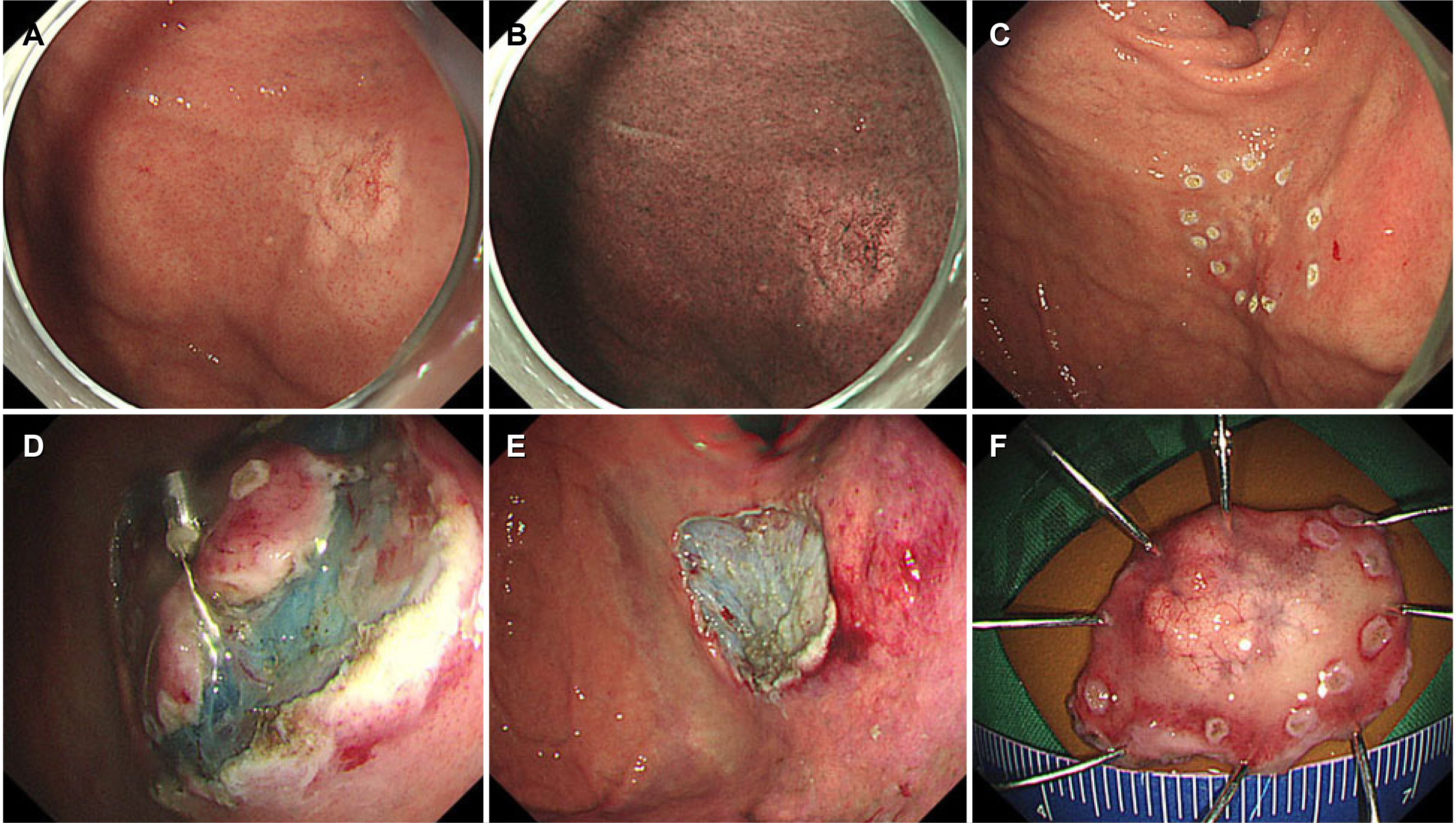
Endoscopic Resection for Gastric Adenocarcinoma of the Fundic Gland Type: A Case Series
- Affiliations
-
- 1Division of Gastroenterology, Pusan National University Hospital, Busan, Korea
- 2Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea
- 3Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 4Department of Pathology, Pusan National University Hospital, Busan, Korea
- KMID: 2543446
- DOI: http://doi.org/10.4166/kjg.2023.019
Abstract
- The fundic gland type (GA-FG) of gastric adenocarcinoma is a rare variant of gastric cancer recently included in the 5th edition of the World Health Organization’s classification of digestive system tumors. Five patients with GA-FG underwent an endoscopic resection at our institution. None of the patients had a Helicobacter pylori infection. Four lesions were located in the upper third of the stomach, and one was in the lower third. Three lesions had a IIa shape, while two resembled a subepithelial tumor. An endoscopic submucosal dissection was performed in four patients and endoscopic mucosal resection in one. Tumor cells were composed of well-differentiated columnar cells mimicking fundic gland cells, and the median tumor size was 10 mm. Three lesions exhibited submucosal invasion. No lymphatic or venous invasion was observed. Tumor cells were positive for MUC6 in all five cases; one case was focally positive for MUC5AC. No recurrence was observed during a median follow-up period of 13 months. An endoscopic resection can be a safe treatment modality for GA-FG, considering its small size and low risk of recurrence or metastasis. (Korean J Gastroenterol 2023;81:259-264)
Figure
Reference
-
1. Lauren P. 1965; The two histological main types of gastric carcinoma: Diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 64:31–49. DOI: 10.1111/apm.1965.64.1.31. PMID: 14320675.2. Nakamura K, Sugano H, Takagi K. 1968; Carcinoma of the stomach in incipient phase: its histogenesis and histological appearances. Gan. 59:251–258. PMID: 5726267.3. Ueyama H, Yao T, Nakashima Y, et al. 2010; Gastric adenocarcinoma of fundic gland type (chief cell predominant type): proposal for a new entity of gastric adenocarcinoma. Am J Surg Pathol. 34:609–619. DOI: 10.1097/pas.0b013e3181d94d53. PMID: 20410811.
Article4. WHO Classification of Tumours Editorial Board. WHO Classification of Tumours of the Digestive System. 5th ed. IARC Lyon;2019.5. Chiba T, Kato K, Masuda T, et al. 2016; Clinicopathological features of gastric adenocarcinoma of the fundic gland (chief cell predominant type) by retrospective and prospective analyses of endoscopic findings. Dig Endosc. 28:722–730. DOI: 10.1111/den.12676. PMID: 27129734.
Article6. Kino H, Nakano M, Kanamori A, et al. 2018; Gastric adenocarcinoma of the fundic gland type after endoscopic therapy for metachronous gastric cancer. Intern Med. 57:795–800. DOI: 10.2169/internalmedicine.9359-17. PMID: 29225256. PMCID: PMC5891516.
Article7. Park ES, Kim YE, Park CK, Yao T, Kushima R, Kim KM. 2012; Gastric adenocarcinoma of fundic gland type: report of three cases. Korean J Pathol. 46:287–291. DOI: 10.4132/koreanjpathol.2012.46.3.287. PMID: 23110017. PMCID: PMC3479759.
Article8. Miyazawa M, Matsuda M, Yano M, et al. 2015; Gastric adenocarcinoma of fundic gland type: Five cases treated with endoscopic resection. World J Gastroenterol. 21:8208–8214. DOI: 10.3748/wjg.v21.i26.8208. PMID: 26185396. PMCID: PMC4499367.
Article9. Matsuda A, Matsuda T, Shibata A, et al. Cancer incidence and incidence rates in Japan in 2008: a study of 25 population-based cancer registries for the Monitoring of Cancer Incidence in Japan (MCIJ) project. Jpn J Clin Oncol. 2014; 44:388–396. DOI: 10.1093/jjco/hyu003. PMID: 24503029.
Article10. Miyazawa M, Matsuda M, Yano M, et al. 2016; Gastric adenocarcinoma of the fundic gland (chief cell-predominant type): A review of endoscopic and clinicopathological features. World J Gastroenterol. 22:10523–10531. DOI: 10.3748/wjg.v22.i48.10523. PMID: 28082804. PMCID: PMC5192263.
Article11. Kim YJ, Lee SY, Kim JH, Sung IK, Park HS. 2022; Incidence of infection among subjects with Helicobacter pylori seroconversion. Clin Endosc. 55:67–76. DOI: 10.5946/ce.2020.299. PMID: 33794562. PMCID: PMC8831407.
Article12. Ueyama H, Matsumoto K, Nagahara A, Hayashi T, Yao T, Watanabe S. 2014; Gastric adenocarcinoma of the fundic gland type (chief cell predominant type). Endoscopy. 46:153–157. DOI: 10.1055/s-0033-1359042. PMID: 24338239.
Article13. Yang M, Sun X, Chen Y, Yang P. Twenty cases of gastric adenocarcinoma of the fundic gland type. Scand J Gastroenterol. 2023; Jan. doi: 10.1080/00365521.2022.2164213. DOI: 10.1080/00365521.2022.2164213. PMID: 36604805.
Article14. Lee W. 2021; Application of current image-enhanced endoscopy in gastric diseases. Clin Endosc. 54:477–487. DOI: 10.5946/ce.2021.160. PMID: 34315196. PMCID: PMC8357595.
Article15. Kushima R, Sekine S, Matsubara A, Taniguchi H, Ikegami M, Tsuda H. 2013; Gastric adenocarcinoma of the fundic gland type shares common genetic and phenotypic features with pyloric gland adenoma. Pathol Int. 63:318–325. DOI: 10.1111/pin.12070. PMID: 23782334.
Article16. Ota H, Yamaguchi D, Iwaya M, et al. 2015; Principal cells in gastric neoplasia of fundic gland (chief cell predominant) type show characteristics of immature chief cells. Pathol Int. 65:202–204. DOI: 10.1111/pin.12244. PMID: 25597649.
Article17. Hidaka Y, Mitomi H, Saito T, et al. 2013; Alteration in the Wnt/β-catenin signaling pathway in gastric neoplasias of fundic gland (chief cell predominant) type. Hum Pathol. 44:2438–2448. DOI: 10.1016/j.humpath.2013.06.002. PMID: 24011952.
Article18. Li C, Wu X, Yang S, Yang X, Yao J, Zheng H. 2020; Gastric adenocarcinoma of the fundic gland type: clinicopathological features of eight patients treated with endoscopic submucosal dissection. Diagn Pathol. 15:131. DOI: 10.1186/s13000-020-01047-2. PMID: 33097069. PMCID: PMC7585219.
Article19. Park YB, Kim GH, Kim K, Ha TK, Park GB, Kwak YM. 2021; Gastric adenocarcinoma of fundic gland type treated by endoscopic submucosal dissection. Korean J Helicobacter Up Gastrointest Res. 21:82–85.
Article20. Lee SY. 2021; Helicobacter pylori-negative gastric cancer. Korean J Helicobacter Up Gastrointest Res. 21:10–21. DOI: 10.7704/kjhugr.2020.0044. DOI: 10.7704/kjhugr.2020.0036. PMID: 25807972.
Article21. Park CH, Yang DH, Kim JW, et al. 2020; Clinical practice guideline for endoscopic resection of early gastrointestinal cancer. Clin Endosc. 53:142–166. DOI: 10.5946/ce.2020.032. PMID: 32252507. PMCID: PMC7137564.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gastric Adenocarcinoma of Fundic Gland Type Treated by Endoscopic Submucosal Dissection
- Gastric Adenocarcinoma of Fundic-gland Type Diagnosed and Treated by Endoscopic Mucosal Resection
- A Case of Atypical Fundic Gland Hyperplasia Confirmed by Endoscopic Mucosal Resection
- Long-term Observation of Gastric Adenocarcinoma of Fundic Gland Mucosa Type before and after Helicobacter pylori Eradication: a Case Report
- Oxyntic Gland Adenoma Treated by Endoscopic Mucosal Resection