J Neurocrit Care.
2023 Jun;16(1):43-45. 10.18700/jnc.230020.
Myelin oligodendrocyte glycoprotein antibody-associated disease manifesting as intractable fever managed by bromocriptine: a case report
- Affiliations
-
- 1Department of Neurology, Kyung Hee University Hospital, Seoul, Korea
- 2Department of Neurology, Inje University Busan Paik Hospital, Busan, Korea
- KMID: 2543392
- DOI: http://doi.org/10.18700/jnc.230020
Abstract
- Background
Demyelinating events expressed as abnormal thermoregulatory responses are rare, but intractable fever in myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD) is very rarely reported.
Case Report
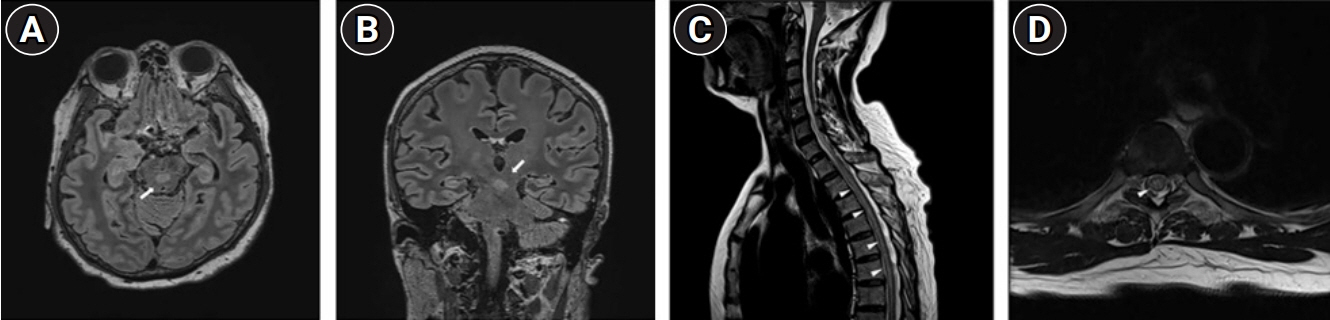
A 56-year-old woman presented with quadriparesis with acroparesthesia. During the admission, fever developed and persisted for 2 days despite the administration of high-dose antipyretics. Brain magnetic resonance imaging (MRI) showed hyperintense lesions involving the upper brainstem. A diagnosis of MOGAD was made according to the clinical characteristics and presence of seropositive MOG antibody. After administration of oral bromocriptine (2.5 mg/day), fever was slowly controlled for a few days.
Conclusion
The present case explained that persistent fever in MOGAD could manifest as an uncommon manifestation. The lesion in the upper brainstem within the brain MRI could be thought of as a lesion anterior to the periaqueductal gray and the lesion at that site could be the cause of the patient's persistent fever with unknown origin.
Figure
Reference
-
1. Banwell B, Bennett JL, Marignier R, Kim HJ, Brilot F, Flanagan EP, et al. Diagnosis of myelin oligodendrocyte glycoprotein antibody-associated disease: International MOGAD Panel proposed criteria. Lancet Neurol. 2023; 22:268–82.2. Jurynczyk M, Messina S, Woodhall MR, Raza N, Everett R, Roca-Fernandez A, et al. Clinical presentation and prognosis in MOG-antibody disease: a UK study. Brain. 2017; 140:3128–38.3. Levy M. Expanding the spectrum of MOG antibody disease. Mult Scler. 2020; 26:515–6.4. Hsu CL, Yeh JH, Lau CI. Persistent hyperthermia in a patient with aquaporin-4-antibody-positive neuromyelitis optica spectrum disorder. J Clin Neurol. 2016; 12:515–6.5. Weiss N, Hasboun D, Demeret S, Fontaine B, Bolgert F, Lyon-Caen O, et al. Paroxysmal hypothermia as a clinical feature of multiple sclerosis. Neurology. 2009; 72:193–5.6. Kwon YN, Kim B, Kim JS, Mo H, Choi K, Oh SI, et al. Myelin oligodendrocyte glycoprotein-immunoglobulin G in the CSF: clinical implication of testing and association with disability. Neurol Neuroimmunol Neuroinflamm. 2021; 9:e1095.7. Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015; 85:177–89.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Immunocytochemical localization of myelin basic protein, proteolipid protein and myelin-associated glycoprotein in human oligodendrocyte in culture
- Clinical and Radiological Features of Myelin Oligodendrocyte Glycoprotein-Associated Myelitis in Adults
- A Case of Magnetic Resonance Imaging-Negative Myelitis Associated with Myelin Oligodendrocyte Glycoprotein Autoantibodies
- MOG Antibody-Positive Myelopathy as a Paraneoplastic Manifestation of Lymphoma
- Myelin Oligodendrocyte Glycoprotein Antibody-Associated Disorder Manifesting as a Lesion on the Postcentral Hand Knob