J Neurocrit Care.
2023 Jun;16(1):39-42. 10.18700/jnc.230018.
Concomitant moyamoya syndrome and infratentorial arteriovenous malformation in a neurofibromatosis type 1 patient: a case report
- Affiliations
-
- 1Department of Neurology, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2543391
- DOI: http://doi.org/10.18700/jnc.230018
Abstract
- Background
Neurofibromatosis type 1 (NF1) is a genetic disorder with diverse phenotypic manifestations. Cerebral vasculopathy is one of the multisystem involvements often overlooked unless symptomatic.
Case Report
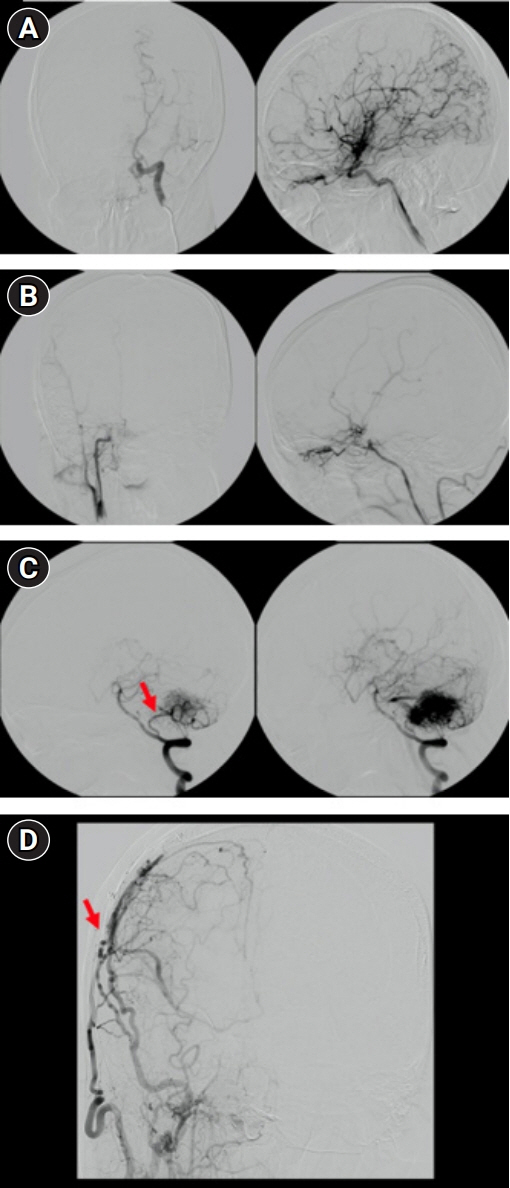
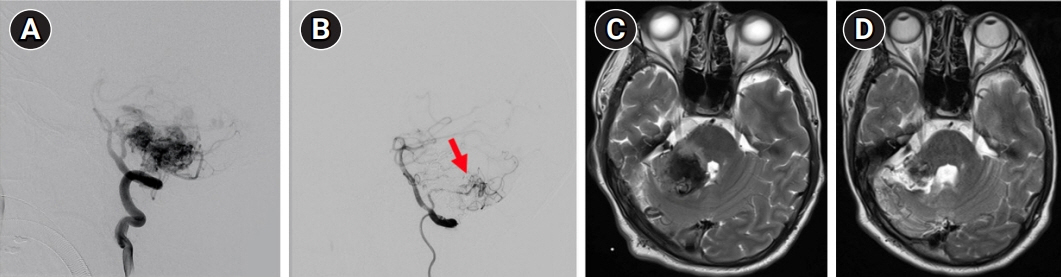
A 28-year-old male patient with prolonged NF1 complained of right-hand position-specific rhythmic tremor after surviving an ipsilateral cerebellar arteriovenous malformation (AVM) hemorrhagic transformation. Not only did he suffer rupture of the infratentorial vasculopathy but he also endured asymmetric supratentorial occlusive vessel changes in Moyamoya syndrome. Due to contralateral limb clumsiness, his right hemispheric vasculature was revascularized by encephaloduroarteriosynangiosis 13 years before the AVM rupture.
Conclusion
This case report describes exceptional NF1 CNS involvement where the cerebral vasculature had concomitant Moyamoya syndrome and unilateral cerebellar AVM in a single patient. Cerebral vasculopathy should be surveyed and adequately addressed during the follow-up of chronic NF1, as it can cause irreversible sequelae or can be life-threatening.
Keyword
Figure
Reference
-
1. Nix JS, Blakeley J, Rodriguez FJ. An update on the central nervous system manifestations of neurofibromatosis type 1. Acta Neuropathol. 2020; 139:625–41.2. Barreto-Duarte B, Andrade-Gomes FH, Arriaga MB, Araújo-Pereira M, Cubillos-Angulo JM, Andrade BB. Association between neurofibromatosis type 1 and cerebrovascular diseases in children: a systematic review. PLoS One. 2021; 16:e0241096.3. Gutmann DH, Ferner RE, Listernick RH, Korf BR, Wolters PL, Johnson KJ. Neurofibromatosis type 1. Nat Rev Dis Primers. 2017; 3:17004.4. Monroe CL, Dahiya S, Gutmann DH. Dissecting clinical heterogeneity in neurofibromatosis type 1. Annu Rev Pathol. 2017; 12:53–74.5. Vogel AC, Gutmann DH, Morris SM. Neurodevelopmental disorders in children with neurofibromatosis type 1. Dev Med Child Neurol. 2017; 59:1112–6.6. Zessis NR, Gao F, Vadlamudi G, Gutmann DH, Hollander AS. Height growth impairment in children with neurofibromatosis type 1 is characterized by decreased pubertal growth velocity in both sexes. J Child Neurol. 2018; 33:762–6.7. Terry AR, Jordan JT, Schwamm L, Plotkin SR. Increased risk of cerebrovascular disease among patients with neurofibromatosis type 1: population-based approach. Stroke. 2016; 47:60–5.8. Kaas B, Huisman TA, Tekes A, Bergner A, Blakeley JO, Jordan LC. Spectrum and prevalence of vasculopathy in pediatric neurofibromatosis type 1. J Child Neurol. 2013; 28:561–9.9. Bargiela D, Verkerk MM, Wee I, Welman K, Ng E, Choong AM. The endovascular management of neurofibromatosis-associated aneurysms: a systematic review. Eur J Radiol. 2018; 100:66–75.10. Puschmann A, Wszolek ZK. Diagnosis and treatment of common forms of tremor. Semin Neurol. 2011; 31:65–77.11. Kim H, Al-Shahi Salman R, McCulloch CE, Stapf C, Young WL; MARS Coinvestigators. Untreated brain arteriovenous malformation: patient-level meta-analysis of hemorrhage predictors. Neurology. 2014; 83:590–7.12. Germans MR, Sun W, Sebök M, Keller A, Regli L. Molecular signature of brain arteriovenous malformation hemorrhage: a systematic review. World Neurosurg. 2022; 157:143–51.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neurofibromatosis Type 1 with Spinal Arteriovenous Malformation
- A Case of Neurofibromatosis Type I with Moyamoya Syndrome and Ganglioneuroma in Lung
- Spontaneous Hemothorax Caused by Rupture of an Intercostal Artery Aneurysm in Neurofibromatosis Type I I : A Case Report
- A Case of Probable Moyamoya Disease (Unilateal Moyamoya Disease) Coexisting Arteriovenous Malformation
- Moyamoya Syndrome: A Window of Moyamoya Disease