Neurointervention.
2023 Jun;18(2):107-113. 10.5469/neuroint.2023.00164.
The Current Limitations and Advanced Analysis of Hemodynamic Study of Cerebral Aneurysms
- Affiliations
-
- 1Department of Neurosurgery, Yongin Severance Hospital, Yongin, Korea
- KMID: 2543365
- DOI: http://doi.org/10.5469/neuroint.2023.00164
Abstract
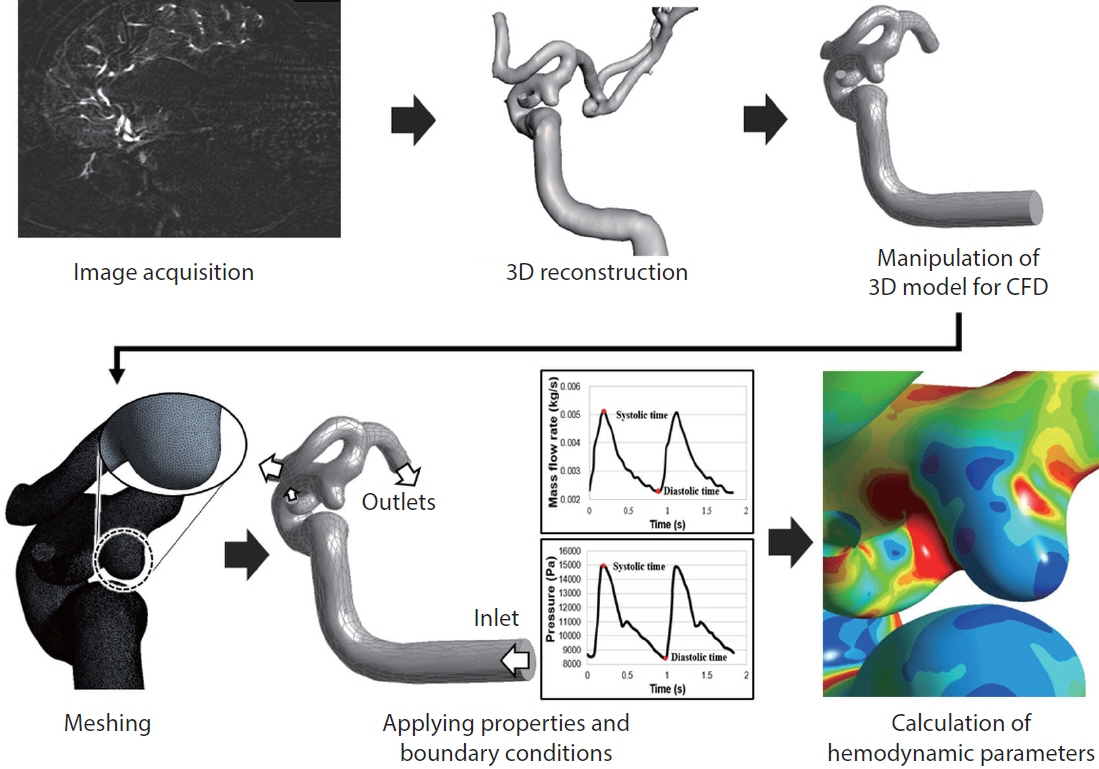
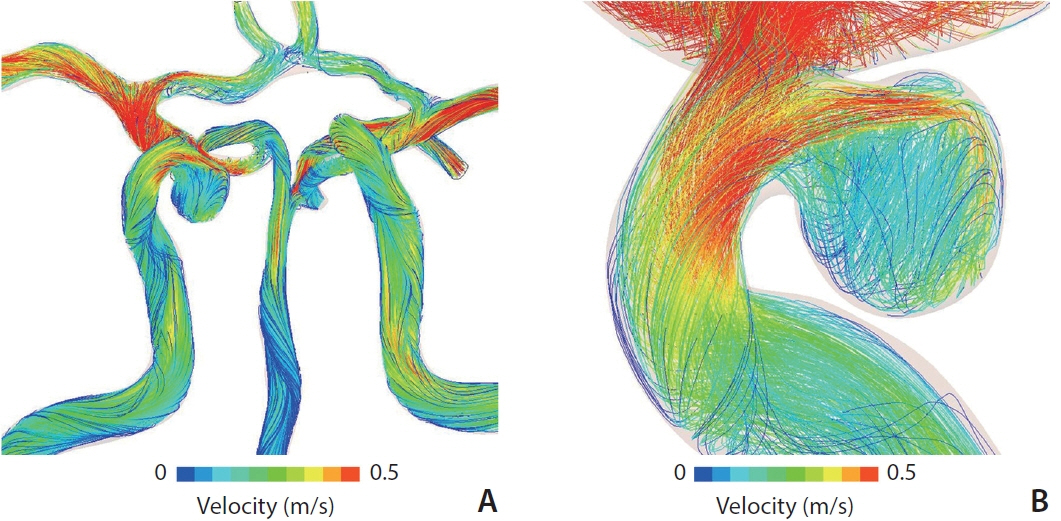
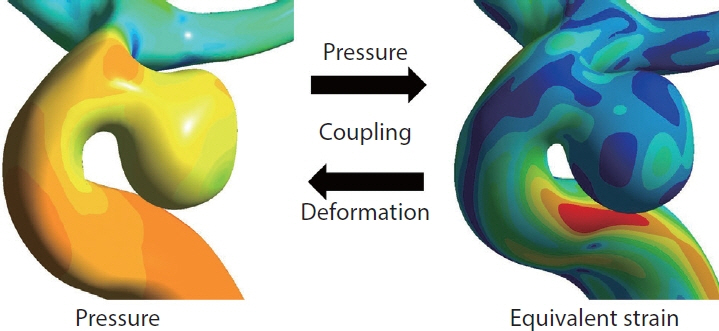
- Among the various perspectives on cerebrovascular diseases, hemodynamic analysis—which has recently garnered interest—is of great help in understanding cerebrovascular diseases. Computational fluid dynamics (CFD) analysis has been the primary hemodynamic analysis method, and studies on cerebral aneurysms have been actively conducted. However, owing to the intrinsic limitations of the analysis method, the role of wall shear stress (WSS), the most representative parameter, remains controversial. High WSS affects the formation of cerebral aneurysms; however, no consensus has been reached on the role of WSS in the growth and rupture of cerebral aneurysms. Therefore, this review aimed to briefly introduce the up-to-date results and limitations made through CFD analysis and to inform the need for a new hemodynamic analysis method.
Keyword
Figure
Reference
-
1. Cebral J, Ollikainen E, Chung BJ, Mut F, Sippola V, Jahromi BR, et al. Flow conditions in the intracranial aneurysm lumen are associated with inflammation and degenerative changes of the aneurysm wall. AJNR Am J Neuroradiol. 2017; 38:119–126.
Article2. Cho KC, Choi JH, Oh JH, Kim YB. Prediction of thin-walled areas of unruptured cerebral aneurysms through comparison of normalized hemodynamic parameters and intraoperative images. Biomed Res Int. 2018; 2018:3047181.
Article3. Dhar S, Tremmel M, Mocco J, Kim M, Yamamoto J, Siddiqui AH, et al. Morphology parameters for intracranial aneurysm rupture risk assessment. Neurosurgery. 2008; 63:185–196. discussion 196-197.4. Feigin VL, Rinkel GJ, Lawes CM, Algra A, Bennett DA, van Gijn J, et al. Risk factors for subarachnoid hemorrhage: an updated systematic review of epidemiological studies. Stroke. 2005; 36:2773–2780.5. Frösen J, Piippo A, Paetau A, Kangasniemi M, Niemelä M, Hernesniemi J, et al. Remodeling of saccular cerebral artery aneurysm wall is associated with rupture: histological analysis of 24 unruptured and 42 ruptured cases. Stroke. 2004; 35:2287–2293.
Article6. Huang ZQ, Meng ZH, Hou ZJ, Huang SQ, Chen JN, Yu H, et al. Geometric parameter analysis of ruptured and unruptured aneurysms in patients with symmetric bilateral intracranial aneurysms: a multicenter CT angiography study. AJNR Am J Neuroradiol. 2016; 37:1413–1417.
Article7. Kleinloog R, de Mul N, Verweij BH, Post JA, Rinkel GJE, Ruigrok YM. Risk factors for intracranial aneurysm rupture: a systematic review. Neurosurgery. 2018; 82:431–440.
Article8. Raghavan ML, Ma B, Harbaugh RE. Quantified aneurysm shape and rupture risk. J Neurosurg. 2005; 102:355–362.
Article9. Rahman M, Smietana J, Hauck E, Hoh B, Hopkins N, Siddiqui A, et al. Size ratio correlates with intracranial aneurysm rupture status: a prospective study. Stroke. 2010; 41:916–920.10. Ujiie H, Tachibana H, Hiramatsu O, Hazel AL, Matsumoto T, Ogasawara Y, et al. Effects of size and shape (aspect ratio) on the hemodynamics of saccular aneurysms: a possible index for surgical treatment of intracranial aneurysms. Neurosurgery. 1999; 45:119–129. discussion 129-130.
Article11. Yasuda R, Strother CM, Taki W, Shinki K, Royalty K, Pulfer K, et al. Aneurysm volume-to-ostium area ratio: a parameter useful for discriminating the rupture status of intracranial aneurysms. Neurosurgery. 2011; 68:310–317. discussion 317-318.
Article12. Zheng Y, Xu F, Ren J, Xu Q, Liu Y, Tian Y, et al. Assessment of intracranial aneurysm rupture based on morphology parameters and anatomical locations. J Neurointerv Surg. 2016; 8:1240–1246.
Article13. Soldozy S, Norat P, Elsarrag M, Chatrath A, Costello JS, Sokolowski JD, et al. The biophysical role of hemodynamics in the pathogenesis of cerebral aneurysm formation and rupture. Neurosurg Focus. 2019; 47:E11.
Article14. Dolan JM, Kolega J, Meng H. High wall shear stress and spatial gradients in vascular pathology: a review. Ann Biomed Eng. 2013; 41:1411–1427.
Article15. Alfano JM, Kolega J, Natarajan SK, Xiang J, Paluch RA, Levy EI, et al. Intracranial aneurysms occur more frequently at bifurcation sites that typically experience higher hemodynamic stresses. Neurosurgery. 2013; 73:497–505.
Article16. Chen H, Selimovic A, Thompson H, Chiarini A, Penrose J, Ventikos Y, et al. Investigating the influence of haemodynamic stimuli on intracranial aneurysm inception. Ann Biomed Eng. 2013; 41:1492–1504.
Article17. Gao L, Hoi Y, Swartz DD, Kolega J, Siddiqui A, Meng H. Nascent aneurysm formation at the basilar terminus induced by hemodynamics. Stroke. 2008; 39:2085–2090.
Article18. Geers AJ, Morales HG, Larrabide I, Butakoff C, Bijlenga P, Frangi AF. Wall shear stress at the initiation site of cerebral aneurysms. Biomech Model Mechanobiol. 2017; 16:97–115.
Article19. Meng H, Swartz DD, Wang Z, Hoi Y, Kolega J, Metaxa EM, et al. A model system for mapping vascular responses to complex hemodynamics at arterial bifurcations in vivo. Neurosurgery. 2006; 59:1094–1100. discussion 1100-1101.
Article20. Meng H, Wang Z, Hoi Y, Gao L, Metaxa E, Swartz DD, et al. Complex hemodynamics at the apex of an arterial bifurcation induces vascular remodeling resembling cerebral aneurysm initiation. Stroke. 2007; 38:1924–1931.
Article21. Sforza DM, Putman CM, Cebral JR. Hemodynamics of cerebral aneurysms. Annu Rev Fluid Mech. 2009; 41:91–107.
Article22. Can A, Du R. Association of hemodynamic factors with intracranial aneurysm formation and rupture: systematic review and meta-analysis. Neurosurgery. 2016; 78:510–520.
Article23. Castro MA, Putman CM, Sheridan MJ, Cebral JR. Hemodynamic patterns of anterior communicating artery aneurysms: a possible association with rupture. AJNR Am J Neuroradiol. 2009; 30:297–302.
Article24. Cebral JR, Mut F, Weir J, Putman C. Quantitative characterization of the hemodynamic environment in ruptured and unruptured brain aneurysms. AJNR Am J Neuroradiol. 2011; 32:145–151.
Article25. Hassan T, Timofeev EV, Saito T, Shimizu H, Ezura M, Matsumoto Y, et al. A proposed parent vessel geometry-based categorization of saccular intracranial aneurysms: computational flow dynamics analysis of the risk factors for lesion rupture. J Neurosurg. 2005; 103:662–680.
Article26. Nixon AM, Gunel M, Sumpio BE. The critical role of hemodynamics in the development of cerebral vascular disease. J Neurosurg. 2010; 112:1240–1253.
Article27. Xiang J, Natarajan SK, Tremmel M, Ma D, Mocco J, Hopkins LN, et al. Hemodynamic-morphologic discriminants for intracranial aneurysm rupture. Stroke. 2011; 42:144–152.
Article28. Meng H, Tutino VM, Xiang J, Siddiqui A. High WSS or low WSS? Complex interactions of hemodynamics with intracranial aneurysm initiation, growth, and rupture: toward a unifying hypothesis. AJNR Am J Neuroradiol. 2014; 35:1254–1262.
Article29. Cebral JR, Detmer F, Chung BJ, Choque-Velasquez J, Rezai B, Lehto H, et al. Local hemodynamic conditions associated with focal changes in the intracranial aneurysm wall. AJNR Am J Neuroradiol. 2019; 40:510–516.30. Ramachandran M, Retarekar R, Raghavan ML, Berkowitz B, Dickerhoff B, Correa T, et al. Assessment of image-derived risk factors for natural course of unruptured cerebral aneurysms. J Neurosurg. 2016; 124:288–295.
Article31. Sforza DM, Kono K, Tateshima S, Viñuela F, Putman C, Cebral JR. Hemodynamics in growing and stable cerebral aneurysms. J Neurointerv Surg. 2016; 8:407–412.
Article32. Cebral JR, Meng H. Counterpoint: realizing the clinical utility of computational fluid dynamics--closing the gap. AJNR Am J Neuroradiol. 2012; 33:396–398.
Article33. Robertson AM, Watton PN. Computational fluid dynamics in aneurysm research: critical reflections, future directions. AJNR Am J Neuroradiol. 2012; 33:992–995.
Article34. Murayama Y, Fujimura S, Suzuki T, Takao H. Computational fluid dynamics as a risk assessment tool for aneurysm rupture. Neurosurg Focus. 2019; 47:E12.
Article35. Cho KC, Yang H, Kim JJ, Oh JH, Kim YB. Prediction of rupture risk in cerebral aneurysms by comparing clinical cases with fluid-structure interaction analyses. Sci Rep. 2020; 10:18237.
Article36. Kim JJ, Yang H, Kim YB, Oh JH, Cho KC. The quantitative comparison between high wall shear stress and high strain in the formation of paraclinoid aneurysms. Sci Rep. 2021; 11:7947.
Article37. Yang H, Cho KC, Kim JJ, Kim JH, Kim YB, Oh JH. Rupture risk prediction of cerebral aneurysms using a novel convolutional neural network-based deep learning model. J Neurointerv Surg. 2023; 15:200–204.
Article38. Steinman DA, Pereira VM. How patient specific are patient-specific computational models of cerebral aneurysms? An overview of sources of error and variability. Neurosurg Focus. 2019; 1475:E14.
Article39. Lauric A, Hippelheuser JE, Malek AM. Critical role of angiographic acquisition modality and reconstruction on morphometric and haemodynamic analysis of intracranial aneurysms. J Neurointerv Surg. 2018; 10:911–915.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Saccular Aneurysm of the Azygos Anterior Cerebral Artery: Three Case Reports
- Stent-assisted Coil Embolization of Cerebral Aneurysms: Review Article
- Superior Temporal Gyrus Approach to Middle Cerebral Artery Aneurysms
- New Pathophysiological Considerations on Cerebral Aneurysms
- Multiple Aneurysms of the Distal Anterior Cerebral Artery: Case Report