Ann Pediatr Endocrinol Metab.
2023 Jun;28(2):149-154. 10.6065/apem.2142188.094.
A case of maturity-onset diabetes of the young type 4 in Korea
- Affiliations
-
- 1Department of Pediatrics, Gachon University Gil Medical Center, Incheon, Korea
- 2Department of Pediatrics, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea
- 3Department of Laborator y Medicine, Gachon University Gil Medical Center, Incheon, Korea
- KMID: 2543297
- DOI: http://doi.org/10.6065/apem.2142188.094
Abstract
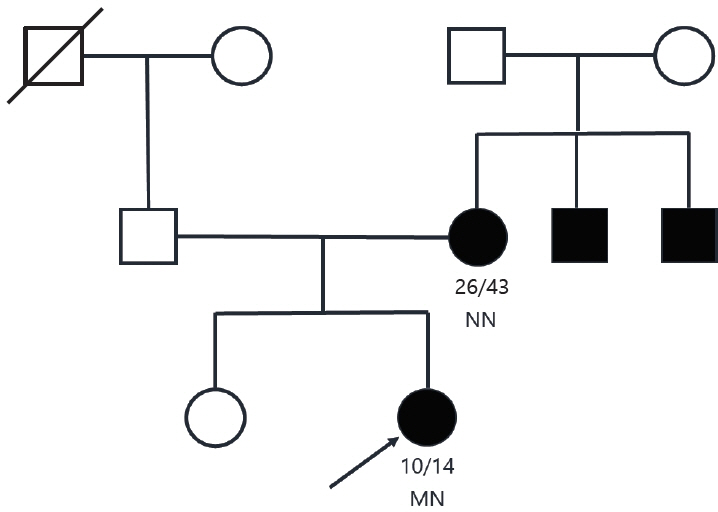
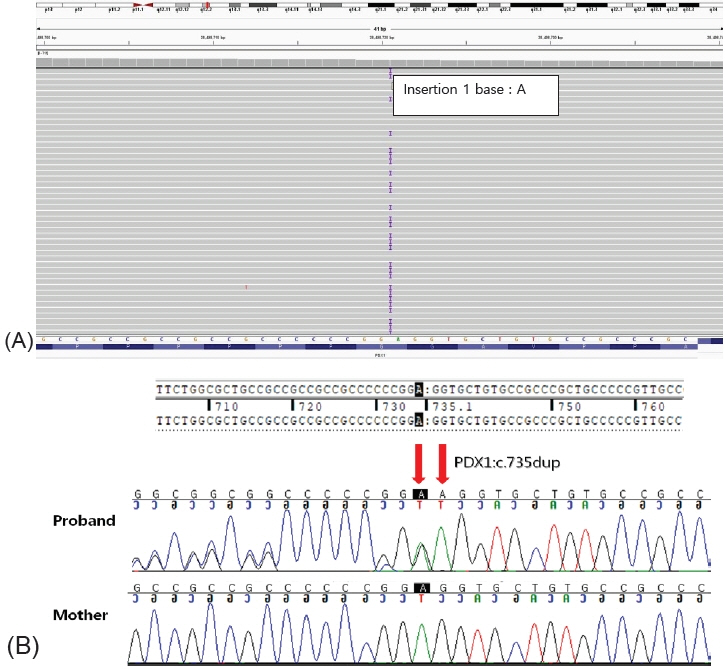
- Maturity-onset diabetes of the young (MODY) is a rare, autosomal dominant disease characterized by non-ketogenic diabetes mellitus (DM). MODY type 4, caused by PDX1 mutation, is a very rare subtype of MODY, especially in Korea. We report a case of a 10-year-old, nonobese girl with a family history of type 2 DM. After diagnosis, the patient’s serum glucose level was well controlled using metformin monotherapy; however, the glycated hemoglobin level increased to 9.0% approximately 2 years after treatment. No obesity or lifestyle problems were observed, and serum fasting C-peptide level was within the normal range. Furthermore, no islet-related autoantibodies were detected. A genetic screening for MODY using a next-generation sequencing panel was performed, and a likely heterozygous pathogenic PDX1 mutation (p.Gly246ArgfsTer21) was identified. The PDX1 variant was not detected in her mother, implying that the mutation had arisen de novo in the proband. She was prescribed insulin degludec in addition to metformin therapy, which improved her hyperglycemia. This report presents a novel MODY type 4 phenotype and highlights the importance of genetic screening in patients with MODY characteristics.
Figure
Reference
-
References
1. Mayer-Davis EJ, Lawrence JM, Dabelea D, Divers J, Isom S, Dolan L, et al. Incidence trends of type 1 and type 2 diabetes among youths, 2002-2012. N Engl J Med. 2017; 376:1419–29.2. Hattersley AT, Greeley SAW, Polak M, Rubio-Cabezas O, Njølstad PR, Mlynarski W, et al. ISPAD clinical practice consensus guidelines 2018: the diagnosis and management of monogenic diabetes in children and adolescents. Pediatr Diabetes. 2018; 19 Suppl 27:47–63.3. Yeung RO, Hannah-Shmouni F, Niederhoffer K, Walker MA. Not quite type 1 or type 2, what now? Review of monogenic, mitochondrial, and syndromic diabetes. Rev Endocr Metab Disord. 2018; 19:35–52.4. Nkonge KM, Nkonge DK, Nkonge TN. The epidemiology, molecular pathogenesis, diagnosis, and treatment of maturity-onset diabetes of the young (MODY). Clin Diabetes Endocrinol. 2020; 6:20.5. Xie F, Chan JC, Ma RC. Precision medicine in diabetes prevention, classification and management. J Diabetes Investig. 2018; 9:998–1015.6. Stoffers DA, Ferrer J, Clarke WL, Habener JF. Early-onset type-II diabetes mellitus (MODY4) linked to IPF1. Nat Genet. 1997; 17:138–9.7. Yang YS, Kwak SH, Park KS. Update on monogenic diabetes in Korea. Diabetes Metab J. 2020; 44:627–39.8. Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015; 17:405–24.9. Heuvel-Borsboom H, de Valk HW, Losekoot M, Westerink J. Maturity onset diabetes of the young: seek and you will find. Neth J Med. 2016; 74:193–200.10. Shields BM, Hicks S, Shepherd MH, Colclough K, Hattersley AT, Ellard S. Maturity-onset diabetes of the young (MODY): how many cases are we missing? Diabetologia. 2010; 53:2504–8.11. Fajans SS, Bell GI, Paz VP, Below JE, Cox NJ, Martin C, et al. Obesity and hyperinsulinemia in a family with pancreatic agenesis and MODY caused by the IPF1 mutation Pro63fsX60. Transl Res. 2010; 156:7–14.12. Caetano LA, Santana LS, Costa-Riquetto AD, Lerario AM, Nery M, Nogueira GF, et al. PDX1 -MODY and dorsal pancreatic agenesis: new phenotype of a rare disease. Clin Genet. 2018; 93:382–6.13. Stanik J, Dusatkova P, Cinek O, Valentinova L, Huckova M, Skopkova M, et al. de novo mutations of GCK, HNF1A and HNF4A may be more frequent in MODY than previously assumed. Diabetologia. 2014; 57:480–4.14. Delvecchio M, Pastore C, Giordano P. Treatment options for MODY patients: a systematic review of literature. Diabetes Ther. 2020; 11:1667–85.15. Mangrum C, Rush E, Shivaswamy V. Genetically targeted dipeptidyl peptidase-4 inhibitor use in a patient with a novel mutation of MODY type 4. Clin Med Insights Endocrinol Diabetes. 2015; 8:83–6.16. Deng M, Xiao X, Zhou L, Wang T. First Case Report of maturity-onset diabetes of the young type 4 pedigree in a chinese family. Front Endocrinol (Lausanne). 2019; 10:406.17. Abreu GM Miss, Tarantino RM, da Fonseca ACP, de Souza RB, Soares CAPD, Cabello PH, et al. PDX1-MODY: a rare missense mutation as a cause of monogenic diabetes. Eur J Med Genet. 2021; 64:104194.18. Al-Kandari H, Al-Abdulrazzaq D, Davidsson L, Nizam R, Jacob S, Melhem M, et al. Identification of Maturity-Onset-Diabetes of the Young (MODY) mutations in a country where diabetes is endemic. Sci Rep. 2021; 11:16060.19. Özdemir TR, Kırbıyık Ö, Dündar BN, Abacı A, Kaya ÖÖ, Çatlı G, et al. Targeted next generation sequencing in patients with maturity-onset diabetes of the young (MODY). J Pediatr Endocrinol Metab. 2018; 31:1295–304.20. Anık A, Çatlı G, Abacı A, Sarı E, Yeşilkaya E, Korkmaz HA, et al. Molecular diagnosis of maturity-onset diabetes of the young (MODY) in Turkish children by using targeted next-generation sequencing. J Pediatr Endocrinol Metab. 2015; 28:1265–71.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Maturity-Onset Diabetes of the Young: What Do Clinicians Need to Know?
- Maturity-onset diabetes of the young: update and perspectives on diagnosis and treatment
- A rare, likely pathogenic GCK variant related to maturity-onset diabetes of the young type 2: A case report
- MODY Syndrome
- Management of Type 2 Diabetes Mellitus in Adolescents and Young Adults