Korean J healthc assoc Infect Control Prev.
2023 Jun;28(1):172-177. 10.14192/kjicp.2023.28.1.172.
An Outbreak of Campylobacter Jejuni Involving Healthcare Workers Detected by COVID-19 Healthcare Worker Symptom Surveillance
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 2Department of Infection Control and Prevention, Gachon University Gil Medical Center, Incheon, Korea
- KMID: 2543148
- DOI: http://doi.org/10.14192/kjicp.2023.28.1.172
Abstract
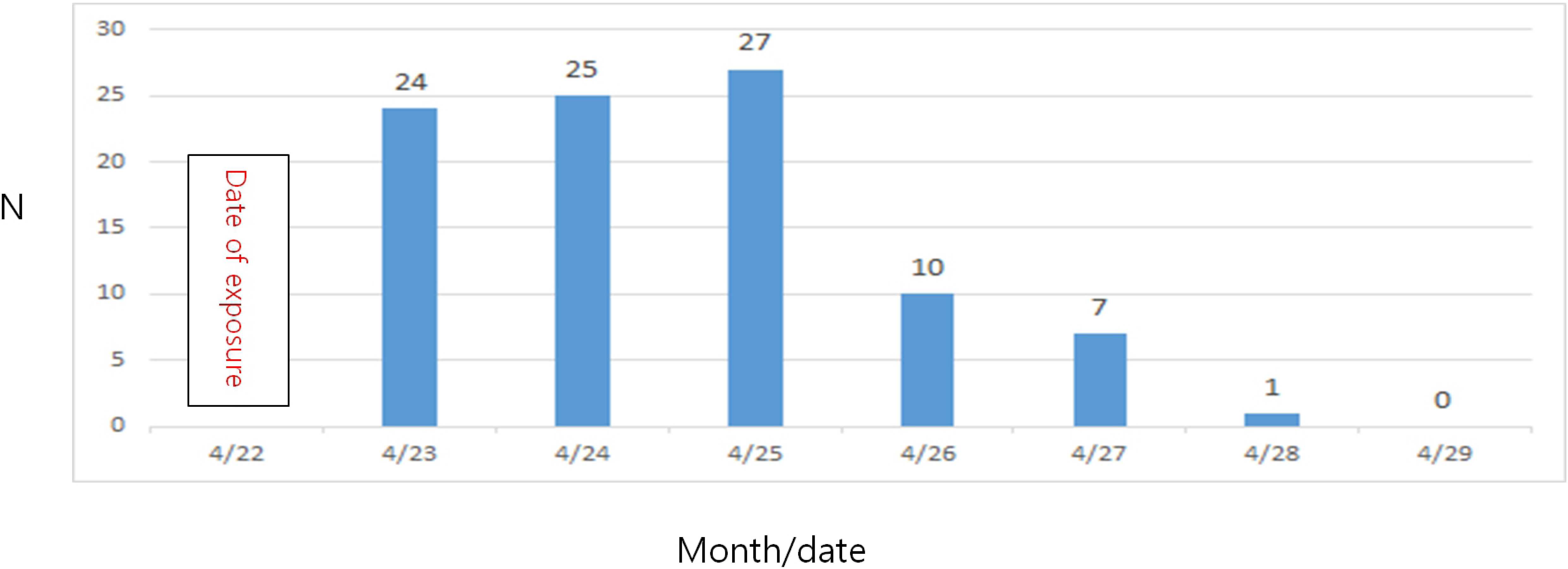
- We identified an outbreak of Campylobacter Jejuni enteritis through coronavirus infection 2019 (COVID-19), healthcare worker (HCW) symptom surveillance, which identified 15 HCWs with fever and diarrhea who were tested for COVID-19 on the same day. COVID-19 monitoring revealed that 15 employees with fever and diarrhea were tested for the virus, of whom two were hospitalized with fever, abdominal pain, and diarrhea. Stool cultures confirmed that C. jejunii was the causative agent of gastroenteritis in these patients. An outbreak of C. jejunii among HCWs was suspected, and an epidemiological investigation was initiated. The symptomatic HCWs had consumed lunch from the same cafeteria on the same day within the incubation period. Based on the results of the epidemiological investigation, 105 out of 2,173 HCWs (11 HCWs who had A-type lunch and 94 who had B-type lunch) reported symptoms of gastroenteritis, with an incidence of 4.8%. Meal B, specifically the pork dumpling, was presumed to have been contaminated. We identified a Campylobacter outbreak among HCWs through a COVID-19 HCW surveillance system. Moreover, the outbreak was first recognized through the COVID-19 HCW surveillance system. Improvements in food storage and cultural methods of food preservation are required. Increasing awareness among HCWs of the possibility of contracting various diseases other than COVID-19 when treating patients with fever is critical to the early recognition of outbreaks and prevention of missing an outbreak.
Keyword
Figure
Reference
-
1. Skirrow MB. 1991; Epidemiology of Campylobacter enteritis. Int J Food Microbiol. 12:9–16. DOI: 10.1016/0168-1605(91)90044-P. PMID: 2018709.
Article2. Trompette M, Le Guilloux L, Souply L, Denis B, Tsouria A, Garrec H, et al. 2019; Increased incidence of Campylobacter enteritis and their quinolone resistance between 2010 and 2015: results of a French national observatory conducted in 21 general hospitals (CHG). Clin Res Hepatol Gastroenterol. 43:338–45. DOI: 10.1016/j.clinre.2018.10.015. PMID: 30528512.
Article3. Kim NO, Jung SM, Na HY, Chung GT, Yoo CK, Seong WK, et al. 2015; Enteric bacteria isolated from diarrheal patients in Korea in 2014. Osong Public Health Res Perspect. 6:233–40. DOI: 10.1016/j.phrp.2015.07.005. PMID: 26473090. PMCID: PMC4588440.
Article4. Cho SH, Shin HH, Choi YH, Park MS, Lee BK. 2008; Enteric bacteria isolated from acute diarrheal patients in the Republic of Korea between the year 2004 and 2006. J Microbiol. 46:325–30. DOI: 10.1007/s12275-008-0015-4. PMID: 18604503.
Article5. Oh YI, Seo KW, Kim DH, Cheon DS. 2021; Prevalence, co-infection and seasonality of fecal enteropathogens from diarrheic cats in the Republic of Korea (2016-2019): a retrospective study. BMC Vet Res. 17:367. DOI: 10.1186/s12917-021-03075-6. PMID: 34852811. PMCID: PMC8633091.6. Yu JH, Kim NY, Cho NG, Kim JH, Kang YA, Lee HG. 2010; Epidemiology of Campylobacter jejuni outbreak in a middle school in Incheon, Korea. J Korean Med Sci. 25:1595–600. DOI: 10.3346/jkms.2010.25.11.1595. PMID: 21060748. PMCID: PMC2966996.
Article7. Taylor DN, Porter BW, Williams CA, Miller HG, Bopp CA, Blake PA. 1982; Campylobacter enteritis: a large outbreak traced to commercial raw milk. West J Med. 137:365–9. PMID: 7179958. PMCID: PMC1274150.8. Kaakoush NO, Castaño-Rodríguez N, Mitchell HM, Man SM. 2015; Global epidemiology of Campylobacter infection. Clin Microbiol Rev. 28:687–720. DOI: 10.1128/CMR.00006-15. PMID: 26062576. PMCID: PMC4462680.
Article9. Im S. Fever symptoms delays in emergency patient care... Get timely emergency care. Medigatenews. https://medigatenews.com/news/922029323. (Updated on 16 October 2021).10. Youn JH. "Wait for PCR results"... Chinese outrage over the death of a 1-year-old infant who missed emergency care. Seoul Economics. https://www.sedaily.com/NewsView/265UOGCT25. (Updated on 5 May 2022).11. Korea Disease Control. 2022. Foodborne infectious disease management guidelines. Korea Disease Control and Prevention Agency;Cheongju: p. 52–58.12. Sullivan SG, Carlson S, Cheng AC, Chilver MB, Dwyer DE, Irwin M, et al. 2020; Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill. 25:2001847. Erratum in: Euro Surveill 2021;26:210527e. DOI: 10.2807/1560-7917.ES.2020.25.47.2001847. PMID: 33243355.
Article13. Ahn SY, Park JY, Lim IS, Chae SA, Yun SW, Lee NM, et al. 2021; Changes in the occurrence of gastrointestinal infections after COVID-19 in Korea. J Korean Med Sci. 36:e180. DOI: 10.3346/jkms.2021.36.e180. PMID: 34155841. PMCID: PMC8216988.
Article14. Yoo M, Chung SH, Park YS, Oh IH, Chae WY, Kim SH, et al. 2020; Clinical characteristics of Campylobacter enterocolitis in Korean adults: a retrospective study at a single center. Korean J Gastroenterol. 75:188–97. DOI: 10.4166/kjg.2020.75.4.188. PMID: 32326685.
Article15. Bourdichon F, Arias E, Babuchowski A, Bückle A, Bello FD, Dubois A, et al. 2021; The forgotten role of food cultures. FEMS Microbiol Lett. 368:fnab085. DOI: 10.1093/femsle/fnab085. PMID: 34223876. PMCID: PMC8397475.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Burnout among Healthcare Workers during COVID-19 Pandemic
- Hospital Infection Control Practice in the COVID-19 Era: An Experience of University Affiliated Hospital
- Factors Affecting Fear of COVID-19 Infection in Healthcare Workers in COVID-19 Dedicated Teams: Focus on Professional Quality of Life
- COVID-19 and MERS Infections in Healthcare Workers in Korea
- COVID-19 Outbreak and Its Association with Healthcare Workers' Emotional Stress: a Cross-Sectional Study