Korean J healthc assoc Infect Control Prev.
2023 Jun;28(1):113-125. 10.14192/kjicp.2023.28.1.113.
Epidemiology of Catheter-related Bloodstream Infections in Neonatal Intensive Care Units: A Rapid Systematic Literature Review
- Affiliations
-
- 1Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea
- 2College of Nursing, Seoul National University, Seoul, Korea
- 3Department of Pediatrics, Korea University Anam Hospital, Seoul, Korea
- 4Allergy and Immunology Center, Korea University, Seoul, Korea
- 5Institute of Nano, Regeneration, Reconstruction, Korea University College of Medicine, Korea University, Seoul, Korea
- KMID: 2543142
- DOI: http://doi.org/10.14192/kjicp.2023.28.1.113
Abstract
- Background
Catheter-related bloodstream infections (CRBSIs) are serious complications in neonatal intensive care units (NICUs). We aimed to assess the incidence of CRBSIs in NICUs worldwide and describe the causative organisms.
Methods
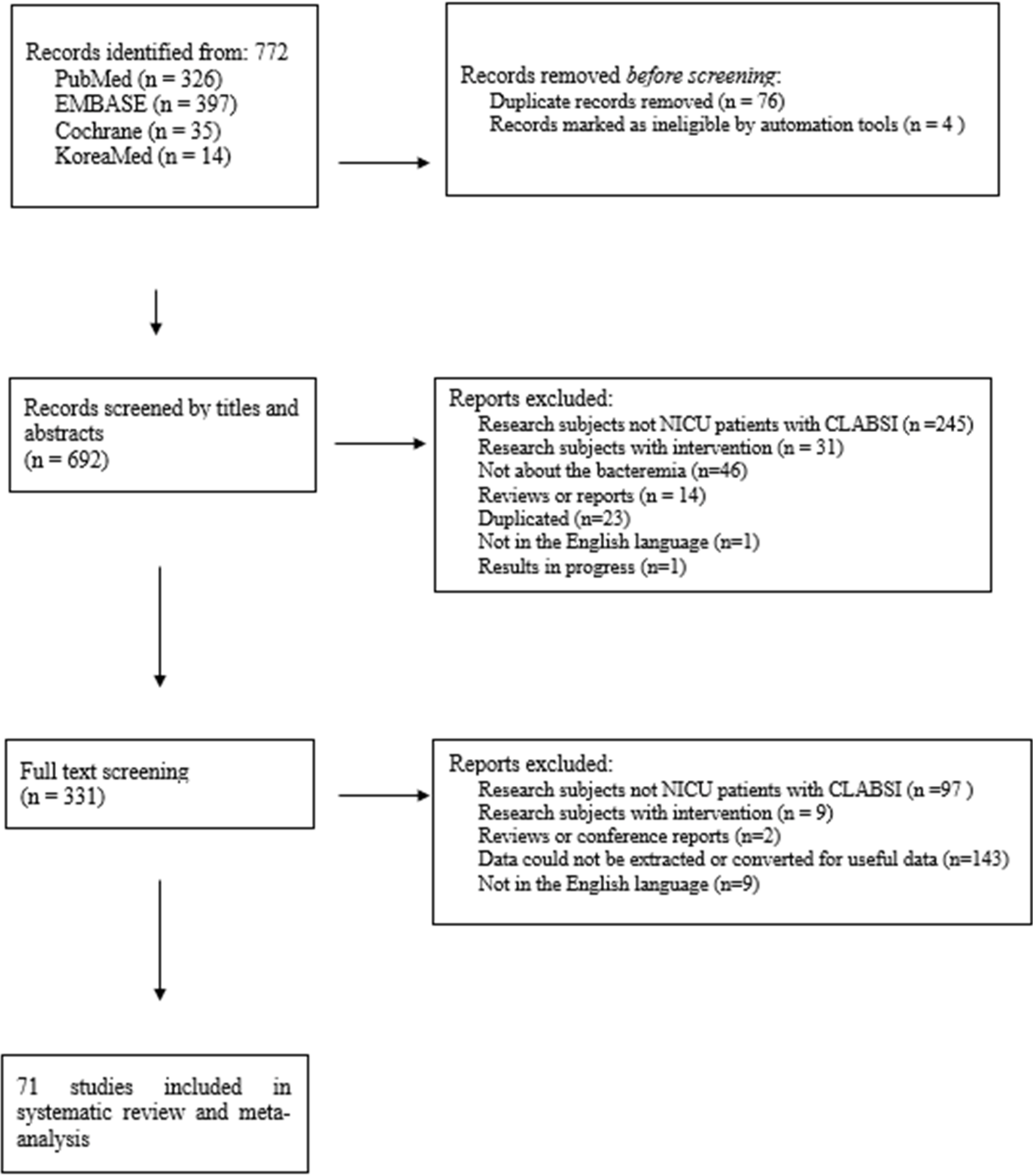
We searched PubMed, EMBASE, Cochrane, and KoreaMed databases. We included studies on CRBSIs in NICU settings with data on bacteremia. We performed a random-effects meta-analysis on CRBSI incidence in NICUs, stratified the data according to WHO regions. We compiled data on underlying organisms.
Results
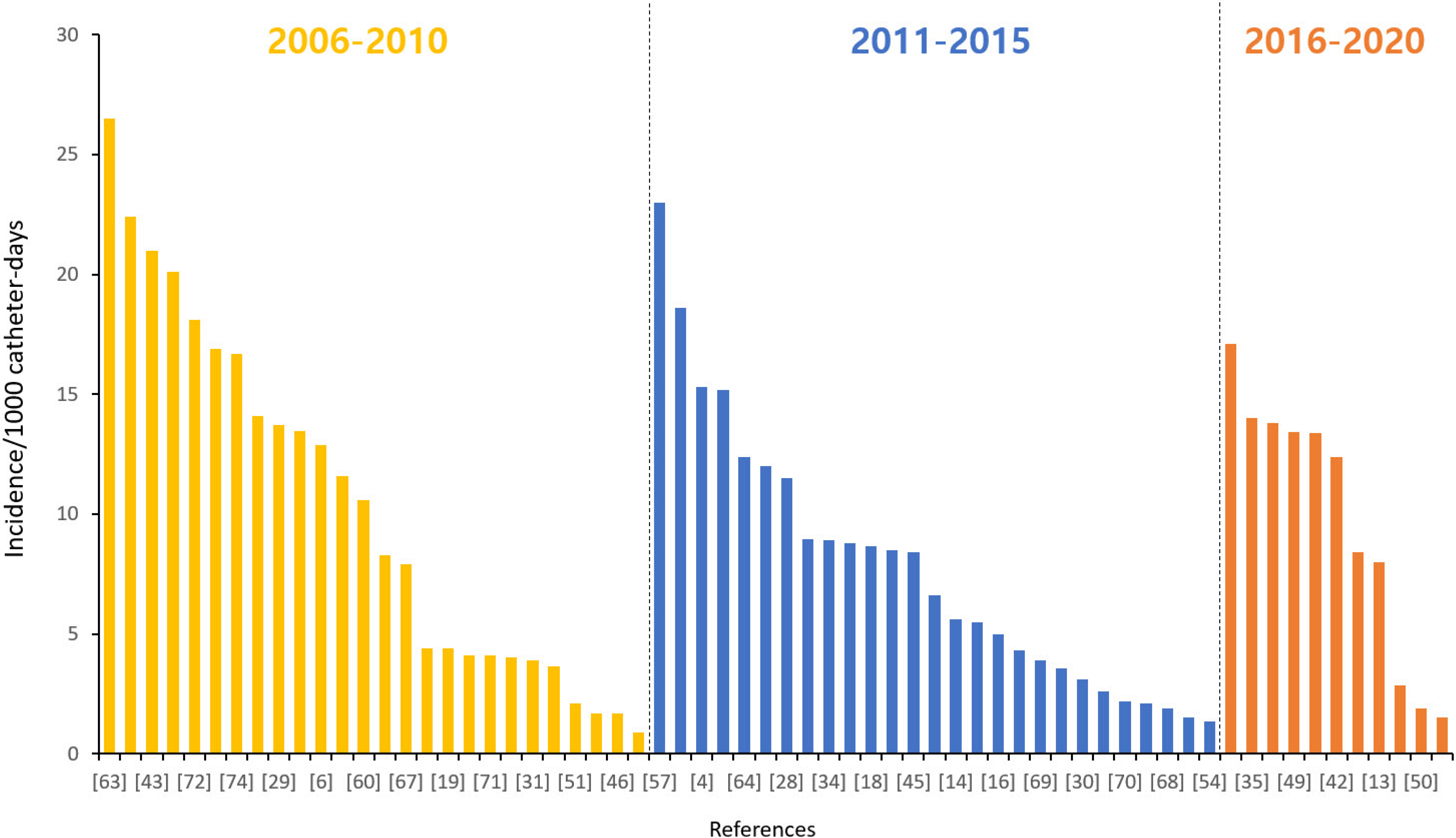
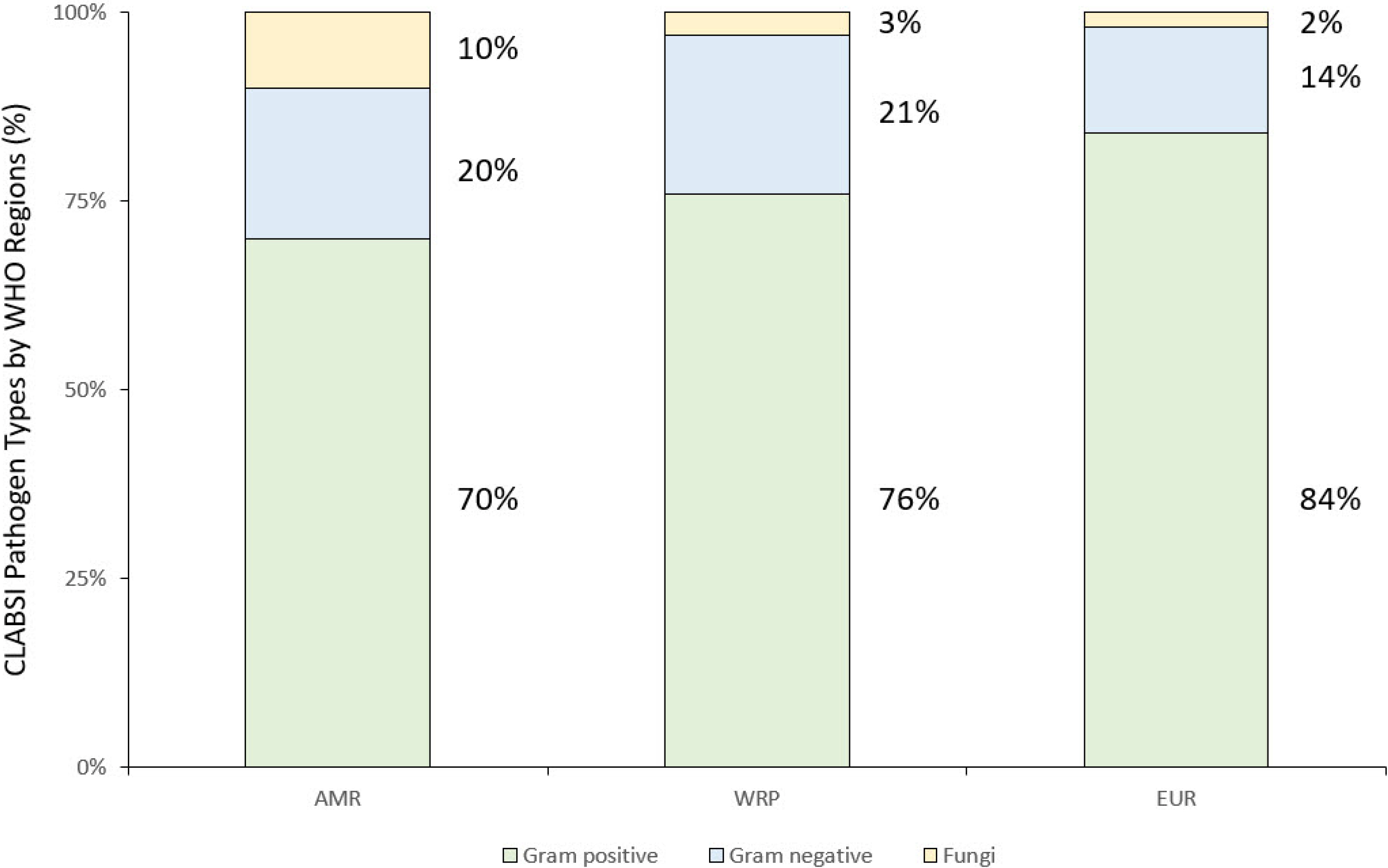
Of the 692 studies identified, 71 published between 2011 and 2022 were considered eligible. The pooled incidence of CRBSI per 1000 catheter days in NICUs was 8.66 (95% confidence interval [CI], 7.19; 10.12). Stratifying by WHO regions, the CRBSI incidence per 1000 catheter days was 10.38 (95% CI, 3.86; 16.90) in the Eastern Mediterranean Region (EMR), 11.77 (95% CI, 9.20; 14.35) in the European Union Region (EUR), 5.94 (95% CI, 3.87; 8.00) in the Western Pacific Region (WPR), and 6.71 (95% CI, 4.39; 9.03) in the Region from the Americas (AMR). Of the 2887 bacterial strains, 73.4% (n=2118) were gram-positive bacteria, 18.9% (n=547) were gram-negative bacteria, and 7.8% (n=225) were fungi. Coagulasenegative Staphylococci (n=1380, 65.2%) were the most common pathogen among the grampositive types, followed by Staphylococcus aureus (n=318, 15%). Among the CRBSI gramnegative cultures, Klebsiella spp. (n=201, 36.7%) was the primary pathogen.
Conclusion
We found a substantial burden of CRBSIs in NICUs across the globe. Our findings highlight the need to improve the implementation of global and local strategies to reduce CRBSIs in NICUs.
Keyword
Figure
Reference
-
1. Kochanowicz JF, Nowicka A, Al-Saad SR, Karbowski LM, Gadzinowski J, Szpecht D. 2022; Catheter-related bloodstream infections in infants hospitalized in neonatal intensive care units: a single center study. Sci Rep. 12:13679. DOI: 10.1038/s41598-022-17820-w. PMID: 35953522. PMCID: PMC9372030.
Article2. Singh L, Das S, Bhat VB, Plakkal N. 2018; Early neurodevelopmental outcome of very low birthweight neonates with culture-positive blood stream infection: a prospective cohort study. Cureus. 10:e3492. DOI: 10.7759/cureus.3492. PMID: 30648034. PMCID: PMC6318141.
Article3. Fleischmann C, Reichert F, Cassini A, Horner R, Harder T, Markwart R, et al. 2021; Global incidence and mortality of neonatal sepsis: a systematic review and meta-analysis. Arch Dis Child. 106:745–52. DOI: 10.1136/archdischild-2020-320217. PMID: 33483376. PMCID: PMC8311109.
Article4. Al-Mousa HH, Omar AA, Rosenthal VD, Salama MF, Aly NY, El-Dossoky Noweir M, et al. 2016; Device-associated infection rates, bacterial resistance, length of stay, and mortality in Kuwait: International Nosocomial Infection Consortium findings. Am J Infect Control. 44:444–9. DOI: 10.1016/j.ajic.2015.10.031. PMID: 26775929.
Article5. Almeida CC, Pissarra da Silva SMS, Flor de Lima Caldas de Oliveira FSD, Guimarães Pereira Areias MHF. 2017; Nosocomial sepsis: evaluation of the efficacy of preventive measures in a level-III neonatal intensive care unit. J Matern Fetal Neonatal Med. 30:2036–41. DOI: 10.1080/14767058.2016.1236245. PMID: 27628652.
Article6. Arnts IJ, Schrijvers NM, van der Flier M, Groenewoud JM, Antonius T, Liem KD. 2015; Central line bloodstream infections can be reduced in newborn infants using the modified Seldinger technique and care bundles of preventative measures. Acta Paediatr. 104:e152–7. DOI: 10.1111/apa.12915. PMID: 25545676.
Article7. Bannatyne M, Smith J, Panda M, Abdel-Latif ME, Chaudhari T. 2018; Retrospective cohort analysis of central line associated blood stream infection following introduction of a central line bundle in a neonatal intensive care unit. Int J Pediatr. 2018:4658181. DOI: 10.1155/2018/4658181. PMID: 30245727. PMCID: PMC6139226.
Article8. Bierlaire S, Danhaive O, Carkeek K, Piersigilli F. 2021; How to minimize central line-associated bloodstream infections in a neonatal intensive care unit: a quality improvement intervention based on a retrospective analysis and the adoption of an evidence-based bundle. Eur J Pediatr. 180:449–60. DOI: 10.1007/s00431-020-03844-9. PMID: 33083900.
Article9. Blanchard AC, Fortin E, Rocher I, Moore DL, Frenette C, Tremblay C, et al. 2013; Central line-associated bloodstream infection in neonatal intensive care units. Infect Control Hosp Epidemiol. 34:1167–73. DOI: 10.1086/673464. PMID: 24113600.
Article10. Bolat F, Uslu S, Bolat G, Comert S, Can E, Bulbul A, et al. 2012; Healthcare-associated infections in a Neonatal Intensive Care Unit in Turkey. Indian Pediatr. 49:951–7. DOI: 10.1007/s13312-012-0249-4. PMID: 22791673.
Article11. Boutaric E, Gilardi M, Cécile W, Fléchelles O. 2013; [Impact of clinical practice guidelines on the incidence of bloodstream infections related to peripherally inserted central venous catheter in preterm infants]. Arch Pediatr. 20:130–6. French. DOI: 10.1016/j.arcped.2012.11.001. PMID: 23245862.12. Bunni L, Brunskill K, Parmar R, Townley P, Yoxall B. 2014; Reducing catheter associated blood stream infections in neonatal intensive care. Arch Dis Child Fetal Neonatal Ed. 99(Suppl 1):A71. DOI: 10.1136/archdischild-2014-306576.202.13. Cabrera DM, Cuba FK, Hernández R, Prevost-Ruiz Y. 2021; Incidence and risk factors of central line catheter-related bloodstream infections. Rev Peru Med Exp Salud Publica. 38:95–100. DOI: 10.17843/rpmesp.2021.381.5108. PMID: 34190932.14. Callejas A, Osiovich H, Ting JY. 2016; Use of peripherally inserted central catheters (PICC) via scalp veins in neonates. J Matern Fetal Neonatal Med. 29:3434–8. DOI: 10.3109/14767058.2016.1139567. PMID: 26754595.
Article15. Chandonnet CJ, Kahlon PS, Rachh P, Degrazia M, Dewitt EC, Flaherty KA, et al. 2013; Health care failure mode and effect analysis to reduce NICU line-associated bloodstream infections. Pediatrics. 131:e1961–9. DOI: 10.1542/peds.2012-3293. PMID: 23690523.
Article16. Cheng HY, Lu CY, Huang LM, Lee PI, Chen JM, Chang LY. 2016; Increased frequency of peripheral venipunctures raises the risk of central-line associated bloodstream infection in neonates with peripherally inserted central venous catheters. J Microbiol Immunol Infect. 49:230–6. DOI: 10.1016/j.jmii.2014.06.001. PMID: 25066708.
Article17. Cheong SM, Totsu S, Nakanishi H, Uchiyama A, Kusuda S. 2016; Outcomes of peripherally inserted double lumen central catheter in very low birth weight infants. J Neonatal Perinatal Med. 9:99–105. DOI: 10.3233/NPM-16915054. PMID: 27002262.
Article18. Cleves D, Pino J, Patiño JA, Rosso F, Vélez JD, Pérez P. 2018; Effect of chlorhexidine baths on central-line-associated bloodstream infections in a neonatal intensive care unit in a developing country. J Hosp Infect. 100:e196–9. DOI: 10.1016/j.jhin.2018.03.022. PMID: 29588187.
Article19. Dumpa V, Adler B, Allen D, Bowman D, Gram A, Ford P, et al. 2019; Reduction in central line-associated bloodstream infection rates after implementations of infection control measures at a level 3 neonatal intensive care unit. Am J Med Qual. 34:488–93. DOI: 10.1177/1062860619873777. PMID: 31479293.
Article20. Erdei C, McAvoy LL, Gupta M, Pereira S, McGowan EC. 2015; Is zero central line-associated bloodstream infection rate sustainable? A 5-year perspective. Pediatrics. 135:e1485–93. DOI: 10.1542/peds.2014-2523. PMID: 25986020.
Article21. Ereno IL, Yeo CL. 2016; Umbilical venous catheter (UVC) use in theneonates: the Singapore general hospital experience. J Paediatr Child Health. 52(S2):32–3.22. Flidel-Rimon O, Guri A, Levi D, Ciobotaro P, Oved M, Shinwell ES. 2019; Reduction of hospital-acquired infections in the neonatal intensive care unit: a long-term commitment. Am J Infect Control. 47:1002–5. DOI: 10.1016/j.ajic.2019.01.001. PMID: 30850254.
Article23. Fontela PS, Platt RW, Rocher I, Frenette C, Moore D, Fortin E, et al. 2012; Epidemiology of central line-associated bloodstream infections in Quebec intensive care units: a 6-year review. Am J Infect Control. 40:221–6. DOI: 10.1016/j.ajic.2011.04.008. PMID: 21824682.
Article24. Freeman JJ, Gadepalli SK, Siddiqui SM, Jarboe MD, Hirschl RB. 2015; Improving central line infection rates in the neonatal intensive care unit: effect of hospital location, site of insertion, and implementation of catheter-associated bloodstream infection protocols. J Pediatr Surg. 50:860–3. DOI: 10.1016/j.jpedsurg.2015.02.001. PMID: 25783394. PMCID: PMC4824061.
Article25. Freitas FTM, Araujo AFOL, Melo MIS, Romero GAS. 2019; Late-onset sepsis and mortality among neonates in a Brazilian Intensive Care Unit: a cohort study and survival analysis. Epidemiol Infect. 147:e208. DOI: 10.1017/S095026881900092X. PMID: 31364533. PMCID: PMC6624867.
Article26. Gadallah MA, Aboul Fotouh AM, Habil IS, Imam SS, Wassef G. 2014; Surveillance of health care-associated infections in a tertiary hospital neonatal intensive care unit in Egypt: 1-year follow-up. Am J Infect Control. 42:1207–11. DOI: 10.1016/j.ajic.2014.07.020. PMID: 25238664.
Article27. Gerver SM, Mihalkova M, Bion JF, Wilson APR, Chudasama D, Johnson AP, et al. 2020; Surveillance of bloodstream infections in intensive care units in England, May 2016-April 2017: epidemiology and ecology. J Hosp Infect. 106:1–9. DOI: 10.1016/j.jhin.2020.05.010. PMID: 32422311.
Article28. Greenhalgh M, Gordon A. 2014; Risk of CLABSI in neonates by PICC line dwell time. J Paediatr Child Health. 50(Suppl 1):86.29. Hei MY, Zhang XC, Gao XY, Zhao LL, Wu ZX, Tian L, et al. 2012; Catheter-related infection and pathogens of umbilical venous catheterization in a neonatal intensive care unit in China. Am J Perinatol. 29:107–14. DOI: 10.1055/s-0031-1295650. PMID: 22131046.
Article30. Helder OK, van Rosmalen J, van Dalen A, Schafthuizen L, Vos MC, Flint RB, et al. 2020; Effect of the use of an antiseptic barrier cap on the rates of central line-associated bloodstream infections in neonatal and pediatric intensive care. Am J Infect Control. 48:1171–8. DOI: 10.1016/j.ajic.2019.11.026. PMID: 31948717.
Article31. Hocevar SN, Edwards JR, Horan TC, Morrell GC, Iwamoto M, Lessa FC. 2012; Device-associated infections among neonatal intensive care unit patients: incidence and associated pathogens reported to the National Healthcare Safety Network, 2006-2008. Infect Control Hosp Epidemiol. 33:1200–6. DOI: 10.1086/668425. PMID: 23143356.
Article32. Holzmann-Pazgal G, Kubanda A, Davis K, Khan AM, Brumley K, Denson SE. 2012; Utilizing a line maintenance team to reduce central-line-associated bloodstream infections in a neonatal intensive care unit. J Perinatol. 32:281–6. DOI: 10.1038/jp.2011.91. PMID: 22011970.
Article33. Hussain AS, Ariff S. 2017; 5 Year surveillance of clabsi in a tertiary care private sector nicu in Pakistan. Antimicrob Resist Infect Control. 6(Suppl 3):P211.34. Hussain ASS, Ali SR, Ariff S, Arbab S, Demas S, Zeb J, et al. 2017; A protocol for quality improvement programme to reduce central line-associated bloodstream infections in NICU of low and middle income country. BMJ Paediatr Open. 1:e000008. DOI: 10.1136/bmjpo-2017-000008. PMID: 29637091. PMCID: PMC5842986.
Article35. Jansen SJ, Lopriore E, Berkhout RJM, van der Hoeven A, Saccoccia B, de Boer JM, et al. 2021; The effect of single-room care versus open-bay care on the incidence of bacterial nosocomial infections in pre-term neonates: a retrospective cohort study. Infect Dis Ther. 10:373–86. DOI: 10.1007/s40121-020-00380-9. PMCID: PMC7756131. PMID: 33355902.
Article36. Jansen SJ, van der Hoeven A, van den Akker T, Veenhof M, von Asmuth EGJ, Veldkamp KE, et al. 2022; A longitudinal analysis of nosocomial bloodstream infections among preterm neonates. Eur J Clin Microbiol Infect Dis. 41:1327–36. DOI: 10.1007/s10096-022-04502-8. PMID: 36178568. PMCID: PMC9556429.
Article37. Jeong IS, Park SM, Lee JM, Song JY, Lee SJ. 2013; Effect of central line bundle on central line-associated bloodstream infections in intensive care units. Am J Infect Control. 41:710–6. DOI: 10.1016/j.ajic.2012.10.010. PMID: 23394886.
Article38. Kim M, Choi S, Jung YH, Choi CW, Shin MJ, Kim ES, et al. 2021; Analysis of central line-associated bloodstream infection among infants in the neonatal intensive care unit: a single center study. Pediatr Infect Vaccine. 28:133–43. DOI: 10.14776/piv.2021.28.e18.
Article39. Kinoshita D, Hada S, Fujita R, Matsunaga N, Sakaki H, Ohki Y. 2019; Maximal sterile barrier precautions independently contribute to decreased central line-associated bloodstream infection in very low birth weight infants: a prospective multicenter observational study. Am J Infect Control. 47:1365–9. DOI: 10.1016/j.ajic.2019.05.006. PMID: 31266662.
Article40. Kleinlugtenbeld OJ, van Straaten HLM, van den Bos MI, Hemels MAC, d'Haens EJ. 2012; Reduction in central line associated bloodstream infections by introducing a quality improvement pathway 'clean line'. Arch Dis Child. 97(Suppl 2):A497. DOI: 10.1136/archdischild-2012-302724.1759.41. Kourkouni E, Kourlaba G, Chorianopoulou E, Tsopela GC, Kopsidas I, Spyridaki I, et al. 2018; Surveillance for central-line-associated bloodstream infections: accuracy of different sampling strategies. Infect Control Hosp Epidemiol. 39:1210–5. DOI: 10.1017/ice.2018.187. PMID: 30156182.
Article42. Kulali F, Çalkavur Ş, Oruç Y, Demiray N, Devrim İ. 2019; Impact of central line bundle for prevention of umbilical catheter-related bloodstream infections in a neonatal intensive care unit: a pre-post intervention study. Am J Infect Control. 47:387–90. DOI: 10.1016/j.ajic.2018.10.002. PMID: 30502109.
Article43. Leblebicioglu H, Erben N, Rosenthal VD, Atasay B, Erbay A, Unal S, et al. 2014; International Nosocomial Infection Control Consortium (INICC) national report on device-associated infection rates in 19 cities of Turkey, data summary for 2003-2012. Ann Clin Microbiol Antimicrob. 13:51. DOI: 10.1186/s12941-014-0051-3. PMID: 25403704. PMCID: PMC4255447.
Article44. Leistner R, Thürnagel S, Schwab F, Piening B, Gastmeier P, Geffers C. 2013; The impact of staffing on central venous catheter-associated bloodstream infections in preterm neonates - results of nation-wide cohort study in Germany. Antimicrob Resist Infect Control. 2:11. DOI: 10.1186/2047-2994-2-11. PMID: 23557510. PMCID: PMC3643825.
Article45. Leveillee A, Lapointe A, Lachance C, Descarries M, Autmizguine J, Dubois J, et al. 2018; Assessing effect of catheter type and position on central line-associated bloodstream infections in the NICU. Paediatr Child Health. 23(Suppl 1):e59. DOI: 10.1093/pch/pxy054.149. PMCID: PMC5961418.
Article46. Milstone AM, Reich NG, Advani S, Yuan G, Bryant K, Coffin SE, et al. 2013; Catheter dwell time and CLABSIs in neonates with PICCs: a multicenter cohort study. Pediatrics. 132:e1609–15. DOI: 10.1542/peds.2013-1645. PMID: 24218474. PMCID: PMC3838533.
Article47. Mohamed Cassim S, Skiffington C, Lucas C, Anand D. 2015; An improvement project to reduce central line associated blood stream infection (CLABSI) in newborn infants. Arch Dis Child. 100(Suppl 3):A238–9. DOI: 10.1136/archdischild-2015-308599.491.48. Nercelles P, Vernal S, Brenner P, Rivero P. 2015; [Risk of bacteremia associated with intravascular devices stratified by birth weight in born of a public hospital of high complexity: follow-up to seven years]. Rev Chilena Infectol. 32:278–82. Spanish. DOI: 10.4067/S0716-10182015000400004. PMID: 26230433.49. Nielsen CL, Zachariassen G, Holm KG. 2022; Central line-associated bloodstream infection in infants admitted to a level lllneonatal intensive care unit. Dan Med J. 69:A05210463. PMID: 35485786.50. Oh Y, Oh KW, Lim G. 2020; Routine scrubbing reduced central line associated bloodstream infection in NICU. Am J Infect Control. 48:1179–83. DOI: 10.1016/j.ajic.2020.02.011. PMID: 32312594.
Article51. Patrick SW, Kawai AT, Kleinman K, Jin R, Vaz L, Gay C, et al. 2014; Health care-associated infections among critically ill children in the US, 2007-2012. Pediatrics. 134:705–12. DOI: 10.1542/peds.2014-0613. PMID: 25201802.
Article52. Pavcnik-Arnol M, Kalan G. 2012; Risk factors for central-line associated bloodstream infections in critically ill neonates. Arch Dis Child. 97(Suppl 2):A169. DOI: 10.1136/archdischild-2012-302724.0582.53. Pharande P, Lindrea KB, Smyth J, Evans M, Lui K, Bolisetty S. 2018; Trends in late-onset sepsis in a neonatal intensive care unit following implementation of infection control bundle: a 15-year audit. J Paediatr Child Health. 54:1314–20. DOI: 10.1111/jpc.14078. PMID: 29888413.
Article54. Piazza AJ, Brozanski B, Provost L, Grover TR, Chuo J, Smith JR, et al. 2016; SLUG bug: quality improvement with orchestrated testing leads to NICU CLABSI reduction. Pediatrics. 137:e20143642. DOI: 10.1542/peds.2014-3642. PMID: 26702032.
Article55. Ponnusamy V, Venkatesh V, Curley A, Musonda P, Brown N, Tremlett C, et al. 2012; Segmental percutaneous central venous line cultures for diagnosis of catheter-related sepsis. Arch Dis Child Fetal Neonatal Ed. 97:F273–8. DOI: 10.1136/archdischild-2011-300822. PMID: 22174018.
Article56. Rallis D, Karagianni P, Papakotoula I, Nikolaidis N, Tsakalidis C. 2016; Significant reduction of central line-associated bloodstream infection rates in a tertiary neonatal unit. Am J Infect Control. 44:485–7. DOI: 10.1016/j.ajic.2015.10.040. PMID: 26717871.
Article57. Resende DS, Peppe AL, dos Reis H, Abdallah VO, Ribas RM, Gontijo Filho PP. 2015; Late onset sepsis in newborn babies: epidemiology and effect of a bundle to prevent central line associated bloodstream infections in the neonatal intensive care unit. Braz J Infect Dis. 19:52–7. DOI: 10.1016/j.bjid.2014.09.006. PMID: 25523073. PMCID: PMC9425250.
Article58. Rosenthal VD, Dueñas L, Sobreyra-Oropeza M, Ammar K, Navoa-Ng JA, de Casares AC, et al. 2013; Findings of the International Nosocomial Infection Control Consortium (INICC), part III: effectiveness of a multidimensional infection control approach to reduce central line-associated bloodstream infections in the neonatal intensive care units of 4 developing countries. Infect Control Hosp Epidemiol. 34:229–37. DOI: 10.1086/669511. PMID: 23388356.
Article59. Salm F, Schwab F, Geffers C, Gastmeier P, Piening B. 2016; The implementation of an evidence-based bundle for bloodstream infections in neonatal intensive care units in Germany: a controlled intervention study to improve patient safety. Infect Control Hosp Epidemiol. 37:798–804. DOI: 10.1017/ice.2016.72. PMID: 27045855.
Article60. Sanderson E, Bolisetty S, Bajuk B, Callander I, Abdel-Latif M, Lui K. 2012; Nosocomial sepsis in NICU - risks associated with duration and type of central venous catheters in NSW and the ACT. J Paediatr Child Health. 48(Suppl 1):132.61. Shalabi M, Adel M, Yoon E, Aziz K, Lee S, Shah PS. 2015; Risk of infection using peripherally inserted central and umbilical catheters in preterm neonates. Pediatrics. 136:1073–9. DOI: 10.1542/peds.2015-2710. PMID: 26574592.
Article62. Shepherd EG, Kelly TJ, Vinsel JA, Cunningham DJ, Keels E, Beauseau W, et al. 2015; Significant reduction of central-line associated bloodstream infections in a network of diverse neonatal nurseries. J Pediatr. 167:41–6.e1. DOI: 10.1016/j.jpeds.2015.03.046. PMID: 25917770.
Article63. Sinha AK, Murthy V, Nath P, Morris JK, Millar M. 2016; Prevention of late onset sepsis and central-line associated blood stream infection in preterm infants. Pediatr Infect Dis J. 35:401–6. DOI: 10.1097/INF.0000000000001019. PMID: 26629870.
Article64. Soares BN, Pissarra S, Rouxinol-Dias AL, Costa S, Guimarães H. 2018; Complications of central lines in neonates admitted to a level III Neonatal Intensive Care Unit. J Matern Fetal Neonatal Med. 31:2770–6. DOI: 10.1080/14767058.2017.1355902. PMID: 28707497.
Article65. Steiner M, Langgartner M, Cardona F, Waldhör T, Schwindt J, Haiden N, et al. 2015; Significant reduction of catheter-associated blood stream infections in preterm neonates after implementation of a care bundle focusing on simulation training of central line insertion. Pediatr Infect Dis J. 34:1193–6. DOI: 10.1097/INF.0000000000000841. PMID: 26186105.
Article66. Taylor JE, McDonald SJ, Earnest A, Buttery J, Fusinato B, Hovenden S, et al. 2017; A quality improvement initiative to reduce central line infection in neonates using checklists. Eur J Pediatr. 176:639–46. DOI: 10.1007/s00431-017-2888-x. PMID: 28283785.
Article67. Ting JY, Goh VS, Osiovich H. 2013; Reduction of central line-associated bloodstream infection rates in a neonatal intensive care unit after implementation of a multidisciplinary evidence-based quality improvement collaborative: a four-year surveillance. Can J Infect Dis Med Microbiol. 24:185–90. DOI: 10.1155/2013/781690. PMID: 24489559. PMCID: PMC3905000.
Article68. Wen J, Yu Q, Chen H, Chen N, Huang S, Cai W. 2017; Peripherally inserted central venous catheter-associated complications exert negative effects on body weight gain in neonatal intensive care units. Asia Pac J Clin Nutr. 26:1–5. DOI: 10.6133/apjcn.112015.07. PMID: 28049254.69. Wilder KA, Wall B, Haggard D, Epperson T. 2016; CLABSI reduction strategy: a systematic central line quality improvement initiative integrating line-rounding principles and a team approach. Adv Neonatal Care. 16:170–7. DOI: 10.1097/ANC.0000000000000259. PMID: 27200515.70. Worth LJ, Daley AJ, Spelman T, Bull AL, Brett JA, Richards MJ. 2018; Central and peripheral line-associated bloodstream infections in Australian neonatal and paediatric intensive care units: findings from a comprehensive Victorian surveillance network, 2008-2016. J Hosp Infect. 99:55–61. DOI: 10.1016/j.jhin.2017.11.021. PMID: 29222036.
Article71. Yalaz M, Altun-Köroğlu O, Ulusoy B, Yildiz B, Akisu M, Vardar F, et al. 2012; Evaluation of device-associated infections in a neonatal intensive care unit. Turk J Pediatr. 54:128–35. PMID: 22734298.72. Yumani DF, van den Dungen FA, van Weissenbruch MM. 2013; Incidence and risk factors for catheter-associated bloodstream infections in neonatal intensive care. Acta Paediatr. 102:e293–8. DOI: 10.1111/apa.12256. PMID: 23627968.
Article73. Zachariah P, Furuya EY, Edwards J, Dick A, Liu H, Herzig CT, et al. 2014; Compliance with prevention practices and their association with central line-associated bloodstream infections in neonatal intensive care units. Am J Infect Control. 42:847–51. DOI: 10.1016/j.ajic.2014.04.020. PMID: 25087136. PMCID: PMC4123126.74. Zhou Q, Lee SK, Hu XJ, Jiang SY, Chen C, Wang CQ, et al. 2015; Successful reduction in central line-associated bloodstream infections in a Chinese neonatal intensive care unit. Am J Infect Control. 43:275–9. DOI: 10.1016/j.ajic.2014.12.001. PMID: 25728154.
Article75. Cho HJ, Cho HK. 2019; Central line-associated bloodstream infections in neonates. Korean J Pediatr. 62:79–84. DOI: 10.3345/kjp.2018.07003. PMID: 30590002. PMCID: PMC6434225.
Article76. Bell T, O'Grady NP. 2017; Prevention of central line-associated bloodstream infections. Infect Dis Clin North Am. 31:551–9. DOI: 10.1016/j.idc.2017.05.007. PMID: 28687213. PMCID: PMC5666696.
Article77. Diaz JV, Riviello ED, Papali A, Adhikari NKJ, Ferreira JC. 2019; Global critical care: moving forward in resource-limited settings. Ann Glob Health. 85:3. DOI: 10.5334/aogh.2413. PMID: 30741504. PMCID: PMC7052346.
Article78. Hug L, Alexander M, You D, Alkema L. UN Inter-agency Group for Child Mortality Estimation. 2019; National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Health. 7:e710–20. Erratum in: Lancet Glob Health 2019;7:e1179. DOI: 10.1016/S2214-109X(19)30163-9. PMID: 31097275. PMCID: PMC6527519.
Article79. Saugstad OD. 2011; Reducing global neonatal mortality is possible. Neonatology. 99:250–7. DOI: 10.1159/000320332. PMID: 21088433.
Article80. Martinez AM, Khu DT, Boo NY, Neou L, Saysanasongkham B, Partridge JC. 2012; Barriers to neonatal care in developing countries: parents' and providers' perceptions. J Paediatr Child Health. 48:852–8. DOI: 10.1111/j.1440-1754.2012.02544.x. PMID: 22970681.
Article81. Markwart R, Saito H, Harder T, Tomczyk S, Cassini A, Fleischmann-Struzek C, et al. 2020; Epidemiology and burden of sepsis acquired in hospitals and intensive care units: a systematic review and meta-analysis. Intensive Care Med. 46:1536–51. DOI: 10.1007/s00134-020-06106-2. PMID: 32591853. PMCID: PMC7381455.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevention of Intravascular Catheter-Related Infections
- Catheter-related bloodstream infections in neonatal intensive care units
- Central line-associated bloodstream infections in neonates
- Nosocomial Infections in Intensive Care Unit: Epidemiology and Control Strategy
- Quality Improvement in Neonatal Intensive Care Units