Korean J healthc assoc Infect Control Prev.
2023 Jun;28(1):78-84. 10.14192/kjicp.2023.28.1.78.
A Survey of the Collection of Denominator Data in the Korean National Healthcare-associated Infections Surveillance System, Intensive Care Unit Module
- Affiliations
-
- 1Department of Internal Medicine, Inje University Ilsan Paik Hospital,Goyang, Korea
- 2Infection Control Office, Inje University Ilsan Paik Hospital,Goyang, Korea
- 3Department of Infectious Diseases, Ajou University School of Medicine, Suwon, Korea
- 4Infection Control Office, Korea University Guro Hospital, Seoul, Korea
- 5Department of Nursing, Soonchunhyang University College of Medicine, Cheonan, Korea
- 6Department of Nursing, The Catholic University of Korea College of Nursing, Seoul, Korea
- 7Infection Control Office, Inje University Sanggye Paik Hospital, Seoul, Korea
- 8Infection Control Team, Chungang University Hospital, Seoul, Korea
- 9Infection Control Office, Seoul National University Bundang Hospital, Sungnam, Korea
- KMID: 2543137
- DOI: http://doi.org/10.14192/kjicp.2023.28.1.78
Abstract
- Background
National surveillance data should be validated to identify data quality issues. Denominator data can substantially affect the healthcare-associated infection (HAI) rate; however, they are relatively overlooked compared to numerator data. We analysed the status of and problems with collecting denominator data by the Korean National Healthcare-associated Infections Surveillance System (KONIS).
Methods
This study was conducted in 21 (10.8%) of the 193 hospitals that participated in the KONIS ICU module between July 2016 and June 2017. A survey examined denominator data collection methods, such as patient days and device days of central lines and urinary catheters, between November and December 2017. The knowledge of central lines and urinary catheters specifically for KONIS reporting purposes, and the correct answer rate to questionnaires regarding specific situations related to the calculation of device days, were also evaluated.
Results
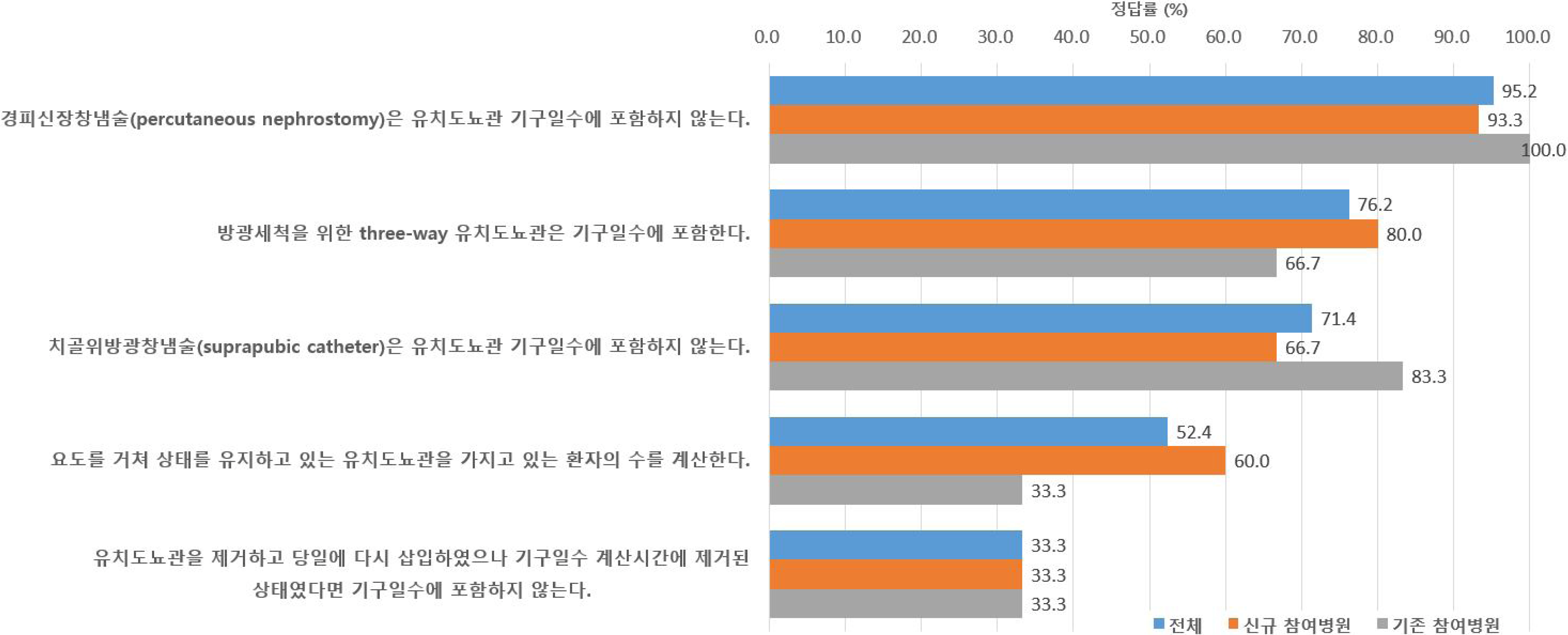
Counting the denominator data, the respective proportions using manual or electronic methods were 52.4% vs. 42.8% for patient days, 66.7% vs. 33.3% for central line days, and 61.9% vs. 38.1% for urinary catheter days. The rate of accurately understanding and responding to the case questions on device days through a survey was 19.0–81.0% for the central lines and 33.3–95.2% for the urinary catheters.
Conclusion
It is important to collect accurate denominator data in addition to numerator data to maintain the reliability of the national HAI surveillance data. Continued education of the surveillance personnel on the definition of denominator data and accurate data collection methods is required.
Figure
Reference
-
1. Korean National Healthcare-associated Infections Surveillance System. KONIS 2020 ICU manual. http://konis.cafe24.com/xe/manual/20922. (Updated on 5 November 2020).2. Korean National Healthcare-associated Infections Surveillance System. KONIS 2016 ICU manual. http://konis.cafe24.com/xe/index.php?mid=manual&page=2&document_srl=609. (Updated on 27 July 2018).3. Rich KL, Reese SM, Bol KA, Gilmartin HM, Janosz T. 2013; Assessment of the quality of publicly reported central line-associated bloodstream infection data in Colorado, 2010. Am J Infect Control. 41:874–9. DOI: 10.1016/j.ajic.2012.12.014. PMID: 23498552.
Article4. Kwak YG, Choi JY, Yoo HM, Lee SO, Kim HB, Han SH, et al. 2017; Validation of the Korean National Healthcare-associated Infections Surveillance System (KONIS): an intensive care unit module report. J Hosp Infect. 96:377–84. DOI: 10.1016/j.jhin.2017.04.003. PMID: 28545827.
Article5. Jeon MH, Kim TH, Kim SR, Chun HK, Han SH, Bang JH, et al. 2014; Korean Nosocomial Infections Surveillance system, intensive care unit module report: summary of data from July 2011 through June 2012. Korean J Nosocomial Infect Control. 19:52–63. DOI: 10.14192/kjnic.2014.19.2.52.
Article6. Kwak YG. Validation of the surveillance and reporting of healthcare-associated infection data to the Korean National Healthcare-associated Infectious Surveillance System (KONIS). https://library.nih.go.kr/ncmiklib/mlib/mlibViewReport.do?searchSubTarget=report&bibctrlno=7222220. (Updated on 12 March 2018).7. Centers for Disease Control. National Healthcare Safety Network (NHSN) external validation guidance and toolkit 2015. Appendix 2: surveillance surveys. https://www.cdc.gov/nhsn/pdfs/validation/archive/2015-nhsn-ev-guidance-p.pdf. (Updated on 1 January 2023).8. Backman LA, Nobert G, Melchreit R, Fekieta R, Dembry LM. 2014; Validation of the surveillance and reporting of central line-associated bloodstream infection denominator data. Am J Infect Control. 42:28–33. DOI: 10.1016/j.ajic.2013.06.014. PMID: 24176605.
Article9. Woeltje KF, Lin MY, Klompas M, Wright MO, Zuccotti G, Trick WE. 2014; Data requirements for electronic surveillance of healthcare-associated infections. Infect Control Hosp Epidemiol. 35:1083–91. DOI: 10.1086/677623. PMID: 25111915.
Article10. Wright MO, Fisher A, John M, Reynolds K, Peterson LR, Robicsek A. 2009; The electronic medical record as a tool for infection surveillance: successful automation of device-days. Am J Infect Control. 37:364–70. DOI: 10.1016/j.ajic.2008.11.003. PMID: 19269712.
Article11. Shelly MA, Concannon C, Dumyati G. 2011; Device use ratio measured weekly can reliably estimate central line-days for central line-associated bloodstream infection rates. Infect Control Hosp Epidemiol. 32:727–30. DOI: 10.1086/660860. PMID: 21666408.
Article12. Stevenson KB, Khan Y, Dickman J, Gillenwater T, Kulich P, Myers C, et al. 2008; Administrative coding data, compared with CDC/NHSN criteria, are poor indicators of health care-associated infections. Am J Infect Control. 36:155–64. DOI: 10.1016/j.ajic.2008.01.004. PMID: 18371510.
Article13. Tejedor SC, Garrett G, Jacob JT, Meyer E, Reyes MD, Robichaux C, et al. 2013; Electronic documentation of central venous catheter-days: validation is essential. Infect Control Hosp Epidemiol. 34:900–7. DOI: 10.1017/S0195941700033695. PMID: 23917903.
Article14. National Healthcare Safety Network. Bloodstream infection event (central line-associated bloodstream infection and non-central line associated bloodstream infection). NHSN patient safety component manual. http://www.cdc.gov/nhsn/PDFs/pscManual/4PSC_CLABScurrent.pdf. (Updated on 1 January 2023).15. Thompson ND, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Godine D, et al. 2015; Estimating central line-associated bloodstream infection incidence rates by sampling of denominator data: a prospective, multicenter evaluation. Am J Infect Control. 43:853–6. DOI: 10.1016/j.ajic.2015.03.031. PMID: 26004907. PMCID: PMC6498435.
Article16. Klevens RM, Tokars JI, Edwards J, Horan T. 2006; Sampling for collection of central line-day denominators in surveillance of healthcare-associated bloodstream infections. Infect Control Hosp Epidemiol. 27:338–42. DOI: 10.1086/503338. PMID: 16622809.
Article17. Thompson ND, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Godine D, et al. 2013; Evaluating the accuracy of sampling to estimate central line-days: simplification of the National Healthcare Safety Network surveillance methods. Infect Control Hosp Epidemiol. 34:221–8. DOI: 10.1086/669515. PMID: 23388355.
Article18. National Healthcare Safety Network. NHSN guidance for missing device-associated denominator data. https://www.cdc.gov/nhsn/pdfs/gen-support/MissingDenomData-508.pdf. (Updated on December 2021).
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Validation Study of Surveillance Data: Focus on the Korean National Healthcare-associated Infections Surveillance System (KONIS), Intensive Care Unit Module
- Prospective nationwide healthcare-associated infection surveillance system in South Korea
- Perspective of Nationwide Surveillance System for Healthcareassociated Infection in Neonatal Intensive Care Units
- Perspective of Nationwide Surveillance System for Surgical Site Infections
- Korean National Healthcare-associated Infections Surveillance System, Intensive Care Unit Module Report: Summary of Data from July 2020 through June 2021