Ann Surg Treat Res.
2023 Jun;104(6):313-324. 10.4174/astr.2023.104.6.313.
Effect of prehabilitation on patients with frailty undergoing colorectal cancer surgery: a systematic review and meta-analysis
- Affiliations
-
- 1Department of Rehabilitation Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 2Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2542795
- DOI: http://doi.org/10.4174/astr.2023.104.6.313
Abstract
- Purpose
The effect of prehabilitation in patients with frailty undergoing colorectal cancer surgery remains controversial. This meta-analysis aimed to assess the impact of prehabilitation before colorectal surgery on the functional outcomes and postoperative complications in patients with frailty undergoing colorectal cancer surgery.
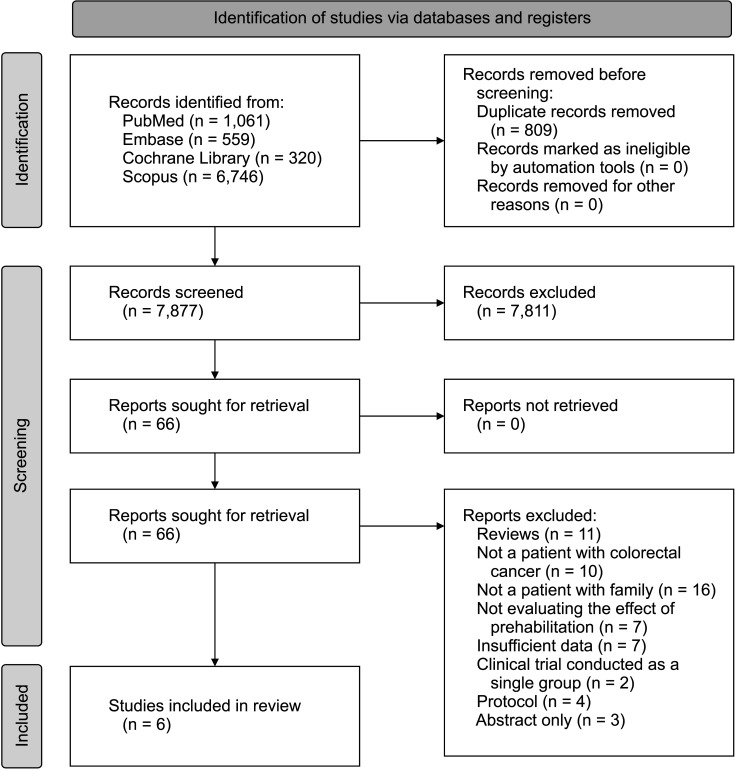
Methods
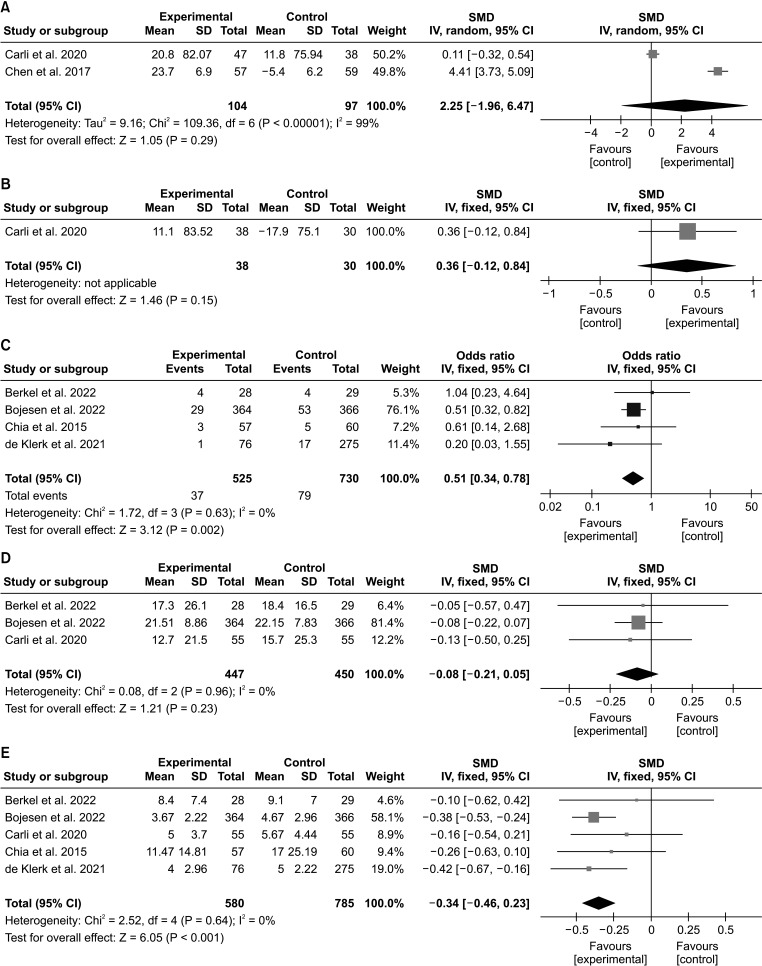
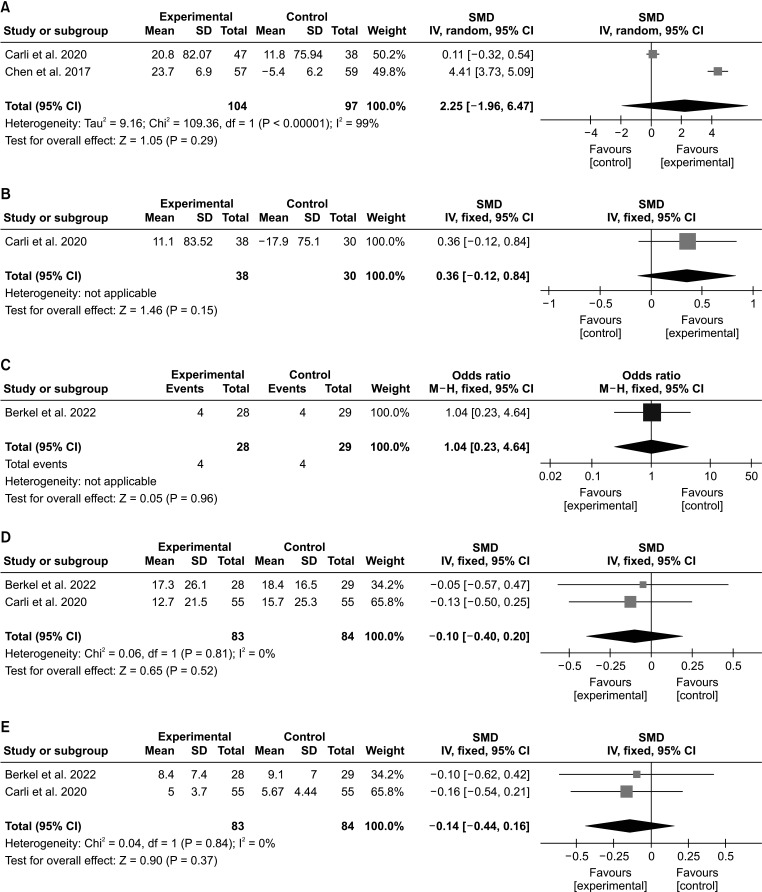
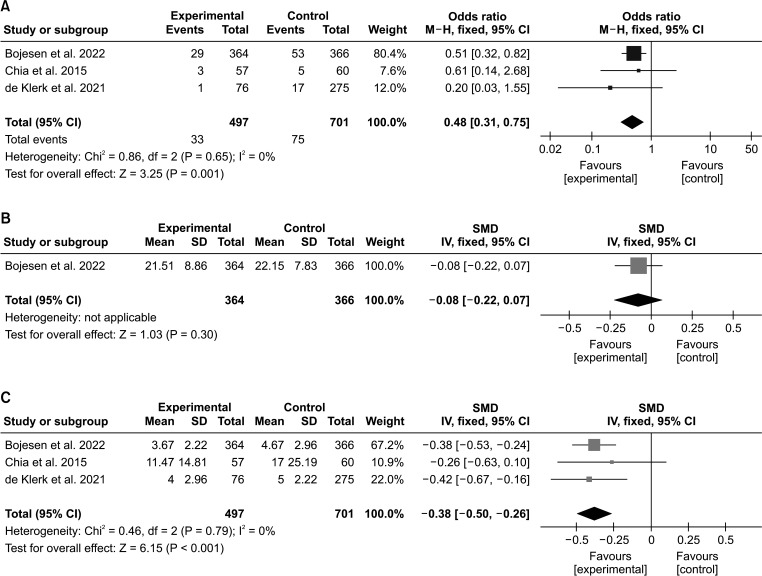
PubMed, EMBASE, Cochrane Library, and Scopus databases were searched for articles published up to November 9, 2022. We included randomized and non-randomized trials in which the effects of prehabilitation in patients with frailty undergoing colorectal cancer surgery were investigated against a control group. Data extracted for our metaanalysis included the 6-minute walk test (6MWT), postoperative incidence of complications (Clavien-Dindo classification ≥IIIa), comprehensive complication index (CCI), and length of stay (LOS) in the hospital.
Results
Compared with the control group, we found a significant improvement in the incidence of postoperative complications and shorter LOS in the hospital in the prehabilitation group. However, the 6MWT and CCI results showed no significant differences between the 2 groups.
Conclusion
Prehabilitation in patients with frailty who underwent colorectal cancer surgery improved the incidence of postoperative complications and LOS in the hospital. Hence, clinicians should consider conducting or recommending prehabilitation exercises prior to colorectal cancer surgery in patients with frailty.
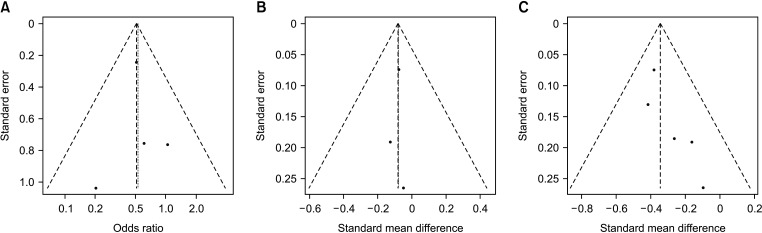
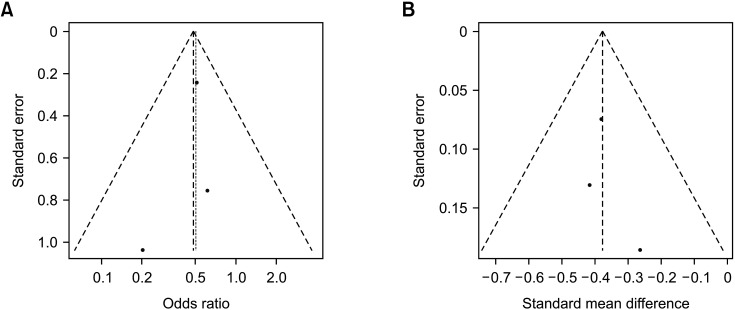
Figure
Cited by 1 articles
-
National cancer screening program for colorectal cancer in Korea
Seung Min Baik, Ryung-Ah Lee
Ann Surg Treat Res. 2023;105(6):333-340. doi: 10.4174/astr.2023.105.6.333.
Reference
-
1. Kocarnik JM, Compton K, Dean FE, Fu W, Gaw BL, et al. Global Burden of Disease 2019 Cancer Collaboration. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022; 8:420–444. PMID: 34967848.2. Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020; 70:145–164. PMID: 32133645.3. Keller DS, Reif de Paula T, Kiran RP, Nemeth SK. Evaluating the association of the new National Surgical Quality Improvement Program modified 5-factor frailty index with outcomes in elective colorectal surgery. Colorectal Dis. 2020; 22:1396–1405. PMID: 32291861.4. Zawadzki M, Krzystek-Korpacka M, Rząca M, Czarnecki R, Obuszko Z, Witkiewicz W. Colorectal surgery in elderly population. Pol Przegl Chir. 2018; 90:29–34.5. Martin D, Romain B, Pache B, Vuagniaux A, Guarnero V, Hahnloser D, et al. Physical activity and outcomes in colorectal surgery: a pilot prospective cohort study. Eur Surg Res. 2020; 61:23–33. PMID: 32492676.6. Michaud Maturana M, English WJ, Nandakumar M, Li Chen J, Dvorkin L. The impact of frailty on clinical outcomes in colorectal cancer surgery: a systematic literature review. ANZ J Surg. 2021; 91:2322–2329. PMID: 34013571.7. Al-Khamis A, Warner C, Park J, Marecik S, Davis N, Mellgren A, Nordenstam J, Kochar K. Modified frailty index predicts early outcomes after colorectal surgery: an ACS-NSQIP study. Colorectal Dis. 2019; 21:1192–1205. PMID: 31162882.8. Xue QL. The frailty syndrome: definition and natural history. Clin Geriatr Med. 2011; 27:1–15. PMID: 21093718.9. Carli F, Bousquet-Dion G, Awasthi R, Elsherbini N, Liberman S, Boutros M, et al. Effect of multimodal prehabilitation vs postoperative rehabilitation on 30-day postoperative complications for frail patients undergoing resection of colorectal cancer: a randomized clinical trial. JAMA Surg. 2020; 155:233–242. PMID: 31968063.10. Bousquet-Dion G, Awasthi R, Loiselle SÈ, Minnella EM, Agnihotram RV, Bergdahl A, et al. Evaluation of supervised multimodal prehabilitation programme in cancer patients undergoing colorectal resection: a randomized control trial. Acta Oncol. 2018; 57:849–859. PMID: 29327644.11. Berkel AE, Bongers BC, Kotte H, Weltevreden P, de Jongh FH, Eijsvogel MM, et al. Effects of community-based exercise prehabilitation for patients scheduled for colorectal surgery with high risk for postoperative complications: results of a randomized clinical trial. Ann Surg. 2022; 275:e299–e306. PMID: 33443905.12. Bojesen RD, Grube C, Buzquurz F, Miedzianogora RE, Eriksen JR, Gögenur I. Effect of modifying high-risk factors and prehabilitation on the outcomes of colorectal cancer surgery: controlled before and after study. BJS Open. 2022; 6:zrac029. PMID: 35639564.13. Chen BP, Awasthi R, Sweet SN, Minnella EM, Bergdahl A, Santa Mina D, et al. Four-week prehabilitation program is sufficient to modify exercise behaviors and improve preoperative functional walking capacity in patients with colorectal cancer. Support Care Cancer. 2017; 25:33–40. PMID: 27539131.14. Chia CL, Mantoo SK, Tan KY. ‘Start to finish trans-institutional transdisciplinary care’: a novel approach improves colorectal surgical results in frail elderly patients. Colorectal Dis. 2016; 18:O43–O50. PMID: 26500155.15. de Klerk M, van Dalen DH, Nahar-van Venrooij LM, Meijerink WJ, Verdaasdonk EG. A mult imodal prehabi litat ion program in high-risk patients undergoing elective resection for colorectal cancer: a retrospective cohort study. Eur J Surg Oncol. 2021; 47:2849–2856. PMID: 34103244.16. Argillander TE, Schäfer S, van Westreenen HL, Kamper A, van der Zaag-Loonen HJ, van Duijvendijk P, et al. The predictive value of preoperative frailty screening for postoperative outcomes in older patients undergoing surgery for non-metastatic colorectal cancer. J Geriatr Oncol. 2022; 13:888–891. PMID: 35339404.17. Assouline B, Cools E, Schorer R, Kayser B, Elia N, Licker M. Preoperative exercise training to prevent postoperative pulmonary complications in adults undergoing major surgery: a systematic review and meta-analysis with trial sequential analysis. Ann Am Thorac Soc. 2021; 18:678–688. PMID: 33030962.18. Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985; 132:919–923. PMID: 3978515.19. Du H, Newton PJ, Salamonson Y, Carrieri-Kohlman VL, Davidson PM. A review of the six-minute walk test: its implication as a self-administered assessment tool. Eur J Cardiovasc Nurs. 2009; 8:2–8. PMID: 18694656.20. Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013; 258:1–7. PMID: 23728278.21. Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014; 44:1428–1446. PMID: 25359355.22. Agarwala P, Salzman SH. Six-Minute Walk Test: clinical role, technique, coding, and reimbursement. Chest. 2020; 157:603–611. PMID: 31689414.23. Soares SM, Jannuzzi HP, Kassab MF, Nucci LB, Paschoal MA. Investigation of the immediate pre-operative physical capacity of patients scheduled for elective abdominal surgery using the 6-minute walk test. Physiotherapy. 2015; 101:292–297. PMID: 25721252.24. Awdeh H, Kassak K, Sfeir P, Hatoum H, Bitar H, Husari A. The SF-36 and 6-Minute Walk Test are significant predictors of complications after major surgery. World J Surg. 2015; 39:1406–1412. PMID: 25651952.25. Michael CM, Lehrer EJ, Schmitz KH, Zaorsky NG. Prehabilitation exercise therapy for cancer: a systematic review and meta-analysis. Cancer Med. 2021; 10:4195–4205. PMID: 34110101.26. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.27. Bolliger M, Kroehnert JA, Molineus F, Kandioler D, Schindl M, Riss P. Experiences with the standardized classification of surgical complications (Clavien-Dindo) in general surgery patients. Eur Surg. 2018; 50:256–261. PMID: 30546385.28. Yoon PD, Chalasani V, Woo HH. Use of Clavien-Dindo classification in reporting and grading complications after urological surgical procedures: analysis of 2010 to 2012. J Urol. 2013; 190:1271–1274. PMID: 23583859.29. Jin HY, Hong I, Bae JH, Lee CS, Han SR, Lee YS, et al. Predictive factors of high comprehensive complication index in colorectal cancer patients using Enhanced Recovery After Surgery protocol: role as a safety net in early discharge. Ann Surg Treat Res. 2021; 101:340–349. PMID: 34934761.30. Boeri L, Turetti M, Silvani C, Fulgheri I, Jannello LM, Garbagnati S, et al. The comprehensive complication index as a tool for reporting the burden of complications after mini-percutaneous nephrolithotomy: is it time to leave the Clavien-Dindo classification behind? World J Urol. 2022; 40:1829–1837. PMID: 35643945.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prehabilitation for medically frail patients undergoing surgery for epithelial ovarian cancer: a cost-effectiveness analysis
- An Introduction of the Systematic Review and Meta-Analysis
- Neurocognitive Effects of Chemotherapy for Colorectal Cancer: A Systematic Review and a Meta-Analysis of 11 Studies
- Systematic review and meta-analysis of cancer risks in relation to environmental waste incinerator emissions: a meta-analysis of case-control and cohort studies
- How to review and assess a systematic review and meta-analysis article: a methodological study (secondary publication)