Korean J Gastroenterol.
2023 May;81(5):221-225. 10.4166/kjg.2023.015.
Case Reports on Black Fungus of the Gastrointestinal Tract: A New Complication in COVID-19 Patients
- Affiliations
-
- 1Departments of Surgical Gastroenterology , Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
- 2Departments of Pathology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
- KMID: 2542789
- DOI: http://doi.org/10.4166/kjg.2023.015
Abstract
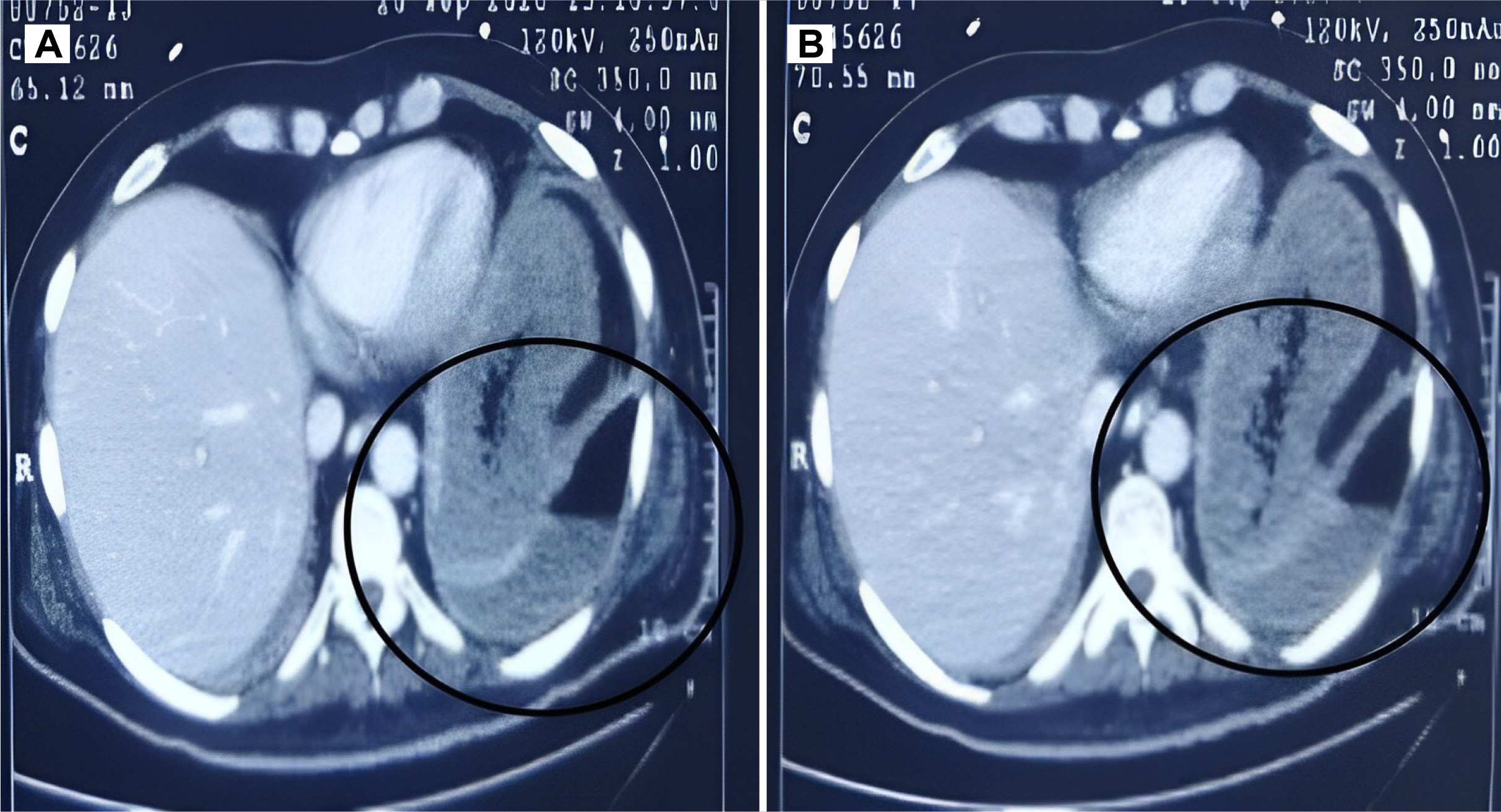
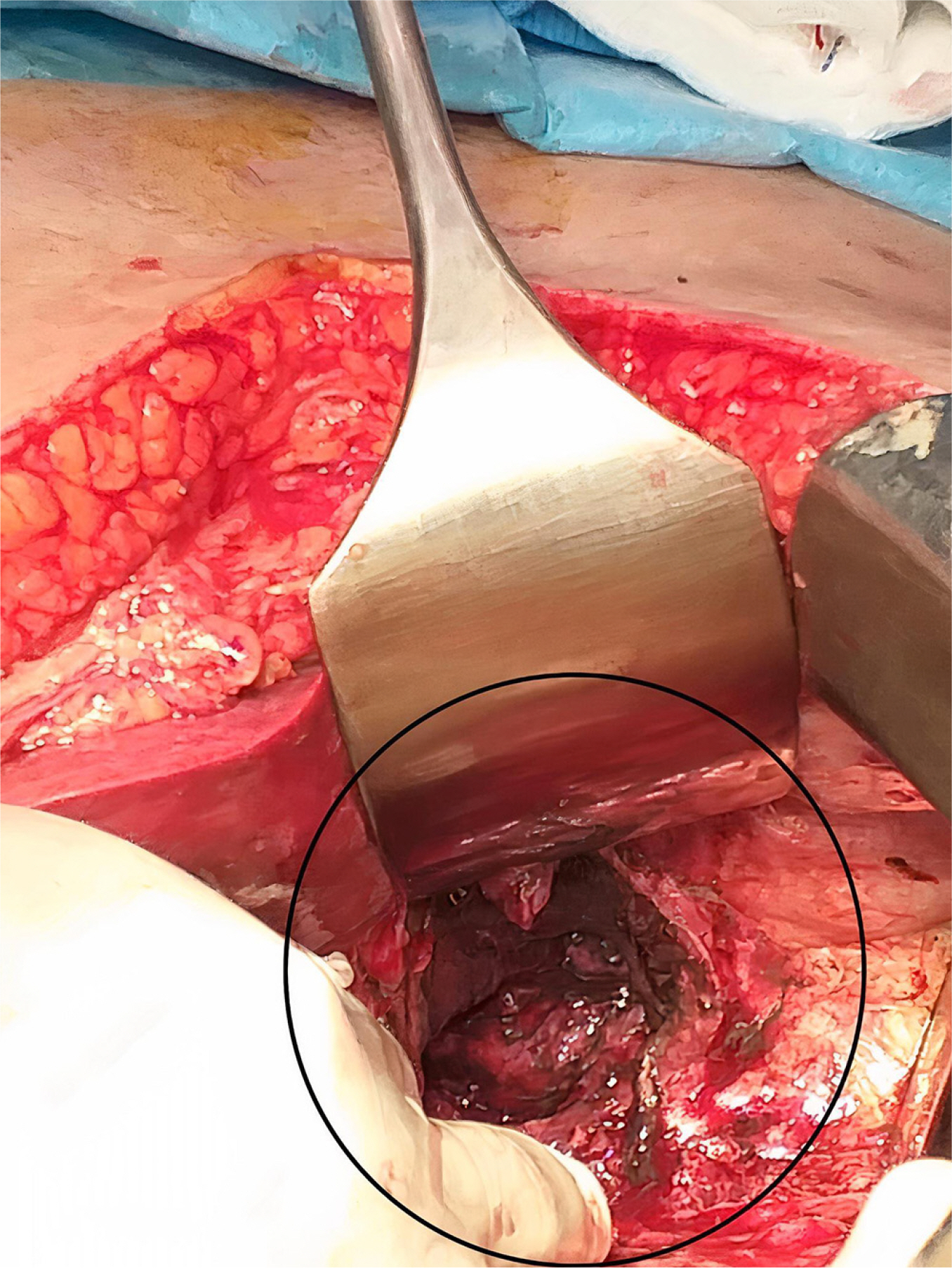
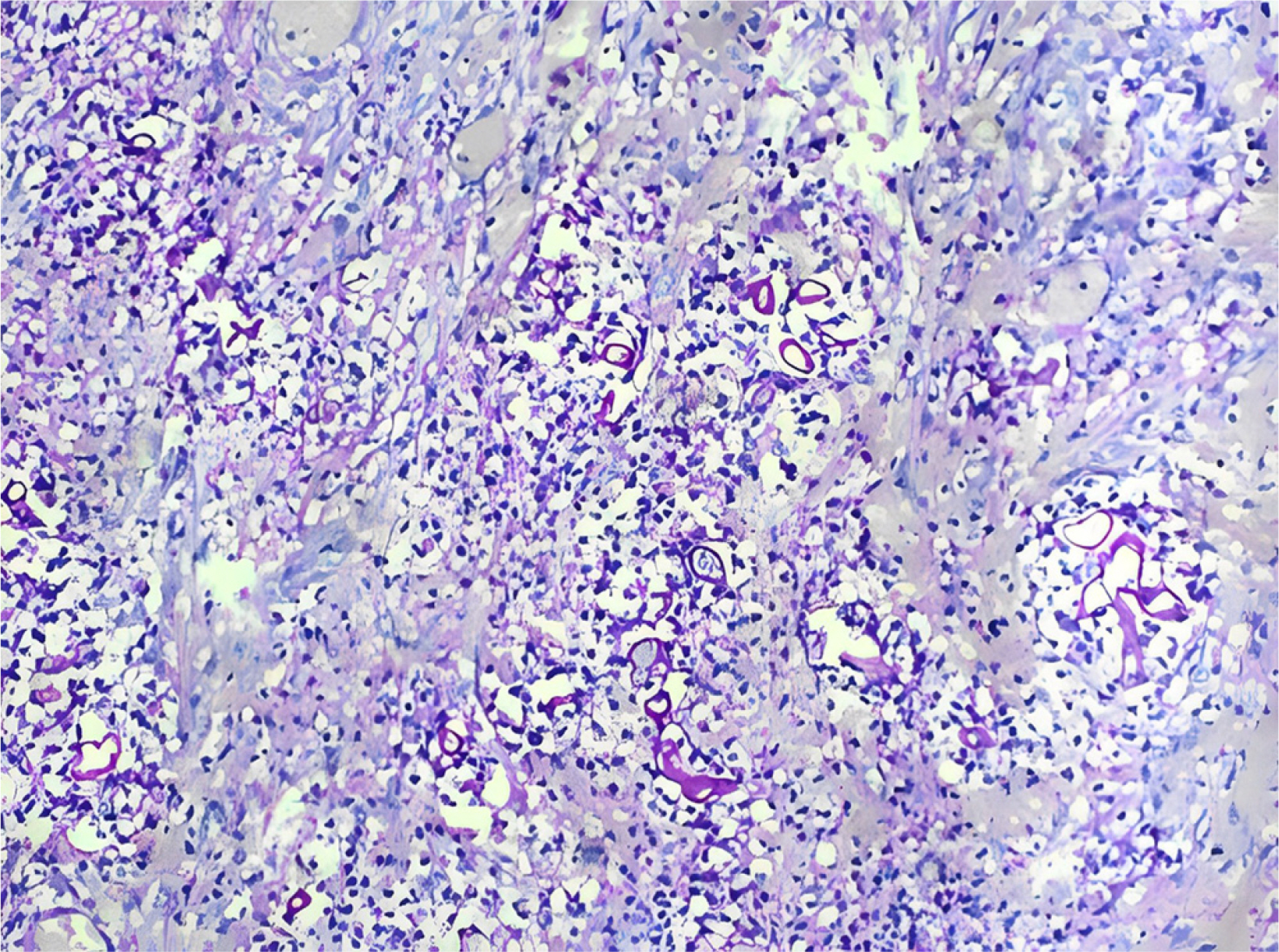
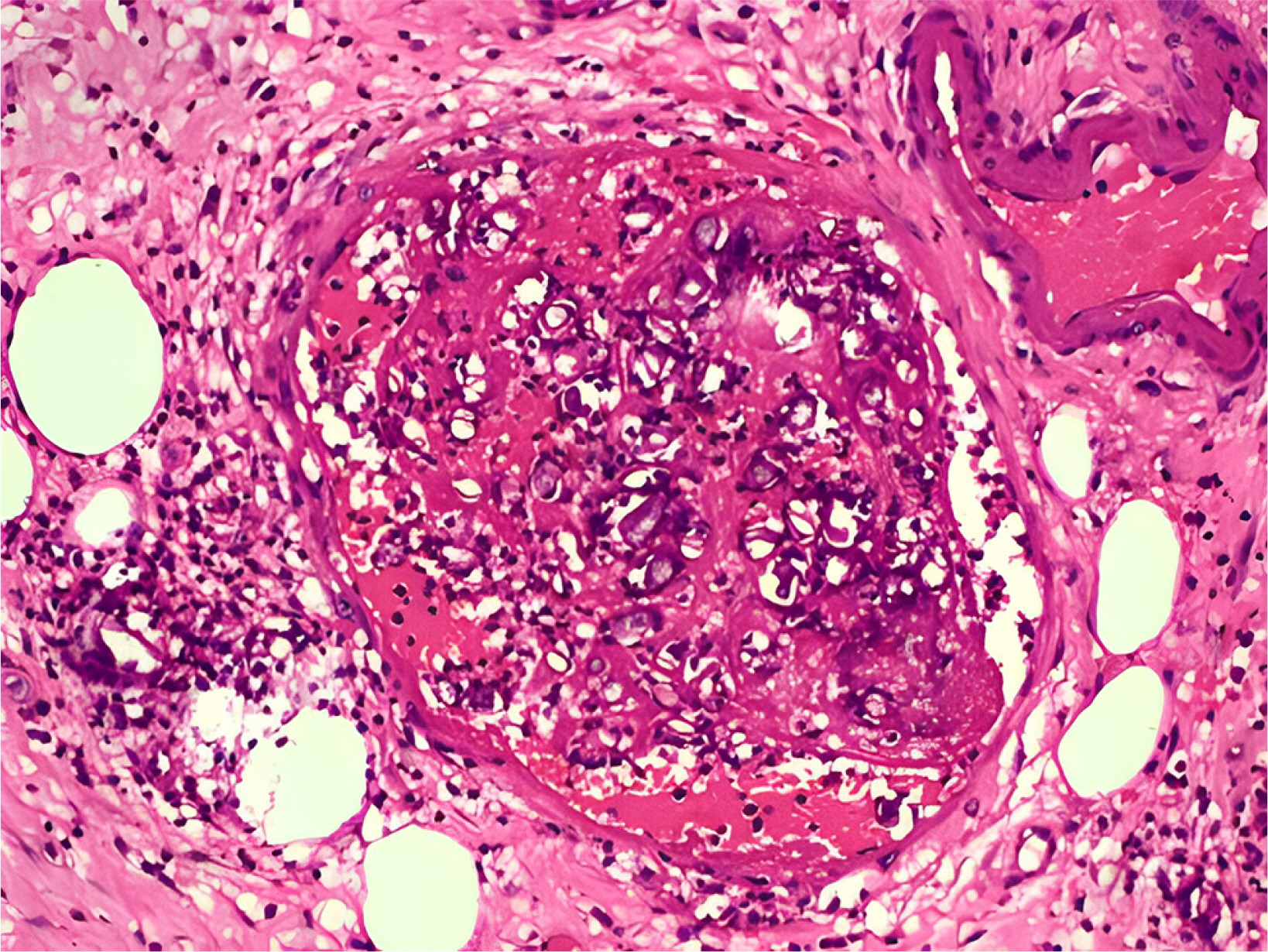
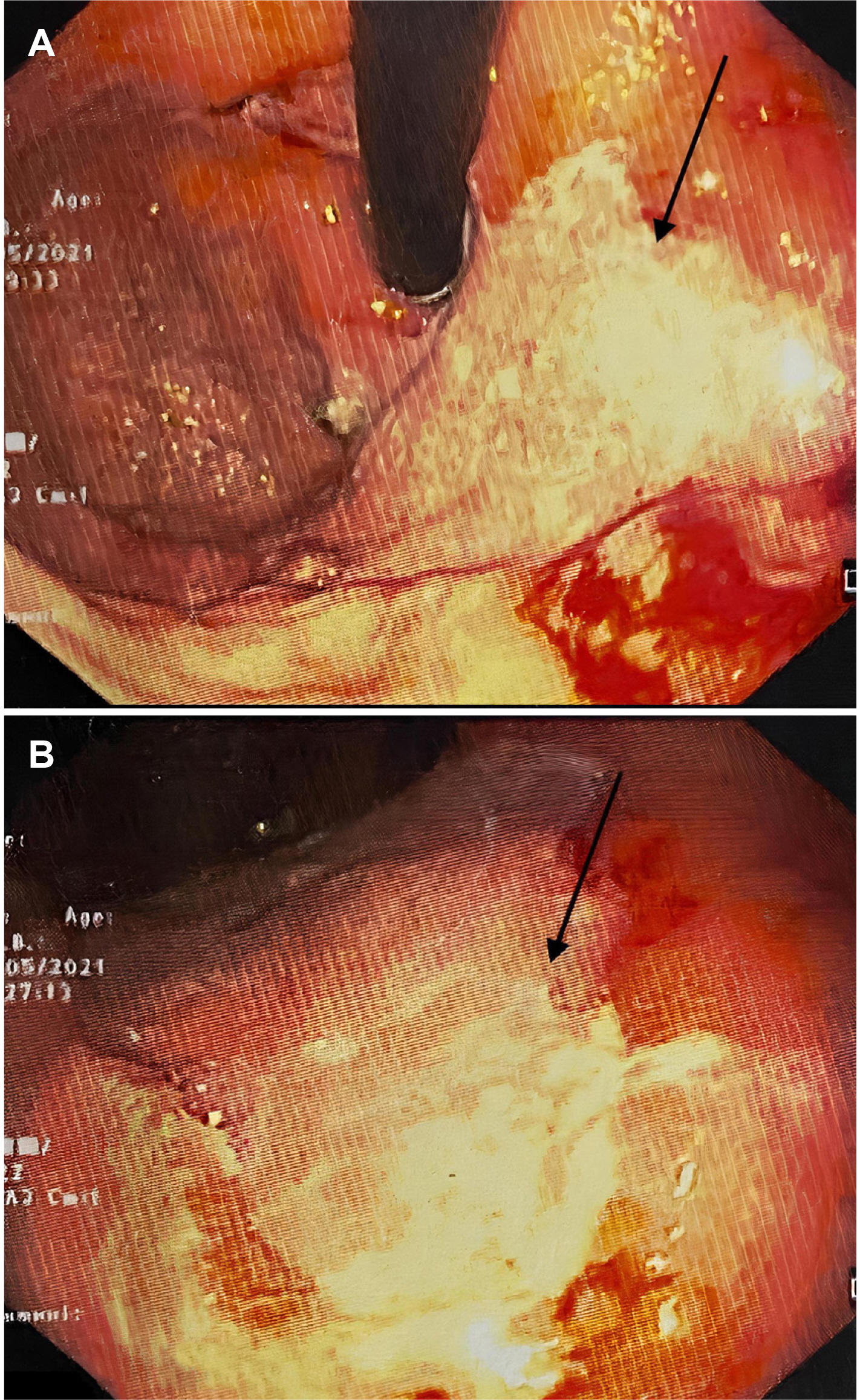
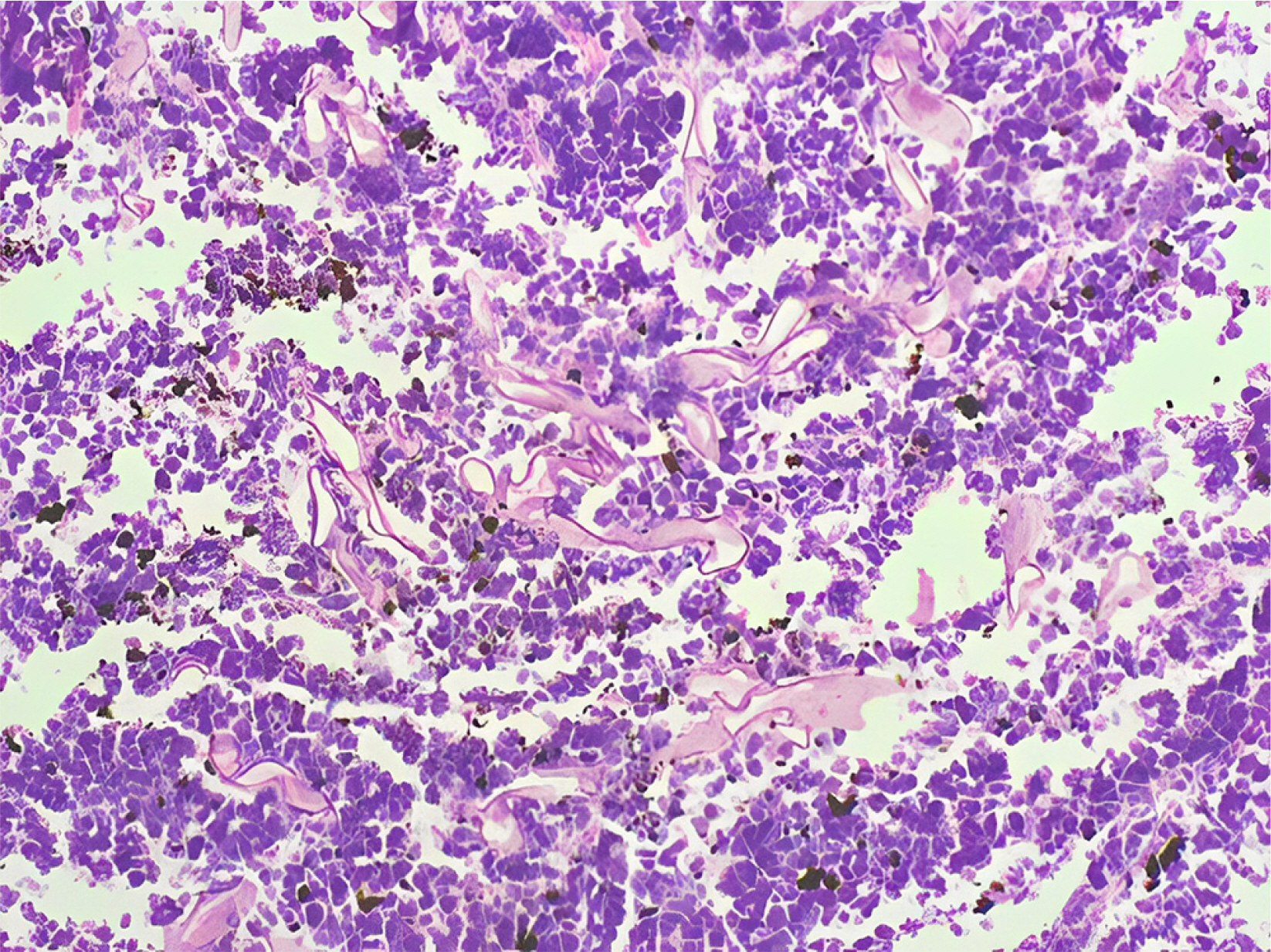
- Gastrointestinal mucormycosis is a rare disease with a significant mortality rate, even when promptly diagnosed and treated. An unusual complication was observed in India during the second wave of coronavirus disease 2019 (COVID-19). Two incidences of gastric mucormycosis were found. A 53-year-old male patient with a history of COVID-19 one month earlier came into the intensive care unit. After admission, the patient developed hematemesis, which was initially treated with blood transfusions and digital subtraction angiography embolization. Esophagogastroduodenoscopy (EGD) revealed a large ulcer with a clot in the stomach. During an exploratory laparotomy, the proximal stomach was necrotic. Histopathological examination confirmed mucormycosis. The patient was started on antifungals, but despite rigorous therapy, the patient died on the tenth postoperative day. Another patient, an 82-year-old male with a history of COVID-19, arrived with hematemesis two weeks earlier and was treated conservatively. EGD revealed a large white-based ulcer with abundant slough along the larger curvature of the body. Mucormycosis was verified by biopsy. He was treated with amphotericin B and isavuconazole. He was discharged after two weeks in a stable condition. Despite quick detection and aggressive treatment, the prognosis is poor. In the second case, prompt diagnosis and treatment saved the patient’s life.
Keyword
Figure
Reference
-
1. Adhikari S, Gautam AR, Paudyal B, Sigdel KR, Basnyat B. 2019; Case Report: Gastric Mucormycosis- a rare but important differential diagnosis of upper gastrointestinal bleeding in an area of Helicobacter pylori endemicity. Wellcome Open Res. 4:5. DOI: 10.12688/wellcomeopenres.15026.1. PMID: 31131332. PMCID: PMC6518441.
Article2. Kauffman CA, Malani AN. 2007; Zygomycosis: an emerging fungal infection with new options for management. Curr Infect Dis Rep. 9:435–440. DOI: 10.1007/s11908-007-0066-4. PMID: 17999877.
Article3. Roden MM, Zaoutis TE, Buchanan WL, et al. 2005; Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 41:634–653. DOI: 10.1086/432579. PMID: 16080086.
Article4. Rothan HA, Byrareddy SN. 2020; The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 109:102433. DOI: 10.1016/j.jaut.2020.102433. PMID: 32113704. PMCID: PMC7127067.
Article5. Riley TT, Muzny CA, Swiatlo E, Legendre DP. 2016; Breaking the mold: A review of mucormycosis and current pharmacological treatment options. Ann Pharmacother. 50:747–757. DOI: 10.1177/1060028016655425. PMID: 27307416.6. Singh RP, Gupta N, Kaur T, Gupta A. 2021; Rare case of gastrointestinal mucormycosis with colonic perforation in an immunocompetent patient with COVID-19. BMJ Case Rep. 14:e244096. DOI: 10.1136/bcr-2021-244096. PMID: 34215642. PMCID: PMC8256735.
Article7. Jain M, Tyagi R, Tyagi R, Jain G. 2022; Post-COVID-19 gastrointestinal invasive mucormycosis. Indian J Surg. 84:545–547. DOI: 10.1007/s12262-021-03007-6. PMID: 34177157. PMCID: PMC8219178.
Article8. Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. 2012; Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis. 54 Suppl 1:S23–34. DOI: 10.1093/cid/cir866. PMID: 22247442.
Article9. Song G, Liang G, Liu W. 2020; Fungal Co-infections associated with Global COVID-19 pandemic: A clinical and diagnostic perspective from China. Mycopathologia. 185:599–606. DOI: 10.1007/s11046-020-00462-9. PMID: 32737747. PMCID: PMC7394275.
Article10. Spellberg B, Walsh TJ, Kontoyiannis DP, Edwards J Jr, Ibrahim AS. 2009; Recent advances in the management of mucormycosis: from bench to bedside. Clin Infect Dis. 48:1743–1751. DOI: 10.1086/599105. PMID: 19435437. PMCID: PMC2809216.
Article11. Werthman-Ehrenreich A. 2021; Mucormycosis with orbital compartment syndrome in a patient with COVID-19. Am J Emerg Med. 42:264.e5–264.e8. DOI: 10.1016/j.ajem.2020.09.032. PMID: 32972795. PMCID: PMC7493738.
Article12. Monte Junior ESD, Santos MELD, Ribeiro IB, et al. 2020; Rare and fatal gastrointestinal mucormycosis (zygomycosis) in a COVID-19 patient: a case report. Clin Endosc. 53:746–749. DOI: 10.5946/ce.2020.180. PMID: 33207116. PMCID: PMC7719411.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COVID-19 and Fungal Infection
- Hemopneumothorax as an Unusual and Delayed Complication of Coronavirus Disease 2019 Pneumonia: A Case Report
- Comprehensive Review of COVID-19 on Benign Prostate Hyperplasia Patient Symptoms
- Assessment and Management of Dysphagia during the COVID-19 Pandemic
- Polyposis of gastrointestinal tract after COVID-19 mRNA vaccination: a report of two cases