J Korean Med Sci.
2023 May;38(20):e147. 10.3346/jkms.2023.38.e147.
Geographic Distribution of Central Nervous System Rehabilitation Treatment in Korea and Its Associated Factors
- Affiliations
-
- 1Graduate School of Public Health, Seoul National University, Seoul, Korea
- 2Outpatient Rehabilitation Center, Korea Workers’ Compensation and Welfare Service Incheon Hospital, Incheon, Korea
- 3Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea
- 4National Traffic Injury Rehabilitation Research Institute, National Traffic Injury Rehabilitation Hospital, Yangpyeong, Korea
- 5Institute of Health Policy and Management, Medical Research Center, Seoul National University, Seoul, Korea
- KMID: 2542590
- DOI: http://doi.org/10.3346/jkms.2023.38.e147
Abstract
- Background
Health disparity is defined as a difference in the accessibility of medical resources among regions or other factors. In South Korea, there might be a disparity because of the low proportion of public medical institutions. This study aimed to investigate the geographic distribution of rehabilitation treatment and examine the factors associated with the rates of rehabilitation treatment in Korea.
Methods
We used administrative claims data in 2007, 2012, and 2017 from the National Health Insurance Database in Korea. We defined physical therapy and occupational therapy as rehabilitation treatments and analyzed the rate of rehabilitation treatments for administrative districts in 2007, 2012, and 2017. Interdecile range and coefficient of variation were used to investigate the geographic distribution of rehabilitation treatment over time. We applied multiple random intercept negative binomial regression to examine the factors associated with rehabilitation treatment. A total of 28,319,614 inpatient and outpatient claims were submitted for 874 hospitals that provided rehabilitation treatment in 2007, 2012, and 2017.
Results
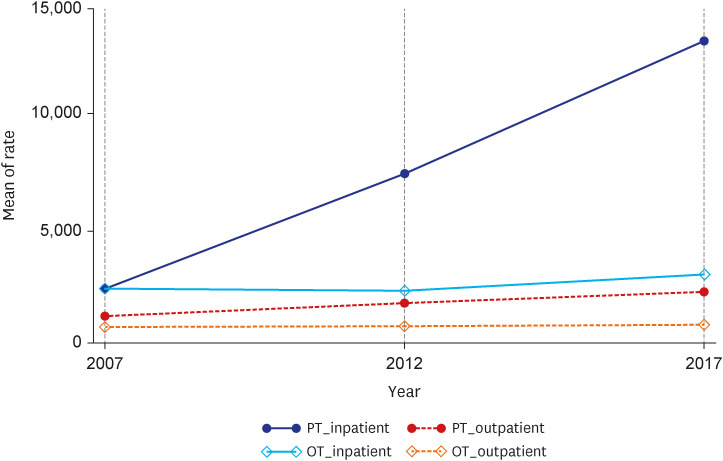
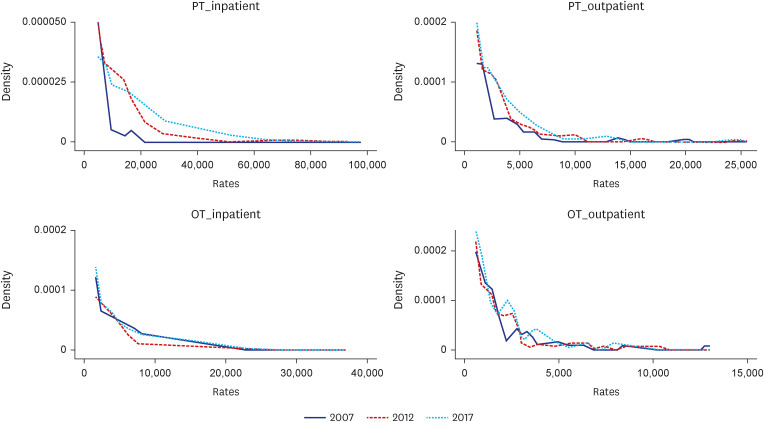
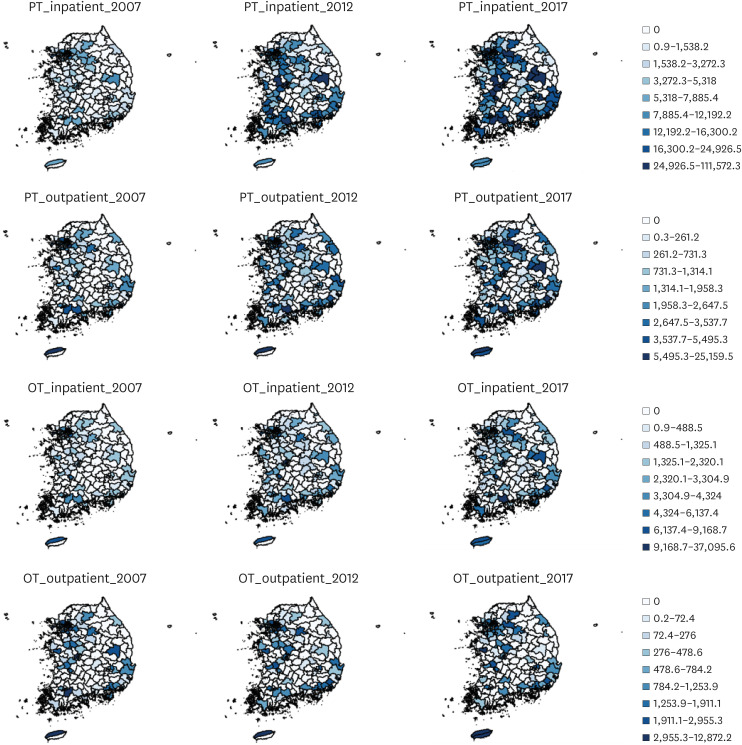
The increase in the mean rates of physical therapy inpatients and outpatients was greater than those for occupational therapy inpatients and outpatients from 2007 to 2017. Both physical therapy and occupational therapy were concentrated in the Seoul Capital Area and other large urban areas. More than 30% of the districts received no rehabilitation treatment. The interdecile range and coefficient of variation for physical therapy declined more than those for occupational therapy from 2007 to 2017. The deprivation index was negatively correlated with physical therapy inpatients, physical therapy outpatients, occupational therapy inpatients, and occupational therapy outpatients. Furthermore, a 1-unit increase in the number of hospital beds per 1,000 people was associated with 1.42 times higher physical therapy inpatient, 1.44 times higher physical therapy outpatient, 2.14 times higher occupational therapy inpatient, and 3.30 times higher occupational therapy outpatient treatment.
Conclusion
To reduce the geographic inequality in rehabilitation treatment, it is necessary to narrow the gap between the supply and demand of rehabilitation services. Providing incentives or direct provisions from the government might be an alternative.
Keyword
Figure
Reference
-
1. Jørgensen HS, Nakayama H, Raaschou HO, Vive-Larsen J, Støier M, Olsen TS. Outcome and time course of recovery in stroke. Part I: outcome. The Copenhagen Stroke Study. Arch Phys Med Rehabil. 1995; 76(5):399–405. PMID: 7741608.2. Pappalardo A, D’Amico E, Leone C, Messina S, Chisari C, Rampello L, et al. Inpatient versus outpatient rehabilitation for multiple sclerosis patients: effects on disability and quality of life. Mult Scler Demyelinating Disord. 2016; 1(1):3.3. Mak MK, Wong-Yu IS, Shen X, Chung CL. Long-term effects of exercise and physical therapy in people with Parkinson disease. Nat Rev Neurol. 2017; 13(11):689–703. PMID: 29027544.4. World Health Organization. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Geneva, Switzerland: World Health Organization;2010.5. Culyer AJ. Equity - some theory and its policy implications. J Med Ethics. 2001; 27(4):275–283. PMID: 11479360.6. Agency for Healthcare Research and Quality (AHRQ). Disparities. Updated 2021. Accessed January 24, 2022. https://www.ahrq.gov/topics/disparities.html .7. Horner RD, Swanson JW, Bosworth HB, Matchar DB. VA Acute Stroke (VAST) Study Team. Effects of race and poverty on the process and outcome of inpatient rehabilitation services among stroke patients. Stroke. 2003; 34(4):1027–1031. PMID: 12624220.8. Gao F, Foster M, Liu Y. Disability concentration and access to rehabilitation services: a pilot spatial assessment applying geographic information system analysis. Disabil Rehabil. 2019; 41(20):2468–2476. PMID: 29726287.9. Jing Q, Tang Q, Sun M, Li X, Chen G, Lu J. Regional disparities of rehabilitation resources for persons with disabilities in China: data from 2014 to 2019. Int J Environ Res Public Health. 2020; 17(19):7319. PMID: 33036409.10. Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009; 374(9696):1196–1208. PMID: 19801098.11. Kim YS, Lee J, Moon Y, Kim KJ, Lee K, Choi J, et al. Unmet healthcare needs of elderly people in Korea. BMC Geriatr. 2018; 18(1):98. PMID: 29678164.12. Kim HK, Leigh JH, Lee YS, Choi Y, Kim Y, Kim JE, et al. Decreasing incidence and mortality in traumatic brain injury in Korea, 2008–2017: a population-based longitudinal study. Int J Environ Res Public Health. 2020; 17(17):6197. PMID: 32859061.13. Jung SH. Stroke rehabilitation fact sheet in Korea. Ann Rehabil Med. 2022; 46(1):1–8. PMID: 35272435.14. Choi Y, Kim YE, Leigh JH, Lee YS, Kim HK, Yi YG, et al. Comparison of trends in the incidence of traumatic spinal cord injury in daily life, automobile accidents, and industrial accidents: a national multi-insurance study in Korea. J Korean Med Sci. 2023; 38(7):e26. PMID: 36808542.15. Kim KW, Kim OS. Super aging in South Korea unstoppable but mitigatable: a sub-national scale population projection for best policy planning. Spat Demogr. 2020; 8(2):155–173. PMID: 34222615.16. Bai G, Anderson GF. A more detailed understanding of factors associated with hospital profitability. Health Aff (Millwood). 2016; 35(5):889–897. PMID: 27140996.17. Kim AM, Kang S, Park JH, Yoon TH, Kim Y. A spatial analysis of geographic variation and factors associated with hospitalization for bacterial pneumonia in Korea. BMC Pulm Med. 2019; 19(1):45. PMID: 30786908.18. Kim AM, Park JH, Yoon TH, Kim Y. Hospitalizations for ambulatory care sensitive conditions as an indicator of access to primary care and excess of bed supply. BMC Health Serv Res. 2019; 19(1):259. PMID: 31029134.19. Kim AM, Park JH, Kang S, Hwang K, Lee T, Kim Y. The effect of geographic units of analysis on measuring geographic variation in medical services utilization. J Prev Med Public Health. 2016; 49(4):230–239. PMID: 27499165.20. Kim AM, Park JH, Kang S, Yoon TH, Kim Y. An ecological study of geographic variation and factors associated with cesarean section rates in South Korea. BMC Pregnancy Childbirth. 2019; 19(1):162. PMID: 31072318.21. Townsend P. Deprivation. J Soc Policy. 1987; 16(2):125–146.22. Korea S. Resident registration population status. Update 2022. Accessed March 15, 2022. https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B040A3&checkFlag=N .23. Ministry of Health and Welfare. Disability registration status. Updated 2018. Accessed March 15, 2022. http://www.mohw.go.kr/react/jb/sjb030301ls.jsp?PAR_MENU_ID=03&MENU_ID=0321 .24. Salgado-Ugarte IH, Shimizu M, Taniuchi T. Exploring the shape of univariate data using kernel density estimators. Stata Tech Bull. 1994; 3(16):25. StataCorp. LP. Stata Multilevel Mixed-Effects Reference Manual Release 17. College Station, TX, USA: StataCorp LP;2021.26. Moon HE. A study on small area variations of the rehabilitation service utilization in post-stroke patients [master’s thesis]. Seoul, Korea: Seoul National University;2013.27. Leigh JH, Kim WS, Sohn DG, Chang WK, Paik NJ. Transitional and long-term rehabilitation care system after stroke in Korea. Front Neurol. 2022; 13:786648. PMID: 35432175.28. Costa AP, Poss JW, Peirce T, Hirdes JP. Acute care inpatients with long-term delayed-discharge: evidence from a Canadian health region. BMC Health Serv Res. 2012; 12(1):172. PMID: 22726609.29. Sonoda S, Saitoh E, Nagai S, Kawakita M, Kanada Y. Full-time integrated treatment program, a new system for stroke rehabilitation in Japan: comparison with conventional rehabilitation. Am J Phys Med Rehabil. 2004; 83(2):88–93. PMID: 14758294.30. Kinoshita S, Abo M, Okamoto T, Miyamura K. Transitional and long-term care system in Japan and current challenges for stroke patient rehabilitation. Front Neurol. 2022; 12:711470. PMID: 35087461.31. Sun EY, Jadotte YT, Halperin W. Disparities in cardiac rehabilitation participation in the United States: a systematic review and meta-analysis. J Cardiopulm Rehabil Prev. 2017; 37(1):2–10. PMID: 27676464.32. Sharifi A, Kamali M, Chabok A. Rehabilitation needs of people with cerebral palsy: a qualitative study. Med J Islam Repub Iran. 2014; 28:16. PMID: 25250261.33. Phillips KA, Morrison KR, Andersen R, Aday LA. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998; 33(3 Pt 1):571–596. PMID: 9685123.34. Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s Behavioral Model of health services use: a systematic review of studies from 1998-2011. Psychosoc Med. 2012; 9:Doc11. PMID: 23133505.35. Bachmann JM, Huang S, Gupta DK, Lipworth L, Mumma MT, Blot WJ, et al. Association of neighborhood socioeconomic context with participation in cardiac rehabilitation. J Am Heart Assoc. 2017; 6(10):e006260. PMID: 29021267.36. Yong-Jae L. An study on the inequality of health care resources distribution affected by regional characteristics. J Crit Soc Welf. 2005; 21:49–78.37. Kamenov K, Mills JA, Chatterji S, Cieza A. Needs and unmet needs for rehabilitation services: a scoping review. Disabil Rehabil. 2019; 41(10):1227–1237. PMID: 29303004.38. Bright T, Wallace S, Kuper H. A systematic review of access to rehabilitation for people with disabilities in low- and middle-income countries. Int J Environ Res Public Health. 2018; 15(10):2165. PMID: 30279358.39. Ministry of Health and Welfare. Ministry of Health and Welfare Statistics YearBook 2017. Sejong, Korea: 2018.40. Ministry of Health and Welfare. Ministry of Health and Welfare Statistics YearBook 2013. Seoul, Korea: 2013.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rehabilitation treatment system for the convalescent and maintenance periods
- Characteristics of Swallowing Disorder in Pediatric Patients with Central Nervous System Disorders: Comparing to Central Nervous System Intact Patients with Gastro-intestinal Disorders
- The value of computerized axial tomography of the brain in children with central nervous system disorders
- Treatment of pediatric central nervous system infections
- A Study on CSF Enzyme Activity in Central Nervous System Infections