Ann Surg Treat Res.
2023 May;104(5):274-280. 10.4174/astr.2023.104.5.274.
Impact of the COVID-19 pandemic on the outcomes of laparoscopic appendectomy for acute appendicitis
- Affiliations
-
- 1Department of Surgery, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea
- 2Department of Surgery, Hallym University Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea
- KMID: 2542234
- DOI: http://doi.org/10.4174/astr.2023.104.5.274
Abstract
- Purpose
This retrospective study aimed to evaluate the impact of the coronavirus disease 2019 (COVID-19) pandemic on the time interval from symptom onset to surgery and on the operative outcomes of laparoscopic appendectomy for patients with acute appendicitis.
Methods
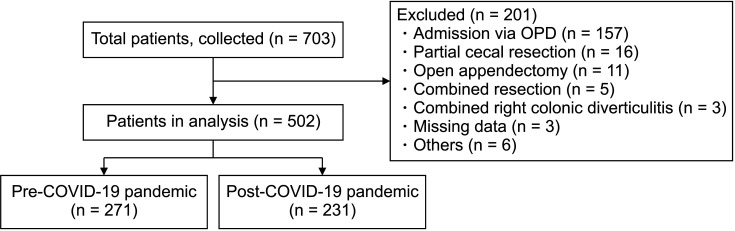
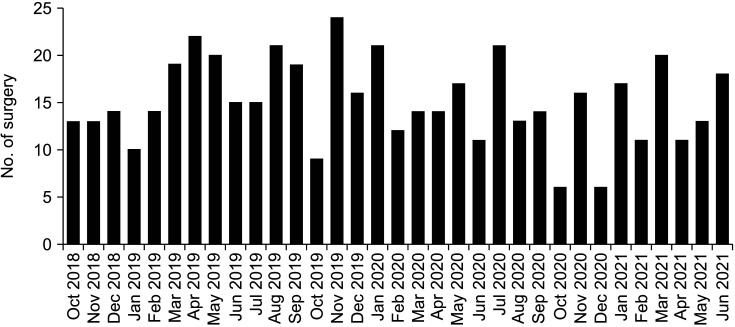
Between October 2018 and July 2021, laparoscopic appendectomy was performed in 502 patients with acute appendicitis admitted to Hallym University Chuncheon Sacred Heart Hospital in Chuncheon, Korea. We compared demographic data, serum levels of inflammatory markers, time to event of appendicitis, and operative outcomes between the pre-COVID-19 and post-COVID-19 pandemic groups.
Results
Laparoscopic appendectomy was performed in 271 patients in the pre-COVID-19 group and in 231 patients in the post-COVID-19 group. There were no differences in baseline characteristics, serum inflammatory marker levels, or the proportions of complicated appendicitis between the groups (25.1%, pre-COVID-19 vs. 31.6%, post-COVID-19; P = 0.106). The time intervals between symptom onset and hospital arrival (24.42 hours vs. 23.59 hours, P = 0.743) and between hospital arrival and the start of surgery (10.12 hours vs. 9.04 hours, P = 0.246) did not increase post-COVID-19. The overall 30-day postoperative complication rate did not differ significantly between the groups (9.6% vs. 10.8%, P = 0.650), and the severity of 30-day postoperative complications was also similar in both groups (P = 0.447).
Conclusion
This study demonstrates that hospitalization and surgeries were not delayed in patients with acute appendicitis and that the operative outcomes of laparoscopic appendectomy did not worsen despite the COVID-19 pandemic.
Keyword
Figure
Reference
-
1. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708–1720. PMID: 32109013.2. Baum A, Schwartz MD. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020; 324:96–99. PMID: 32501493.3. Reschen ME, Bowen J, Novak A, Giles M, Singh S, Lasserson D, et al. Impact of the COVID-19 pandemic on emergency department attendances and acute medical admissions. BMC Emerg Med. 2021; 21:143. PMID: 34800973.4. Gao Z, Li M, Zhou H, Liang Y, Zheng C, Li S, et al. Complicated appendicitis are common during the epidemic period of 2019 novel coronavirus (2019-nCoV). Asian J Surg. 2020; 43:1002–1005. PMID: 32863144.5. Köhler F, Müller S, Hendricks A, Kastner C, Reese L, Boerner K, et al. Changes in appendicitis treatment during the COVID-19 pandemic: a systematic review and meta-analysis. Int J Surg. 2021; 95:106148. PMID: 34700020.6. Rudnicki Y, Soback H, Mekiten O, Lifshiz G, Avital S. The impact of COVID-19 pandemic lockdown on the incidence and outcome of complicated appendicitis. Surg Endosc. 2022; 36:3460–3466. PMID: 34312724.7. Scheijmans JC, Borgstein AB, Puylaert CA, Bom WJ, Bachiri S, van Bodegraven EA, et al. Impact of the COVID-19 pandemic on incidence and severity of acute appendicitis: a comparison between 2019 and 2020. BMC Emerg Med. 2021; 21:61. PMID: 33980150.8. Turanli S, Kiziltan G. Did the COVID-19 pandemic cause a delay in the diagnosis of acute appendicitis? World J Surg. 2021; 45:18–22. PMID: 33089347.9. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.10. Pokala N, Sadhasivam S, Kiran RP, Parithivel V. Complicated appendicitis: is the laparoscopic approach appropriate?: a comparative study with the open approach: outcome in a community hospital setting. Am Surg. 2007; 73:737–742. PMID: 17879676.11. Ceresoli M, Coccolini F, Magnone S, Lucianetti A, Bisagni P, Armao T, et al. The decrease of non-complicated acute appendicitis and the negative appendectomy rate during pandemic. Eur J Trauma Emerg Surg. 2021; 47:1359–1365. PMID: 33844036.12. Huijgen D, de Wijkerslooth EM, Janssen JC, Beverdam FH, Boerma EG, Dekker JW, et al. Multicenter cohort study on the presentation and treatment of acute appendicitis during the COVID-19 pandemic. Int J Colorectal Dis. 2022; 37:1087–1095. PMID: 35415811.13. Zaikos TD, Boudiab EM, Peshel EC, Wu AA, Dyer E, Haut ER, et al. Acute appendicitis severity during the early COVID-19 pandemic period. Trauma Surg Acute Care Open. 2021; 6:e000809. PMID: 34466662.14. El Nakeeb A, Emile SH, AbdelMawla A, Attia M, Alzahrani M, ElGamdi A, et al. Presentation and outcomes of acute appendicitis during COVID-19 pandemic: lessons learned from the Middle East: a multicentre prospective cohort study. Int J Colorectal Dis. 2022; 37:777–789. PMID: 35152340.15. Orthopoulos G, Santone E, Izzo F, Tirabassi M, Pérez-Caraballo AM, Corriveau N, et al. Increasing incidence of complicated appendicitis during COVID-19 pandemic. Am J Surg. 2021; 221:1056–1060. PMID: 33012500.16. Zheng Z, Bi JT, Liu YQ, Cai X. The impact of COVID-19 pandemic on the treatment of acute appendicitis in China. Int J Colorectal Dis. 2022; 37:215–219. PMID: 34647160.17. Choi HG, Kang HS, Lim H, Kim JH, Kim JH, Cho SJ, et al. Changes in the incidence rates of gastrointestinal diseases due to the COVID-19 pandemic in south korea: a long-term perspective. J Pers Med. 2022; 12:1144. PMID: 35887641.18. An S, Kim HR, Jang S, Kim K. The impact of the coronavirus disease-19 pandemic on the clinical characteristics and treatment of adult patients with acute appendicitis. Front Surg. 2022; 9:878534. PMID: 35433818.19. Angeramo CA, Dreifuss NH, Schlottmann F, Rotholtz NA. More severe presentations of acute appendicitis during COVID-19. J Gastrointest Surg. 2021; 25:1902–1904. PMID: 33469887.20. Gaitero Tristán J, Souto Romero H, Escalada Pellitero S, Espiñera CR, Andina Martín D, Espinosa Góngora R, et al. Acute appendicitis in children during the COVID-19 pandemic: neither delayed diagnosis nor worse outcomes. Pediatr Emerg Care. 2021; 37:185–190. PMID: 33651763.21. Velayos M, Muñoz-Serrano AJ, Estefanía-Fernández K, Sarmiento Caldas MC, Moratilla Lapeña L, López-Santamaría M, et al. Influence of the coronavirus 2 (SARS-Cov-2) pandemic on acute appendicitis. An Pediatr (Engl Ed). 2020; 93:118–122.22. Kariya A, Krutsri C, Singhatas P, Sumritpradit P, Thampongsa T, Lertsitthichai P, et al. Incidence of complicated appendicitis during the COVID-19 pandemic: a systematic review and meta-analysis. Int J Surg Open. 2022; 45:100512. PMID: 35845315.23. Choi YS, Yi JW, Chung CT, Shin WY, Choi SK, Heo YS. Clinical experience of emergency appendectomy under the COVID-19 pandemic in a single institution in South Korea. Medicina (Kaunas). 2022; 58:783. PMID: 35744046.24. Kang BM, Choi SI, Kim BS, Lee SH. Single-port laparoscopic surgery in uncomplicated acute appendicitis: a randomized controlled trial. Surg Endosc. 2018; 32:3131–3137. PMID: 29340826.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of COVID-19 on the care of acute appendicitis: a single-center experience in Korea
- Safety of laparoscopic appendectomy for the management of acute appendicitis during pregnancy
- Did the COVID-19 pandemic impact the surgical treatment of febrile acute appendicitis at a single center in Korea, a country not under lockdown? Observational cohort study
- Laparoscopic Appendectomy for Acute Appendicitis Caused by Enterobius Vermicularis
- Clinical Evaluation of Laparoscopic Appendectomy