J Yeungnam Med Sci.
2023 Apr;40(2):187-192. 10.12701/jyms.2022.00759.
Outcomes after repair of complete atrioventricular canal with a modified single-patch technique: a retrospective study
- Affiliations
-
- 1Department of Adult Cardiac Surgery, Onassis Cardiac Surgery Center, Athens, Greece
- 2Department of Paediatric and Congenital Heart Surgery, Onassis Cardiac Surgery Center, Athens, Greece
- 3Department of Thoracic Surgery, Attikon University Hospital of Athens, Athens, Greece
- 4Paediatric Cardiac and Adult Congenital Heart Disease Intensive Care Unit, Onassis Cardiac Surgery Center, Athens, Greece
- 5Department of Cardiac Surgery Intensive Care, Onassis Cardiac Surgery Center, Athens, Greece
- 6Department of Paediatric Cardiology and Adult Congenital Heart Disease, Onassis Cardiac Surgery Center, Athens, Greece
- KMID: 2541945
- DOI: http://doi.org/10.12701/jyms.2022.00759
Abstract
- Background
This study aimed to present the short- and midterm outcomes after complete atrioventricular canal defect (CAVC) repair using a single-patch technique.
Methods
This study included 30 children who underwent surgical correction of the CAVC using a single-patch technique.
Results
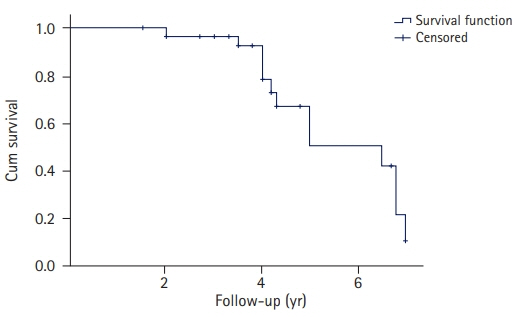
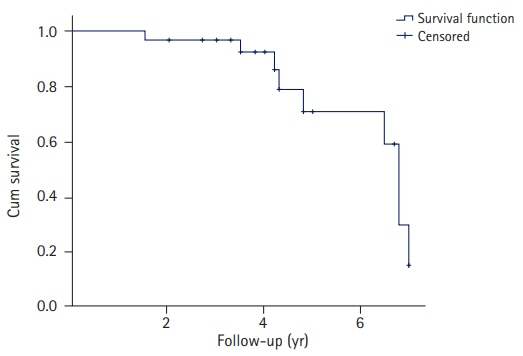
The median age of the patients was 5.7 months (interquartile range [IQR], 5.0–7.5 months), and 23 patients (76.7%) had type A CAVC. Fourteen patients (46.7%) were female and 17 (56.7%) had been diagnosed with Down syndrome. The in-hospital mortality rate was 0%. No deaths were observed during a median follow-up of 4 years (IQR, 3.5–5.0 years). Patients without Down syndrome were associated with late moderate mitral regurgitation (MR) (p=0.02). Late MR less than moderate degree was observed in 96.6%, 78.5%, and 50% of patients after 2, 4, and 5 years of follow-up, respectively, while late tricuspid valve regurgitation less than moderate degree was observed in 96.7%, 85.9%, and 59.0% of patients after 2, 4, and 6 years of follow-up, respectively. After a median follow-up of 4 years, only one patient had required surgical repair of a left ventricular outflow tract obstruction, which occurred 26 months after the first operation. Multivariable logistic regression analysis adjusted for the type of CAVC, sex, Down syndrome, age, and weight revealed that the absence of Down syndrome was a risk factor for late moderate MR (MR-2) (odds ratio, 0.05; 95% confidence interval, 0.006–0.50; p=0.01).
Conclusion
A single-patch technique for CAVC surgical repair is a safe method with acceptable short- and midterm results.
Figure
Reference
-
References
1. Pacifico AD. Atrio-ventricular septal defects. In : Stark JF, de Leval MR, Tsang VT, editors. Surgery for congenital heart defects. 3rd ed. Chichester, UK; Hoboken, NJ: John Wiley & Sons;2006.2. Rastelli G, Kirklin JW, Titus JL. Anatomic observations on complete form of persistent common atrioventricular canal with special reference to atrioventricular valves. Mayo Clin Proc. 1966; 41:296–308.3. Wilcox BR, Jones DR, Frantz EG, Brink LW, Henry GW, Mill MR, et al. Anatomically sound, simplified approach to repair of "complete" atrioventricular septal defect. Ann Thorac Surg. 1997; 64:487–94.4. Nicholson IA, Nunn GR, Sholler GF, Hawker RE, Cooper SG, Lau KC, et al. Simplified single patch technique for the repair of atrioventricular septal defect. J Thorac Cardiovasc Surg. 1999; 118:642–6.5. Reynen S, Hövels-Gürich HH, Vazquez-Jimenez JF, Messmer BJ, Sachweh JS. Long-term outcome up to 40 years after single patch repair of complete atrioventricular septal defect in infancy or childhood. Thorac Cardiovasc Surg. 2021; 69(Suppl 3):e68–75.6. Stephens EH, Backer CL. Teaching the modified single-patch technique for complete atrioventricular septal defect. World J Pediatr Congenit Heart Surg. 2022; 13:371–5.7. Cantinotti M, Giordano R, Koestenberger M, Voges I, Santoro G, Franchi E, et al. Echocardiographic examination of mitral valve abnormalities in the paediatric population: current practices. Cardiol Young. 2020; 30:1–11.8. Geoffrion TR, Singappuli K, Murala JSK. A review of the Nunn modified single patch technique for atrioventricular septal defect repair. Transl Pediatr. 2018; 7:91–103.9. Azzab S, Samy A, Singab H, Zeinah M, Musollari G, Axiaq A, et al. The effect of surgical technique, age, and trisomy 21 on early outcome of surgical management of complete atrioventricular canal defect. Cardiol Young. 2022; 32:869–73.10. Ginde S, Lam J, Hill GD, Cohen S, Woods RK, Mitchell ME, et al. Long-term outcomes after surgical repair of complete atrioventricular septal defect. J Thorac Cardiovasc Surg. 2015; 150:369–74.11. Houck CA, Evertz R, Teuwen CP, Roos-Hesselink JW, Kammeraad JA, Duijnhouwer AL, et al. Dysrhythmias in patients with a complete atrioventricular septal defect: from surgery to early adulthood. Congenit Heart Dis. 2019; 14:280–7.12. Backer CL, Kaushal S, Mavroudis C. Modified single-patch technique: repairing complete atrioventricular septal defect. Ann Pediatr Cardiol. 2009; 2:51–4.13. Di Mambro C, Calvieri C, Silvetti MS, Tamburri I, Giannico S, Baban A, et al. Bradyarrhythmias in repaired atrioventricular septal defects: single-center experience based on 34 years of follow-up of 522 patients. Pediatr Cardiol. 2018; 39:1590–7.14. Backer CL, Eltayeb O, Mongé MC, Wurlitzer KC, Hack MA, Boles LH, et al. Modified single patch: are we still worried about subaortic stenosis? Ann Thorac Surg. 2015; 99:1671–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Repair of Complete Atrioventricular Septal Defect with Surgical Modification
- Surgical Treatment of Complete Atrioventricular Septal Defect with Tetralogy of Fallot: Report of one case
- Clinical Outcomes of Diverse Patch Grafts
- Surgical Treatment of Complete Atrioventricular Septal Defect: The Early and Mid-Term Results
- A New Technique of Arthroscopic Meniscal Repair -Modified Inside-Out Technique