Intest Res.
2023 Apr;21(2):196-204. 10.5217/ir.2022.00045.
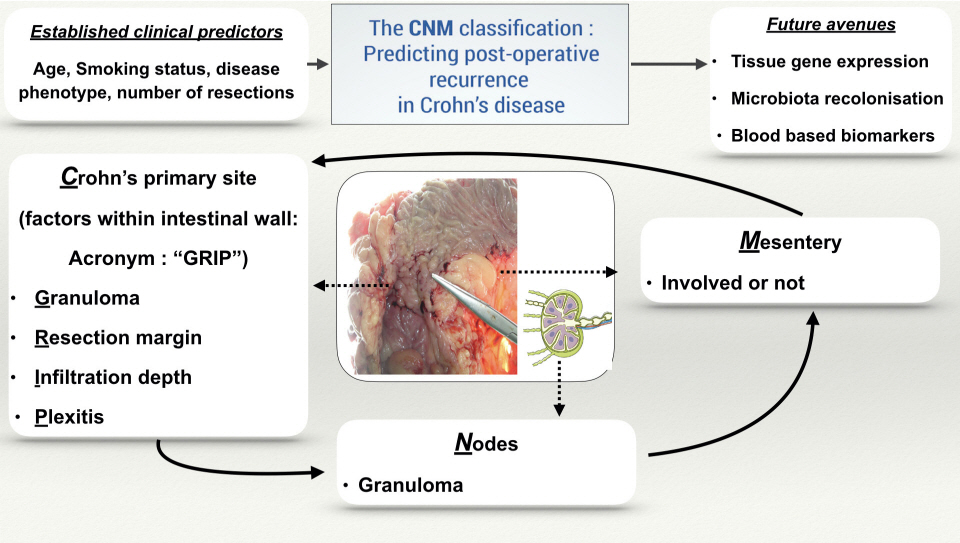
Proposal of novel staging system CNM (Crohn’s primary site, nodes, mesentery) to predict postoperative recurrence of Crohn’s disease
- Affiliations
-
- 1Department of Surgical Gastroenterology, Asian Institute of Gastroenterology, Hyderabad, India
- 2Department of Medical Gastroenterology, Asian Institute of Gastroenterology, Hyderabad, India
- 3Department of Pathology, Asian Institute of Gastroenterology, Hyderabad, India
- KMID: 2541892
- DOI: http://doi.org/10.5217/ir.2022.00045
Abstract
- After oncologic resection, histological grading and staging of the tumor give important prognostic information about the future risk of recurrence and hence influence the subsequent management plan. Several studies and their meta-analysis have shown that various histological features (e.g., microscopic positive resection margins, plexitis, granuloma, mesenteric inflammatory activity) can predict postoperative clinical/endoscopic/surgical recurrence after resection in Crohn’s disease (CD). Inclusion of mesentery in surgical resection specimens has been shown to reduce surgical recurrence after ileocolonic resection in CD. However, there is no uniform histopathological staging system for risk stratification in postoperative CD to systematically predict postoperative recurrence. This is because the prediction to date is based on clinical characteristics (smoking status, disease phenotype, surgical history). Histopathological predictors are still not adopted in routine clinical practice due to the lack of a uniform staging system, heterogeneity of published studies and lack of standardized definition of histological features. In this article, we attempted to incorporate all such histological features in a single histological staging system CNM (Crohn’s primary site [resection margin positivity, plexitis, granuloma, depth of infiltration], nodes [presence of granuloma], mesentery [involved or not]) in surgical resection specimen in CD. The proposed CNM classification would help to enable systematic reporting, design future clinical trials, stratify postoperative recurrence risk and choose appropriate postoperative prophylaxis.
Keyword
Figure
Reference
-
1. Tandon P, Malhi G, Abdali D, et al. Active margins, plexitis, and granulomas increase postoperative Crohn’s recurrence: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2021; 19:451–462.
Article2. Coffey CJ, Kiernan MG, Sahebally SM, et al. Inclusion of the mesentery in ileocolic resection for Crohn’s disease is associated with reduced surgical recurrence. J Crohns Colitis. 2018; 12:1139–1150.
Article3. de Groof EJ, van der Meer JH, Tanis PJ, et al. Persistent mesorectal inflammatory activity is associated with complications after proctectomy in Crohn’s disease. J Crohns Colitis. 2019; 13:285–293.
Article4. Li Y, Mohan H, Lan N, et al. Mesenteric excision surgery or conservative limited resection in Crohn’s disease: study protocol for an international, multicenter, randomized controlled trial. Trials. 2020; 21:210.
Article5. Fazio VW, Marchetti F, Church M, et al. Effect of resection margins on the recurrence of Crohn’s disease in the small bowel: a randomized controlled trial. Ann Surg. 1996; 224:563–573.
Article6. Bemelman WA, Warusavitarne J, Sampietro GM, et al. ECCOESCP consensus on surgery for Crohn’s disease. J Crohns Colitis. 2018; 12:1–16.
Article7. Riault C, Diouf M, Chatelain D, et al. P692 Positive histological margins is a risk factor of recurrence after ileocaecal resection in Crohn’s disease. J Crohns Colitis. 2019; 13(Suppl 1):S466–S467.
Article8. de Buck van Overstraeten A, Eshuis EJ, Vermeire S, et al. Short- and medium-term outcomes following primary ileocaecal resection for Crohn’s disease in two specialist centres. Br J Surg. 2017; 104:1713–1722.
Article9. Kinchen J, Rajaratnam K, Kingston G, Mee A, De Silva A. P211 The presence of microscopic disease at the resection margins predicts post-surgical relapse in Crohn’s disease. J Crohns Colitis. 2012; 6(Suppl 1):S93–S94.
Article10. Malireddy K, Larson DW, Sandborn WJ, et al. Recurrence and impact of postoperative prophylaxis in laparoscopically treated primary ileocolic Crohn disease. Arch Surg. 2010; 145:42–47.
Article11. Wasmann KA, van Amesfoort J, van Montfoort ML, Koens L, Bemelman WA, Buskens CJ. The predictive value of inflammation at ileocecal resection margins for postoperative Crohn’s recurrence: a cohort study. Inflamm Bowel Dis. 2020; 26:1691–1699.
Article12. Ferrante M, de Hertogh G, Hlavaty T, et al. The value of myenteric plexitis to predict early postoperative Crohn’s disease recurrence. Gastroenterology. 2006; 130:1595–1606.
Article13. Ng SC, Lied GA, Kamm MA, Sandhu F, Guenther T, Arebi N. Predictive value and clinical significance of myenteric plexitis in Crohn’s disease. Inflamm Bowel Dis. 2009; 15:1499–1507.
Article14. Boland K, Stempak J, Weizman A, et al. P311 Microscopic inflammation and myenteric plexitis at the margin of resection do not predict endoscopic recurrence in patients with Crohn’s disease after ileocolic resection. J Crohns Colitis. 2017; 11(Suppl 1):S235.
Article15. Hammoudi N, Cazals-Hatem D, Auzolle C, et al. Association between microscopic lesions at ileal resection margin and recurrence after surgery in patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2020; 18:141–149.16. Misteli H, Koh CE, Wang LM, Mortensen NJ, George B, Guy R. Myenteric plexitis at the proximal resection margin is a predictive marker for surgical recurrence of ileocaecal Crohn’s disease. Colo-rectal Dis. 2015; 17:304–310.
Article17. Nakao S, Itabashi M, Yamamoto T, Okamoto T. Predictive value of myenteric and submucosal plexitis for postoperative Crohn’s disease recurrence. J Anus Rectum Colon. 2018; 1:56–64.
Article18. Sokol H, Polin V, Lavergne-Slove A, et al. Plexitis as a predictive factor of early postoperative clinical recurrence in Crohn’s disease. Gut. 2009; 58:1218–1225.
Article19. Milassin Á, Sejben A, Tiszlavicz L, et al. Analysis of risk factors-especially different types of plexitis-for postoperative relapse in Crohn’s disease. World J Gastrointest Surg. 2017; 9:167–173.
Article20. Bressenot A, Peyrin-Biroulet L. Histologic features predicting postoperative Crohn’s disease recurrence. Inflamm Bowel Dis. 2015; 21:468–475.
Article21. Decousus S, Boucher AL, Joubert J, et al. Myenteric plexitis is a risk factor for endoscopic and clinical postoperative recurrence after ileocolonic resection in Crohn’s disease. Dig Liver Dis. 2016; 48:753–758.
Article22. Lemmens B, de Buck van Overstraeten A, Arijs I, et al. Submucosal plexitis as a predictive factor for postoperative endoscopic recurrence in patients with Crohn’s disease undergoing a resection with ileocolonic anastomosis: results from a prospective single-centre study. J Crohns Colitis. 2017; 11:212–220.
Article23. Blaker PA, Nedjat-Shokouhi B, Thomas DM, Harris AW. P074 - Myenteric plexitis does not predict endoscopic Crohn’s disease recurrence 12 months following ileo-colonic resection in district general hospital practice. J Crohns Colitis. 2009; 3:S40.
Article24. Rahier JF, Dubuquoy L, Colombel JF, et al. Decreased lymphatic vessel density is associated with postoperative endoscopic recurrence in Crohn’s disease. Inflamm Bowel Dis. 2013; 19:2084–2090.
Article25. Cullen G, O’toole A, Keegan D, Sheahan K, Hyland JM, O’donoghue DP. Long-term clinical results of ileocecal resection for Crohn’s disease. Inflamm Bowel Dis. 2007; 13:1369–1373.
Article26. Li Y, Stocchi L, Liu X, et al. Presence of granulomas in mesenteric lymph nodes is associated with postoperative recurrence in Crohn’s disease. Inflamm Bowel Dis. 2015; 21:2613–2618.
Article27. Unger LW, Argeny S, Stift A, et al. Mesenteric granulomas independently predict long-term risk of surgical recurrence in Crohn’s disease. Colorectal Dis. 2020; 22:170–177.
Article28. Poredska K, Kunovsky L, Marek F, et al. The influence of microscopic inflammation at resection margins on early postoperative endoscopic recurrence after ileocaecal resection for Crohn’s disease. J Crohns Colitis. 2020; 14:361–368.
Article29. Denoya P, Canedo J, Berho M, et al. Granulomas in Crohn’s disease: does progression through the bowel layers affect presentation or predict recurrence? Colorectal Dis. 2011; 13:1142–1147.
Article30. Heimann TM, Miller F, Martinelli G, Szporn A, Greenstein AJ, Aufses AH Jr. Correlation of presence of granulomas with clinical and immunologic variables in Crohn’s disease. Arch Surg. 1988; 123:46–48.
Article31. Gionchetti P, Dignass A, Danese S, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: Part 2: surgical management and special situations. J Crohns Colitis. 2017; 11:135–149.
Article32. Sensi B, Siragusa L, Efrati C, et al. The role of inflammation in Crohn’s disease recurrence after surgical treatment. J Immunol Res. 2020; 2020:8846982.
Article33. Coffey JC, Byrnes KG, Walsh DJ, Cunningham RM. Update on the mesentery: structure, function, and role in disease. Lancet Gastroenterol Hepatol. 2022; 7:96–106.
Article34. Zhu Y, Qian W, Huang L, et al. Role of extended mesenteric excision in postoperative recurrence of Crohn’s colitis: a single-center study. Clin Transl Gastroenterol. 2021; 12:e00407.
Article35. Ble A, Renzulli C, Cenci F, et al. The relationship between endoscopic and clinical recurrence in postoperative Crohn’s disease: a systematic review and meta-analysis. J Crohns Colitis. 2022; 16:490–499.
Article36. Bachour SP, Shah RS, Lyu R, et al. Test characteristics of cross-sectional imaging and concordance with endoscopy in postoperative Crohn’s disease. Clin Gastroenterol Hepatol. 2022; 20:2327–2336.
Article37. Fahad H, Abu-Elmagd K, Lashner B, Fiocchi C. Recurrence of Crohn’s disease after small bowel transplantation: fact or fiction. Inflamm Bowel Dis. 2020; 26:21–23.
Article38. Hamilton AL, Kamm MA, De Cruz P, et al. Luminal microbiota related to Crohn’s disease recurrence after surgery. Gut Microbes. 2020; 11:1713–1728.
Article39. Cerrillo E, Moret I, Iborra M, et al. A nomogram combining fecal calprotectin levels and plasma cytokine profiles for individual prediction of postoperative Crohn’s disease recurrence. Inflamm Bowel Dis. 2019; 25:1681–1691.
Article40. Machiels K, Pozuelo Del Río M, Martinez-De la Torre A, et al. Early postoperative endoscopic recurrence in Crohn’s disease is characterised by distinct microbiota recolonisation. J Crohns Colitis. 2020; 14:1535–1546.
Article41. Ngollo M, Perez K, Hammoudi N, et al. Identification of gene expression profiles associated with an increased risk of postoperative recurrence in Crohn’s disease. J Crohns Colitis. 2022; 16:1269–1280.42. Walshe M, Nayeri S, Ji J, et al. A role for CXCR3 ligands as biomarkers of post-operative Crohn’s disease recurrence. J Crohns Colitis. 2022; 16:900–910.
Article43. McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm. 2016; 38:655–662.
Article44. Waggoner J, Carline JD, Durning SJ. Is there a consensus on consensus methodology? Descriptions and recommendations for future consensus research. Acad Med. 2016; 91:663–668.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary hypertrophic osteoarthropathy accompanied by Crohn's disease: a case report
- Isolated Crohn's Disease of Appendix: Is It Crohn's Disease or Idiopathic Granulomatous Appendicitis? Report of a case and review of the literature
- Prevention of Post-operative Recurrence in Crohn's Disease
- New Aspects of surgical therapy of recurrent Crohn's disease
- A case of Crohn disease