Ann Rehabil Med.
2023 Apr;47(2):118-128. 10.5535/arm.22103.
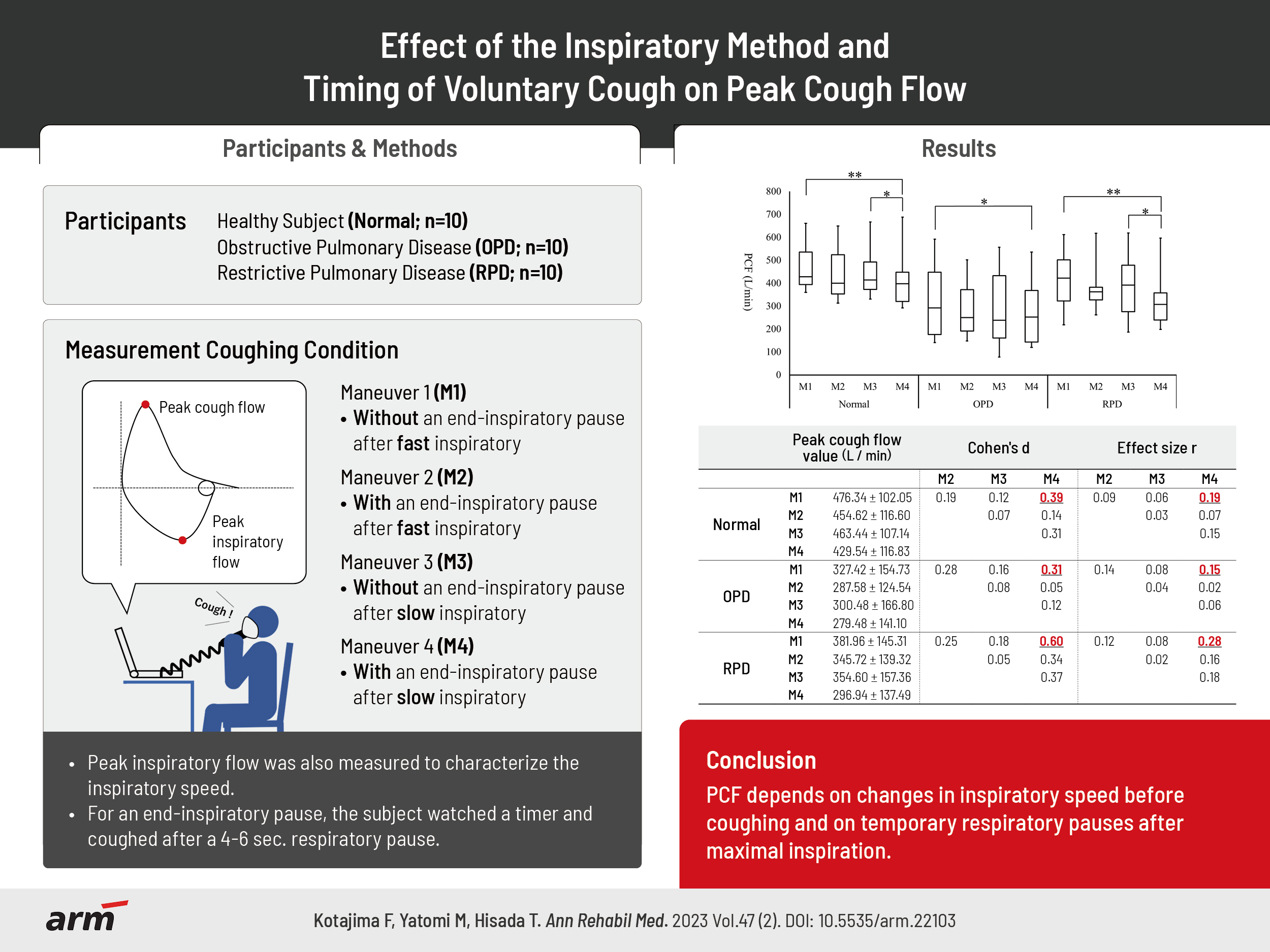
Effect of the Inspiratory Method and Timing of Voluntary Cough on Peak Cough Flow
- Affiliations
-
- 1Department of Rehabilitation Sciences, Gunma University Graduate School of Health Sciences, Maebashi, Japan
- 2Department of Respiratory Medicine, Gunma University Graduate School of Medicine, Maebashi, Japan
- 3Department of Allergy and Respiratory Medicine, Gunma University Hospital, Maebashi, Japan
- KMID: 2541845
- DOI: http://doi.org/10.5535/arm.22103
Abstract
Objective
To define the effect of the inspiratory method and cough timing on peak cough flow (PCF).
Methods
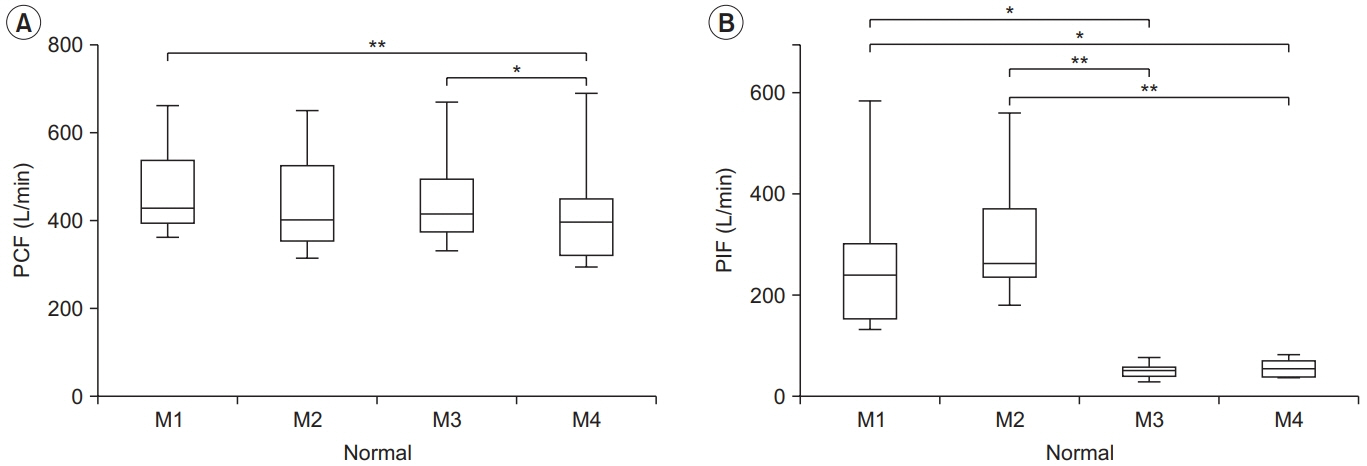
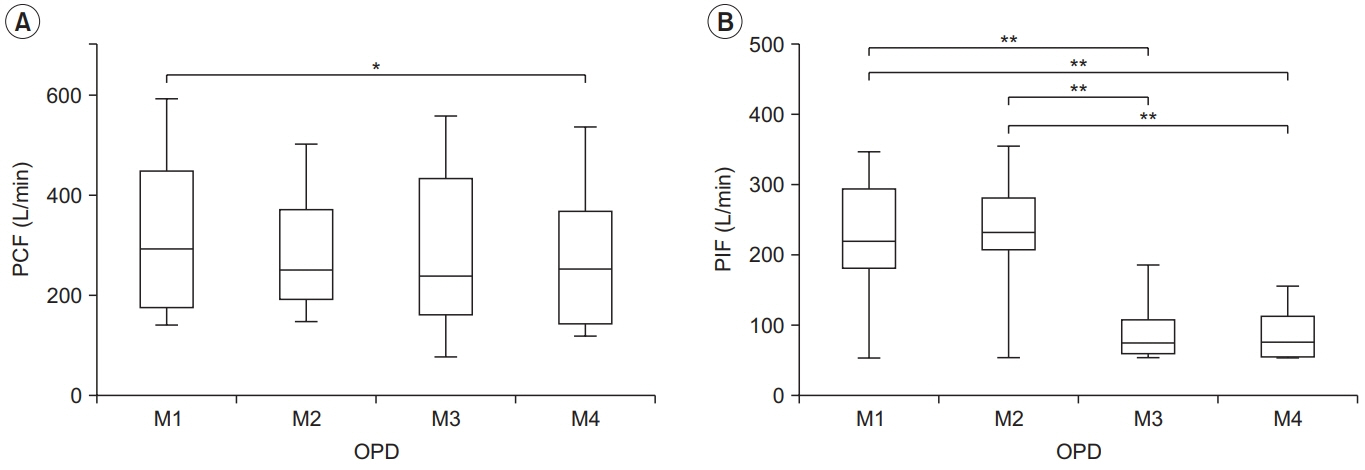
We investigated the effect of measurement conditions on PCF in healthy subjects (n=10). We then compared obstructive and restrictive pulmonary diseases (n=20) to assess for similar results in respiratory diseases. The PCF was measured under four conditions: before coughing, without maneuver 1 or with maneuver 2 a temporary respiratory pause (4–6 seconds) after rapid inspiration, and without maneuver 3 or with maneuver 4 a temporary respiratory pause after slow inspiration. After the measurements were completed, the PCF between the four conditions was compared for each subject group, and the effect size was calculated.
Results
PCF of maneuvers 1 and 3 were significantly higher than maneuver 4 in healthy subjects (476.34±102.05 L/min and 463.44±107.14 L/min vs. 429.54±116.83 L/min, p<0.01 and p<0.05, respectively) and patients with restrictive pulmonary disease (381.96±145.31 L/min, 354.60±157.36 L/min vs. 296.94±137.49 L/min, p<0.01 and p<0.05, respectively). In obstructive pulmonary disease, maneuver 1 was significantly higher than maneuver 4 (327.42±154.73 L/min vs. 279.48±141.10 L/min, p<0.05). The largest effect sizes were shown by maneuvers 4 and 1.
Conclusion
PCF depends on changes in inspiratory speed before coughing and on temporary respiratory pauses after maximal inspiration. It will become necessary to unify the measurement methods for coughing strength and present appropriate coughing methods.
Keyword
Figure
Reference
-
1. Bach JR, Saporito LR. Criteria for extubation and tracheostomy tube removal for patients with ventilatory failure. A different approach to weaning. Chest. 1996; 110:1566–71.
Article2. Bach JR, Ishikawa Y, Kim H. Prevention of pulmonary morbidity for patients with Duchenne muscular dystrophy. Chest. 1997; 112:1024–8.
Article3. Chatwin M, Toussaint M, Gonçalves MR, Sheers N, Mellies U, Gonzales-Bermejo J, et al. Airway clearance techniques in neuromuscular disorders: a state of the art review. Respir Med. 2018; 136:98–110.
Article4. Finder JD, Birnkrant D, Carl J, Farber HJ, Gozal D, Iannaccone ST, et al. Respiratory care of the patient with Duchenne muscular dystrophy: ATS consensus statement. Am J Respir Crit Care Med. 2004; 170:456–65.5. Bach JR. Update and perspectives on noninvasive respiratory muscle aids. Part 1: the inspiratory aids. Chest. 1994; 105:1230–40.
Article6. Bianchi C, Baiardi P, Khirani S, Cantarella G. Cough peak flow as a predictor of pulmonary morbidity in patients with dysphagia. Am J Phys Med Rehabil. 2012; 91:783–8.
Article7. Hanayama K, Ishikawa Y, Bach JR. Amyotrophic lateral sclerosis. Successful treatment of mucous plugging by mechanical insufflation-exsufflation. Am J Phys Med Rehabil. 1997; 76:338–9.8. D’Angelo E, Prandi E, Milic-Emili J. Dependence of maximal flow-volume curves on time course of preceding inspiration. J Appl Physiol (1985). 1993; 75:1155–9.
Article9. D’Angelo E, Prandi E, Marazzini L, Milic-Emili J. Dependence of maximal flow-volume curves on time course of preceding inspiration in patients with chronic obstruction pulmonary disease. Am J Respir Crit Care Med. 1994; 150(6 Pt 1):1581–6.
Article10. Koulouris NG, Rapakoulias P, Rassidakis A, Dimitroulis J, Gaga M, Milic-Emili J, et al. Dependence of forced vital capacity manoeuvre on time course of preceding inspiration in patients with restrictive lung disease. Eur Respir J. 1997; 10:2366–70.
Article11. Kurazumi Y, Horikoshi T, Tsuchikawa T, Matsubara N. The body surface area of Japanese. Jpn J Biometeorol. 1994; 31:5–29.12. Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of spirometry 2019 update. An Official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med. 2019; 200:e70–88.
Article13. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2021 report). Global Initiative for Chronic Obstructive Lung Disease, Inc.;2021.14. Yawata A, Tsubaki A, Yawata H, Takai H, Matsumoto K, Takehara N, et al. Voluntary cough intensity and its influencing factors differ by sex in community-dwelling adults. Ther Adv Respir Dis. 2017; 11:427–33.
Article15. Trebbia G, Lacombe M, Fermanian C, Falaize L, Lejaille M, Louis A, et al. Cough determinants in patients with neuromuscular disease. Respir Physiol Neurobiol. 2005; 146:291–300.
Article16. Tzelepis GE, Zakynthinos S, Vassilakopoulos T, Geroulanos S, Roussos C. Inspiratory maneuver effects on peak expiratory flow. Role of lung elastic recoil and expiratory pressure. Am J Respir Crit Care Med. 1997; 156:1399–404.
Article17. D’Angelo E, Milic-Emili J, Marazzini L. Effects of bronchomotor tone and gas density on time dependence of forced expiratory vital capacity maneuver. Am J Respir Crit Care Med. 1996; 154:1318–22.
Article18. West JB, Luks AM. West’s respiratory physiology: the essentials. 10th ed. Philadelphia: Wolters Kluwer;2016. p. 117–45.19. Dietz V, Schmidtbleicher D, Noth J. Neuronal mechanisms of human locomotion. J Neurophysiol. 1979; 42:1212–22.
Article20. Komi PV. Stretch-shortening cycle: a powerful model to study normal and fatigued muscle. J Biomech. 2000; 33:1197–206.
Article21. Zakynthinos S, Vassilakopoulos T, Mavrommatis A, Roussos C, Tzelepis GE. Effects of different expiratory maneuvers on inspiratory muscle force output. Am J Respir Crit Care Med. 1999; 159:892–5.
Article22. Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging. 2006; 1:253–60.
Article23. Gibson GJ. Clinical tests of respiratory function. 2nd ed. London: Chapman and Hall;1996. p. 57–160.24. Hughes JMB, Pride NB. Lung function tests: physiological principles and clinical applications. Philadelphia: Saunders;1999. p. 27–9.25. Boni E, Chiari S, Trigiani M, Gatta D, Pini L, Tantucci C. Effect of preceding inspiratory speed and endinspiratory pause on forced expiratory manoeuvre in healthy subjects and chronic obstructive pulmonary disease patients. Respiration. 2009; 78:270–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Respiratory Muscle Strength and Cough Capacity in Patients with Duchenne Muscular Dystrophy
- Assisted Cough and Pulmonary Compliance in Patients with Duchenne Muscular Dystrophy
- Analysis of Pulmonary Mechanics and the Factors for Coughing in Duchenne Muscular Dystrophy
- Clinical Significance of Nasal Peak Inspiratory Flow Rate in Patients with Chronic Cough
- The Relationships of Coughing to the Respiratory Muscle Strength and Pulmonary Compliance in Tetraplegic Patients