J Korean Acad Oral Health.
2023 Mar;47(1):26-31. 10.11149/jkaoh.2023.47.1.26.
A machine learning based decision tree analysis of influential factor for the number of remaining teeth in Korean adults
- Affiliations
-
- 1Department of Dental Hygiene, Daejeon Institute of Science and Technology, Daejeon, Korea
- 2Department of Dental Hygiene, College of Health Science, Dankook University, Cheonan, Korea
- KMID: 2541088
- DOI: http://doi.org/10.11149/jkaoh.2023.47.1.26
Abstract
Objectives
This study aims to investigate the effect of determinants on the number of remaining teeth in Korean adults using a machine learning-based decision tree analysis.
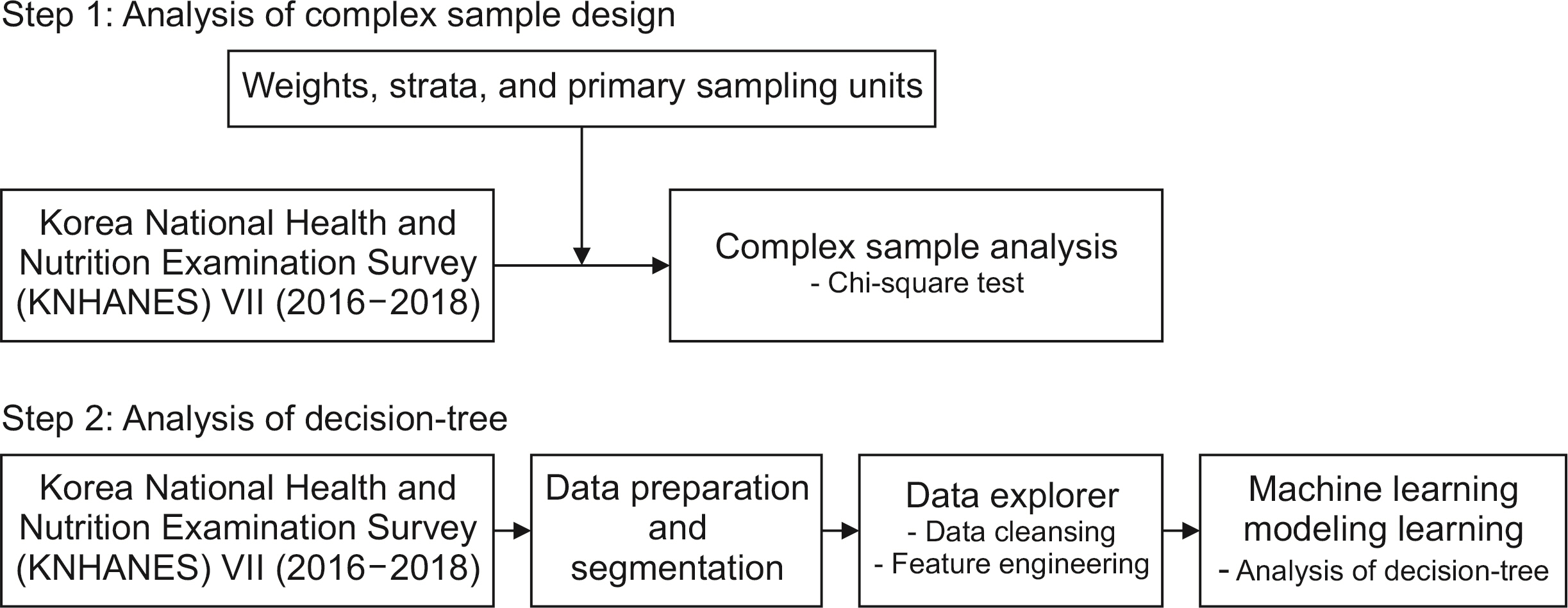
Methods
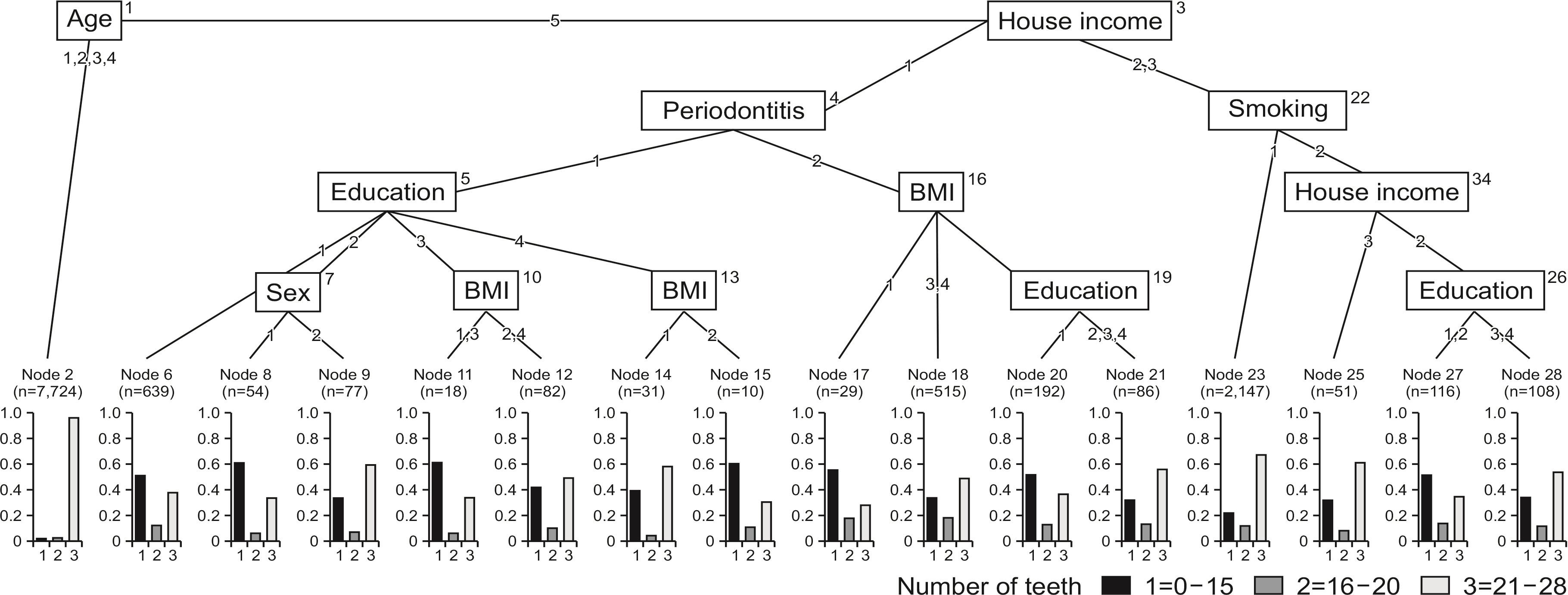
The study used data from the Korea National Health and Nutrition Examination Survey (KNHANES) VII (2016-2018) and a decision-tree analysis to explain the causes for the number of remaining teeth in adults. The determinants for the study are sex, age, house income, education level, diabetes, BMI, smoking, alcohol drinking, tooth brushing per day, and periodontitis.
Results
Age had the most significant effect on the number of remaining teeth, followed by house income.
Conclusions
This research is meaningful as it provides a systematic index in the number of remaining teeth in Korean adults based on a combination of numerous variables. These variables have already been validated against the results of previous studies that have attempted to elucidate new variables affecting the number of remaining teeth.
Keyword
Figure
Reference
-
References
1. Castrejón-Pérez RC, Borges-Yáñez SA, Gutiérrez-Robledo LM, Ávila-Funes JA. 2012; Oral health conditions and frailty in Mexican community-dwelling elderly: a cross sectional analysis. BMC Public Health. 12:773. https://doi.org/10.1186/1471-2458-12-773. DOI: 10.1186/1471-2458-12-773. PMID: 22971075. PMCID: PMC3490998. PMID: 0a8becb6688149a3934a7650929e8a13.
Article2. Lee GR, Yoo WK. 2010; A study on denture satisfaction in rural elderly people. J Agric Med Community Health. 35:56–66. https://doi.org/10.5393/JAMCH.2010.35.1.056. DOI: 10.5393/JAMCH.2010.35.1.056.
Article3. Petersen PE, Kandelman D, Arpin S, Ogawa H. 2010; Global oral health of older people-call for public health action. Community Dent Health. 27:257–267. PMID: 21313969.4. Petersen PE, Yamamoto T. 2005; Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 33:81–92. https://doi.org/10.1111/j.1600-0528.2004.00219.x. DOI: 10.1111/j.1600-0528.2004.00219.x. PMID: 15725170.
Article5. Kim YH, Han K, Vu D, Cho KH, Lee SH. 2018; Number of remaining teeth and its association with socioeconomic status in South Korean adults: data from the Korean national health and nutrition examination survey 2012-2013. PLoS One. 13:e0196594. https://doi.org/10.1371/journal.pone.0196594. DOI: 10.1371/journal.pone.0196594. PMID: 29746489. PMCID: PMC5945020. PMID: a5b8970ece3945dfbbdc33657bafbc6e.
Article6. Jung SH, Ryu JI, Jung DB. 2011; Association of total tooth loss with socio-behavioural health indicators in Korean elderly. J Oral Rehabil. 38:517–524. https://doi.org/10.1111/j.1365-2842.2010.02178.x. DOI: 10.1111/j.1365-2842.2010.02178.x. PMID: 21118289.
Article7. Kim HN, Ha TG, Kim MJ, Jun EJ, Jeong SH, Kim JB. 2016; Factors related to number of present teeth in Korean elderly adults aged 55-84 years. Int J Dent Hyg. 14:151–158. https://doi.org/10.1111/idh.12151. DOI: 10.1111/idh.12151. PMID: 26074207.
Article8. Avlund K, Schultz-Larsen K, Christiansen N, Holm-Pedersen P. 2011; Number of teeth and fatigue in older adults. J Am Geriatr Soc. 59:1459–1464. 03502.x. DOI: 10.1111/j.1532-5415.2011.03502.x. PMID: 21797832.
Article9. Goodman AH, Pelto GH, Allen LH, Chavez A. 1992; Socioeconomic and Anthropometric Correlates of Linear Enamel Hypoplasia Children from Solis, Mexic. Int J Paleopathol. 2:373–380.10. Jimenez M, Dietrich T, Shih MC, Li Y, Joshipura KJ. 2009; Racial/ethnic variations in associations between socioeconomic factors and tooth loss. Community Dent Oral Epidemiol. 37:267–275. https://doi.org/10.1111/j.1600-0528.2009.00466.x. DOI: 10.1111/j.1600-0528.2009.00466.x. PMID: 19302573. PMCID: PMC2758161.
Article11. Aida J, Ando Y, Akhter R, Aoyama H, Masui M, Morita M. 2006; Reasons for permanent tooth extractions in Japan. J Epidemiol. 16:214–219. https://doi.org/10.2188/jea.16.214. DOI: 10.2188/jea.16.214. PMID: 16951541. PMCID: PMC7683702.
Article12. Lee CH, Lee SK, Chang KY. 2002; The profile of age for the tooth extraction in permanent teeth of Koreans. J Korean Acad Dent Health. 26:209–218.13. Lim KJ, Han KY. 1990; A study on the rate of each tooth Loss due to periodontal disease during surgical periodontal treatment. J Periodontal Implant Sci. 20:413–426.14. Han MH. 2022; Identification of high-risk group for obesity in the elderly: Decision tree analysis. Journal of the Korean Data and Information Science Society. 33:629–643. DOI: 10.7465/jkdi.2022.33.4.629.
Article15. Kim HS, Jeong SH, Park SK. 2019; Decision-Tree Analysis to Predict Blood Pressure Control Status Among Hypertension Patients Taking Antihypertensive Medications. J Korean Biol Nurs Sci. 21:85–97. DOI: 10.7586/jkbns.2019.21.1.85.
Article16. Lee KJ, Lee HY, Oh KJ. 2015; Using fuzzy-neural network to predict hedge fund survival. J Korean Data and Information Science Society. 26:1189–1198. https://doi.org/10.7465/jkdi.2015.26.6.1189. DOI: 10.7465/jkdi.2015.26.6.1189.
Article17. Yoo SH, Park IS, Kim YM. 2018; A decision-tree analysis of influential factors and reasons for unmet dental care in Korean adults. Health and Social Welfare Review. 37:294–335. https://doi.org/10.15709/hswr.2017.37.4.294. DOI: 10.15709/hswr.2017.37.4.294.
Article18. World Health Organization(WHO). 2006 Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. [Internet]. Available from: https://apps.who.int/iris/handle/10665/43588?search-result=true&query=Definition+and+diagnosis+of+diabetes+mellitus&scope=&rpp=10&sort_by=score&order=desc. Cited 2023 March 13.19. Park SW, Kim BG, Kim JW, Park JW, Kim JI. 2018; A cross-sectional study on the pulmonary function of residents in two urban areas with different PM 10 concentrations: Data from the fourth Korea national health and nutrition examination survey (KNHANES) 2007-2009. Ann Occup Environ Med. 30:1–12. https://doi.org/10.1186/s40557-018-0258-4. DOI: 10.1186/s40557-018-0258-4. PMID: 30026954. PMCID: PMC6048902. PMID: 79ff9ae22b6b4d648bfc1bc7718d2de6.
Article20. Kim SO, Bae EM, Lee YN, Son JS. 2021; Association between consumption of sugar-sweetened beverages and risk of cardiovascular disease in Korean men: Analysis Based on the Korea National Health and Nutrition Examination Survey 2014-2016. Korean J Fam Med. 42:212–218. https://doi.org/10.4082/kjfm.20.0114. DOI: 10.4082/kjfm.20.0114. PMID: 34038989. PMCID: PMC8164932.
Article21. World Health Organization(WHO). Oral health surveys: basic methods. 4th ed. [Internet]. Available from: https://apps.who.int/iris/handle/10665/41905. Cited 2023 March 13.22. Park HE, Song HY, Han K, Cho KH, Kim YH. 2019; Number of remaining teeth and health-related quality of life: The Korean National Health and Nutrition Examination Survey 2010-2012. Health Qual Life Outcomes. 17:1–10. https://doi.org/10.1186/s12955-019-1078-0. DOI: 10.1186/s12955-019-1078-0. PMID: 30626402. PMCID: PMC6327472. PMID: 977974d998a04977a5cc89f7af8d5a0f.
Article23. Lee JH, Kim GY, Choi KH. 2020; The Relationship between Childbirth, Housing and Socio-Economic Factors: The Pattern Analysis using Decision Tree. Digital Contents Society. 21:327–336. https://doi.org/10.9728/dcs.2020.21.2.327. DOI: 10.9728/dcs.2020.21.2.327.
Article24. Jin HJ. 2010; Analysis for consumer groups using decision tree model: focused on tangerine consumption. The Korean Journal of Agricultural Economics. 50:19–40.25. Hancock S, Zinn C, Schofield G. 2020; The consumption of processed sugar- and starch-containing foods, and dental caries: a systematic review. Eur J Oral Sci. 128:467–475. https://doi.org/10.1111/eos.12743. DOI: 10.1111/eos.12743. PMID: 33156952.
Article26. Nazir MA. 2017; Prevalence of periodontal disease, its association with systemic diseases and prevention. Int J Health Sci. 11:72–80.27. Lee BJ. 2021; Prediction Model of Hypertension Using Sociodemographic Characteristics Based on Machine Learning. KIPS Trans Softw and Data Eng. 10:541–546. https://doi.org/10.3745/KTSD2E.2021.10.11.541.
Article28. Greene JC, Suomi JD. 1977; Epidemiology and public health aspects of caries and periodontal disease. J Dent Res. 56(3_suppl):20–26. https://doi.org/10.1177/002203457705600312011. DOI: 10.1177/002203457705600312011. PMID: 416057.
Article29. Papapanou PN, Lindhe J, Sterrett JD, Eneroth L. 1991; Considerations on the contribution of ageing to loss of periodontal tissue support. J Clin Periodontol. 18:611–615. https://doi.org/10.1111/j.1600-051x.1991.tb00098.x. DOI: 10.1111/j.1600-051X.1991.tb00098.x. PMID: 1795058.
Article30. Lopez B, Pardinas AF, Garcia-Vazquez E, Dopico E. 2012; Socio-cultural factors in dental diseases in the Medieval and early Modern Age of northern Spain. Homo. 63:21–42. https://doi.org/10.1016/j.jchb.2011.12.001. DOI: 10.1016/j.jchb.2011.12.001. PMID: 22265008.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prediction of dental caries in 12-year-old children using machine-learning algorithms
- Evaluating Pedicle-Screw Instrumentation Using Decision-Tree Analysis Based on Pullout Strength
- A pilot study using machine learning methods about factors influencing prognosis of dental implants
- Decision support system for the prognostication of sarcopenia in adult women: Machine learning analysis using Korean National Health and Nutrition Examination Survey data
- Development of Machine Learning Models to Categorize Life Satisfaction in Older Adults in Korea