J Korean Med Sci.
2023 Mar;38(12):e92. 10.3346/jkms.2023.38.e92.
Impact of COVID-19 on Out-of-Hospital Cardiac Arrest in Korea
- Affiliations
-
- 1119 EMS Division, National Fire Agency 119, Sejong, Korea
- 2Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea
- 3Laboratory of Emergency Medical Services, Seoul National University Hospital Biomedical Research Institute, Seoul, Korea
- KMID: 2541040
- DOI: http://doi.org/10.3346/jkms.2023.38.e92
Abstract
- Background
Coronavirus disease 2019 (COVID-19) is a global public health crisis that has had a significant impact on emergency medical services (EMS). Several studies have reported an increase in the incidence of out-of-hospital cardiac arrest (OHCA) and a decreased survival due to COVID-19, which has been limited to a short period or has been reported in some regions. This study aimed to investigate the effect of COVID-19 on OHCA patients using a nationwide database.
Methods
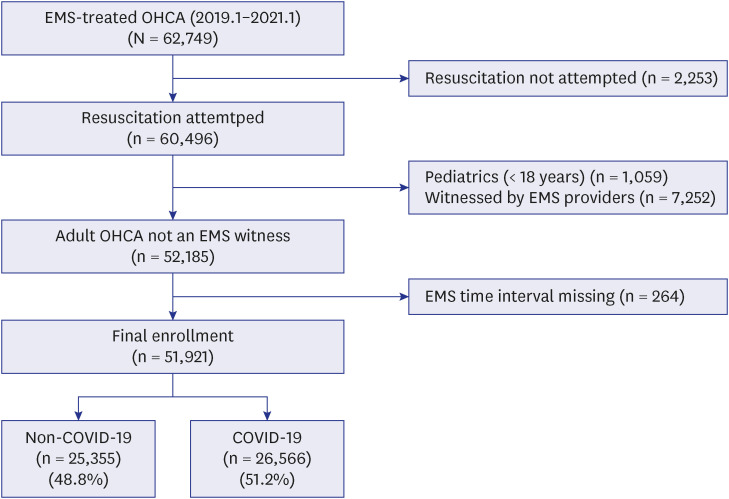
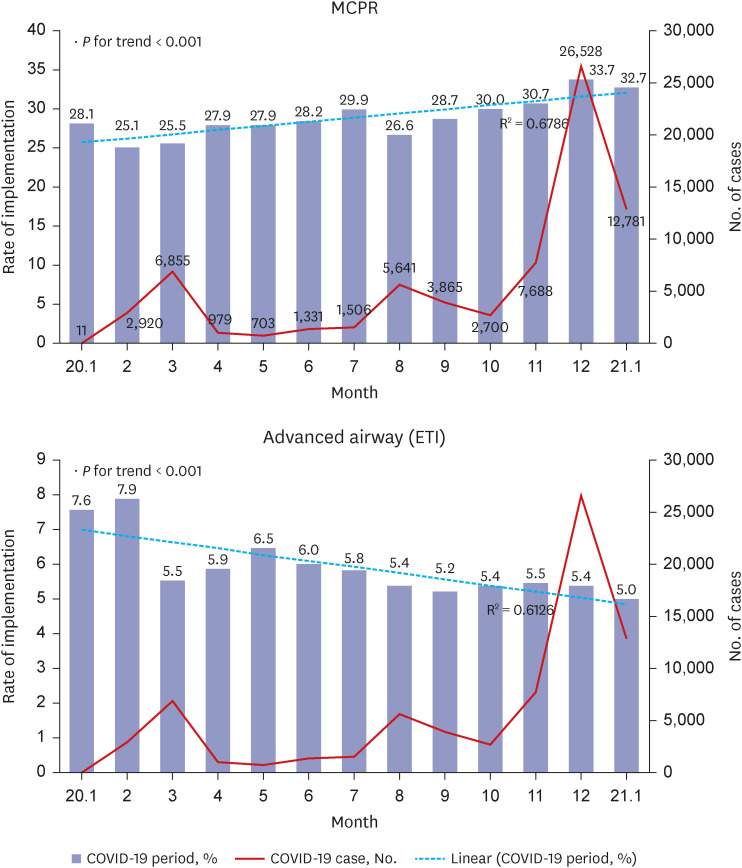
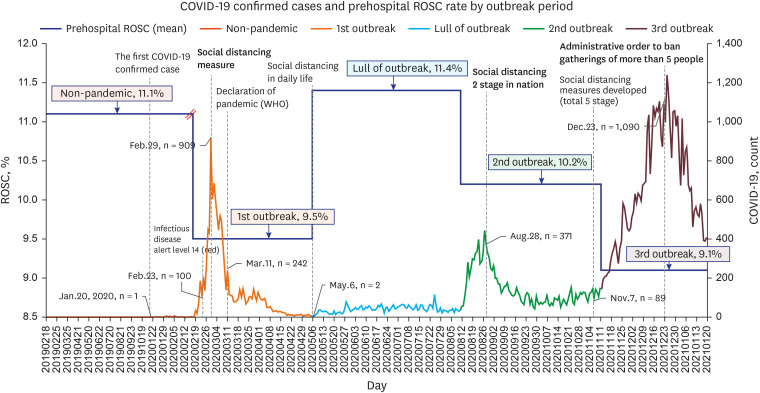
We included adult OHCA patients treated by EMS providers from January 19, 2019 to January 20, 2021. The years before and after the first confirmed case in Korea were set as the non-COVID-19 and COVID-19 periods, respectively. The main exposure of interest was the COVID-19 period, and the primary outcome was prehospital return of spontaneous circulation (ROSC). Other OHCA variables were compared before and after the COVID-19 pandemic and analyzed. We performed a multivariable logistic regression analysis to understand the independent effect of the COVID-19 period on prehospital ROSC.
Results
The final analysis included 51,921 eligible patients, including 25,355 (48.8%) during the non-COVID-19 period and 26,566 (51.2%) during the COVID-19 period. Prehospital ROSC deteriorated during the COVID-19 period (10.2% vs. 11.1%, P = 0.001). In the main analysis, the adjusted odds ratios (AORs) for prehospital ROSC showed no significant differences between the COVID-19 and non-COVID-19 periods (AOR [95% confidence interval], 1.02 [0.96–1.09]).
Conclusion
This study found that the proportion of prehospital ROSC was lower during the COVID-19 period than during the non-COVID-19 period; however, there was no statistical significance when adjusting for potential confounders. Continuous efforts are needed to restore the broken chain of survival in the prehospital phase and increase the survival rate of OHCA patients.
Keyword
Figure
Reference
-
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382(8):727–733. PMID: 31978945.2. Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021; 19(3):141–154. PMID: 33024307.3. Carter P, Anderson M, Mossialos E. Health system, public health, and economic implications of managing COVID-19 from a cardiovascular perspective. Eur Heart J. 2020; 41(27):2516–2518. PMID: 32320040.4. Haleem A, Javaid M, Vaishya R. Effects of COVID-19 pandemic in daily life. Curr Med Res Pract. 2020; 10(2):78–79. PMID: 32292804.5. Zambrano-Monserrate MA, Ruano MA, Sanchez-Alcalde L. Indirect effects of COVID-19 on the environment. Sci Total Environ. 2020; 728:138813. PMID: 32334159.6. Shivalkar S, Pingali MS, Verma A, Singh A, Singh V, Paital B, et al. Outbreak of COVID-19: a detailed overview and its consequences. Adv Exp Med Biol. 2021; 1353:23–45. PMID: 35137366.7. World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Updated 2020. Accessed March 11, 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 .8. Gräsner JT, Lefering R, Koster RW, Masterson S, Böttiger BW, Herlitz J, et al. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: a prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation. 2016; 105:188–195. PMID: 27321577.9. Hawkes C, Booth S, Ji C, Brace-McDonnell SJ, Whittington A, Mapstone J, et al. Epidemiology and outcomes from out-of-hospital cardiac arrests in England. Resuscitation. 2017; 110:133–140. PMID: 27865775.10. Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010; 3(1):63–81. PMID: 20123673.11. Berg KM, Cheng A, Panchal AR, Topjian AA, Aziz K, Bhanji F, et al. Part 7: Systems of Care: 2020 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020; 142(16 Suppl 2):S580–S604. PMID: 33081524.12. Hwang SO, Cha KC, Jung WJ, Roh YI, Kim TY, Chung SP, et al. 2020 Korean Guidelines for Cardiopulmonary Resuscitation. Part 2. Environment for cardiac arrest survival and the chain of survival. Clin Exp Emerg Med. 2021; 8(S):S8–14. PMID: 34034446.13. Kashef MA, Lotfi AS. Evidence-based approach to out-of-hospital cardiac arrest. Curr Treat Options Cardiovasc Med. 2021; 23(6):43. PMID: 33994773.14. Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020; 5(8):e437–e443. PMID: 32473113.15. Lim ZJ, Ponnapa Reddy M, Afroz A, Billah B, Shekar K, Subramaniam A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: a systematic review and meta-analysis. Resuscitation. 2020; 157:248–258. PMID: 33137418.16. Fothergill RT, Smith AL, Wrigley F, Perkins GD. Out-of-hospital cardiac arrest in London during the COVID-19 pandemic. Resusc Plus. 2021; 5:100066. PMID: 33521706.17. Ahn JY, Ryoo HW, Cho JW, Kim JH, Lee SH, Jang TC. Impact of the COVID-19 outbreak on adult out-of-hospital cardiac arrest outcomes in Daegu, South Korea: an observational study. Clin Exp Emerg Med. 2021; 8(2):137–144. PMID: 34237819.18. Lim SL, Shahidah N, Saffari SE, Ng QX, Ho AF, Leong BS, et al. Impact of COVID-19 on out-of-hospital cardiac arrest in Singapore. Int J Environ Res Public Health. 2021; 18(7):3646. PMID: 33807454.19. Lim D, Park SY, Choi B, Kim SH, Ryu JH, Kim YH, et al. The comparison of emergency medical service responses to and outcomes of out-of-hospital cardiac arrest before and during the COVID-19 pandemic in an area of Korea. J Korean Med Sci. 2021; 36(36):e255. PMID: 34519188.20. Kim YT, Shin SD, Hong SO, Ahn KO, Ro YS, Song KJ, et al. Effect of national implementation of Utstein recommendation from the global resuscitation alliance on ten steps to improve outcomes from out-of-hospital cardiac arrest: a ten-year observational study in Korea. BMJ Open. 2017; 7(8):e016925.21. Kim Y, Kim YY, Yeom H, Jang J, Hwang I, Park K, et al. COVID-19 1-Year Outbreak Report as of January 19, 2021 in the Republic of Korea. Public Health Wkly Rep. 2021; 14:478–481.22. Kim YS, Kim KH, Song KJ, Shin SD, Park JH. The number and level of first-contact emergency medical services crew and clinical outcomes in out-of-hospital cardiac arrest with dual dispatch response. Clin Exp Emerg Med. 2022; 9(4):314–322. PMID: 36216399.23. Song KJ, Shin SD, Park CB, Kim JY, Kim DK, Kim CH, et al. Dispatcher-assisted bystander cardiopulmonary resuscitation in a metropolitan city: a before-after population-based study. Resuscitation. 2014; 85(1):34–41. PMID: 23792111.24. Shin SD, Ong ME, Tanaka H, Ma MH, Nishiuchi T, Alsakaf O, et al. Comparison of emergency medical services systems across Pan-Asian countries: a Web-based survey. Prehosp Emerg Care. 2012; 16(4):477–496. PMID: 22861161.25. Callaway CW, Soar J, Aibiki M, Böttiger BW, Brooks SC, Deakin CD, et al. Part 4: advanced life support: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015; 132(16):Suppl 1. S84–145. PMID: 26472860.26. Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004; 110(21):3385–3397. PMID: 15557386.27. Perman SM. Overcoming fears to save lives: COVID-19 and the threat to bystander CPR in out-of-hospital cardiac arrest. Circulation. 2020; 142(13):1233–1235. PMID: 32795100.28. Scquizzato T, Olasveengen TM, Ristagno G, Semeraro F. The other side of novel coronavirus outbreak: fear of performing cardiopulmonary resuscitation. Resuscitation. 2020; 150:92–93. PMID: 32259607.29. Lee MJ, Shin TY, Lee CH, Moon JD, Roh SG, Kim CW, et al. 2020 Korean guidelines for cardiopulmonary resuscitation. Part 9. Education and system implementation for enhanced chain of survival. Clin Exp Emerg Med. 2021; 8(S):S116–S124. PMID: 34034453.30. Moon S, Ryoo HW, Ahn JY, Park JB, Lee DE, Kim JH, et al. A 5-year change of knowledge and willingness by sampled respondents to perform bystander cardiopulmonary resuscitation in a metropolitan city. PLoS One. 2019; 14(2):e0211804. PMID: 30730932.31. Bhanji F, Mancini ME, Sinz E, Rodgers DL, McNeil MA, Hoadley TA, et al. Part 16: education, implementation, and teams: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122(18):Suppl 3. S920–S933. PMID: 20956232.32. Eisenberg MS, Bergner L, Hallstrom A. Cardiac resuscitation in the community. Importance of rapid provision and implications for program planning. JAMA. 1979; 241(18):1905–1907. PMID: 430772.33. Vukmir RB. Survival from prehospital cardiac arrest is critically dependent upon response time. Resuscitation. 2006; 69(2):229–234. PMID: 16500015.34. Sladjana A, Gordana P, Ana S. Emergency response time after out-of-hospital cardiac arrest. Eur J Intern Med. 2011; 22(4):386–393. PMID: 21767757.35. Tanaka H, Ong ME, Siddiqui FJ, Ma MH, Kaneko H, Lee KW, et al. Modifiable factors associated with survival after out-of-hospital cardiac arrest in the pan-asian resuscitation outcomes study. Ann Emerg Med. 2018; 71(5):608–617.e15. PMID: 28985969.36. Holmén J, Herlitz J, Ricksten SE, Strömsöe A, Hagberg E, Axelsson C, et al. Shortening ambulance response time increases survival in out-of-hospital cardiac arrest. J Am Heart Assoc. 2020; 9(21):e017048. PMID: 33107394.37. Eastwood K, Morgans A, Smith K, Hodgkinson A, Becker G, Stoelwinder J. A novel approach for managing the growing demand for ambulance services by low-acuity patients. Aust Health Rev. 2016; 40(4):378–384. PMID: 26568037.38. Perlini S, Canevari F, Cortesi S, Sgromo V, Brancaglione A, Contri E, et al. Emergency department and out-of-hospital emergency system (112-AREU 118) integrated response to coronavirus disease 2019 in a Northern Italy centre. Intern Emerg Med. 2020; 15(5):825–833. PMID: 32507926.39. Jensen T, Holgersen MG, Jespersen MS, Blomberg SN, Folke F, Lippert F, et al. Strategies to handle increased demand in the COVID-19 crisis: a coronavirus EMS Support track and a web-based self-triage system. Prehosp Emerg Care. 2021; 25(1):28–38. PMID: 32870754.40. Prezant DJ, Lancet EA, Zeig-Owens R, Lai PH, Appel D, Webber MP, et al. System impacts of the COVID-19 pandemic on New York City’s emergency medical services. J Am Coll Emerg Physicians Open. 2020; 1(6):1205–1213. PMID: 33392524.41. Leeies M, Ffrench C, Strome T, Weldon E, Bullard M, Grierson R. Prehospital application of the canadian triage and acuity scale by emergency medical services. CJEM. 2017; 19(1):26–31. PMID: 27508353.42. World Health Organization. Infection Prevention and Control During Health Care When Coronavirus Disease (COVID-19) Is Suspected or Confirmed: Interim Guidance, 29 June 2020. Geneva, Switzerland: World Health Organization;2020.43. Christian MD, Loutfy M, McDonald LC, Martinez KF, Ofner M, Wong T, et al. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg Infect Dis. 2004; 10(2):287–293. PMID: 15030699.44. Nam HS, Yeon MY, Park JW, Hong JY, Son JW. Healthcare worker infected with middle east respiratory syndrome during cardiopulmonary resuscitation in Korea, 2015. Epidemiol Health. 2017; 39:e2017052. PMID: 29129042.45. Burns TA, Touzeau C, Kaufman BT, Butsch AL, Vesselinov R, Stone RM. Decreases in out of hospital cardiac arrest (OHCA) outcome metrics persist when known COVID patients are excluded from analysis. Am J Emerg Med. 2022; 51:64–68. PMID: 34678575.46. Ko HY, Park JE, Jeong DU, Shin TG, Sim MS, Jo IJ, et al. Impact of personal protective equipment on out-of-hospital cardiac arrest resuscitation in coronavirus pandemic. Medicina (Kaunas). 2021; 57(12):1291. PMID: 34946236.47. Tian Y, Tu X, Zhou X, Yu J, Luo S, Ma L, et al. Wearing a N95 mask increases rescuer’s fatigue and decreases chest compression quality in simulated cardiopulmonary resuscitation. Am J Emerg Med. 2021; 44:434–438. PMID: 33046304.48. Sahu AK, Suresh S, Mathew R, Aggarwal P, Nayer J. Impact of personal protective equipment on the effectiveness of chest compression: a systematic review and meta-analysis. Am J Emerg Med. 2021; 39:190–196. PMID: 33046289.49. Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, Becker LB, et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020; 141(25):e933–e943. PMID: 32270695.50. Wang PL, Brooks SC. Mechanical versus manual chest compressions for cardiac arrest. Cochrane Database Syst Rev. 2018; 8(8):CD007260. PMID: 30125048.51. Atkins DL, Sasson C, Hsu A, Aziz K, Becker LB, Berg RA, et al. 2022 interim guidance to health care providers for basic and advanced cardiac life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association in Collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, the Society of Critical Care Anesthesiologists, and American Society of Anesthesiologists. Circ Cardiovasc Qual Outcomes. 2022; 15(4):e008900. PMID: 35072519.52. Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012; 7(4):e35797. PMID: 22563403.53. Brewster DJ, Chrimes N, Do TB, Fraser K, Groombridge CJ, Higgs A, et al. Consensus statement: safe Airway Society principles of airway management and tracheal intubation specific to the COVID-19 adult patient group. Med J Aust. 2020; 212(10):472–481. PMID: 32356900.54. Ball J, Nehme Z, Bernard S, Stub D, Stephenson M, Smith K. Collateral damage: Hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. 2020; 156:157–163. PMID: 32961304.55. Chan PS, Girotra S, Tang Y, Al-Araji R, Nallamothu BK, McNally B. Outcomes for out-of-hospital cardiac arrest in the United States during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2021; 6(3):296–303. PMID: 33188678.56. Scquizzato T, Landoni G, Scandroglio AM, Franco A, Calabrò MG, Paoli A, et al. Outcomes of out-of-hospital cardiac arrest in patients with SARS-CoV-2 infection: a systematic review and meta-analysis. Eur J Emerg Med. 2021; 28(6):423–431. PMID: 34690258.57. Baert V, Beuscart JB, Recher M, Javaudin F, Hugenschmitt D, Bony T, et al. Coronavirus disease 2019 and out-of-hospital cardiac arrest: no survivors. Crit Care Med. 2022; 50(5):791–798. PMID: 34605777.58. Myat A, Song KJ, Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet. 2018; 391(10124):970–979. PMID: 29536861.59. Kim KH, Ro YS, Park JH, Kim TH, Jeong J, Hong KJ, et al. Association between case volume of ambulance stations and clinical outcomes of out-of-hospital cardiac arrest: a nationwide multilevel analysis. Resuscitation. 2021; 163:71–77. PMID: 33895233.60. Perkins GD, Jacobs IG, Nadkarni VM, Berg RA, Bhanji F, Biarent D, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation. 2015; 96:328–340. PMID: 25438254.61. Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020; 41(32):3045–3054. PMID: 32562486.62. Baldi E, Primi R, Bendotti S, Currao A, Compagnoni S, Gentile FR, et al. Relationship between out-of-hospital cardiac arrests and COVID-19 during the first and second pandemic wave. The importance of monitoring COVID-19 incidence. PLoS One. 2021; 16(11):e0260275. PMID: 34797840.63. Baert V, Beuscart JB, Recher M, Javaudin F, Hugenschmitt D, Bony T, et al. Coronavirus disease 2019 and out-of-hospital cardiac arrest: no survivors. Crit Care Med. 2022; 50(5):791–798. PMID: 34605777.64. Van de Voorde P, Bossaert L, Mentzelopoulos S, Blom MT, Couper K, Djakow J, et al. Ethik der Reanimation und Entscheidungen am Lebensende. Notf Rettmed. 2020; 23(4):263–267.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The impact of COVID-19 through epidemiological changes in out-of-hospital cardiac arrest patients: a study in a single emergency medical center
- Analysis of reasons for the termination of resuscitation in non-traumatic out-of-hospital cardiac arrests before and after the COVID-19 pandemic
- Cardiovascular Manifestations of COVID-19
- No frequency change of prehospital treatments by emergency medical services providers for traumatic cardiac arrest patients before and after the COVID-19 pandemic in Korea: an observational study
- Variance of the COVID-19 occurrence in the community: influence on the emergency medical service and the survival of out-of-hospital cardiac arrest patients