Korean J Pain.
2023 Apr;36(2):173-183. 10.3344/kjp.23011.
Long-term consistency of clinical sensory testing measures for pain assessment
- Affiliations
-
- 1San Jorge University, Campus Universitario, Zaragoza, Spain
- 2Department of Health Science and Technology, Faculty of Medicine, Aalborg University, Aalborg, Denmark
- 3Department of Physiotherapy and Occupational Therapy, Aalborg University Hospital, Aalborg, Denmark
- 4Department of Physiatry and Nursing, Faculty of Health Sciences, University of Zaragoza, Zaragoza, Spain
- 5Department of Physiotherapy, University College of Northern Denmark, Aalborg, Denmark
- KMID: 2541026
- DOI: http://doi.org/10.3344/kjp.23011
Abstract
- Background
Understanding the stability of quantitative sensory tests (QSTs) over time is important to aid clinicians in selecting a battery of tests for assessing and monitoring patients. This study evaluated the short- and long-term reliability of selected QSTs.
Methods
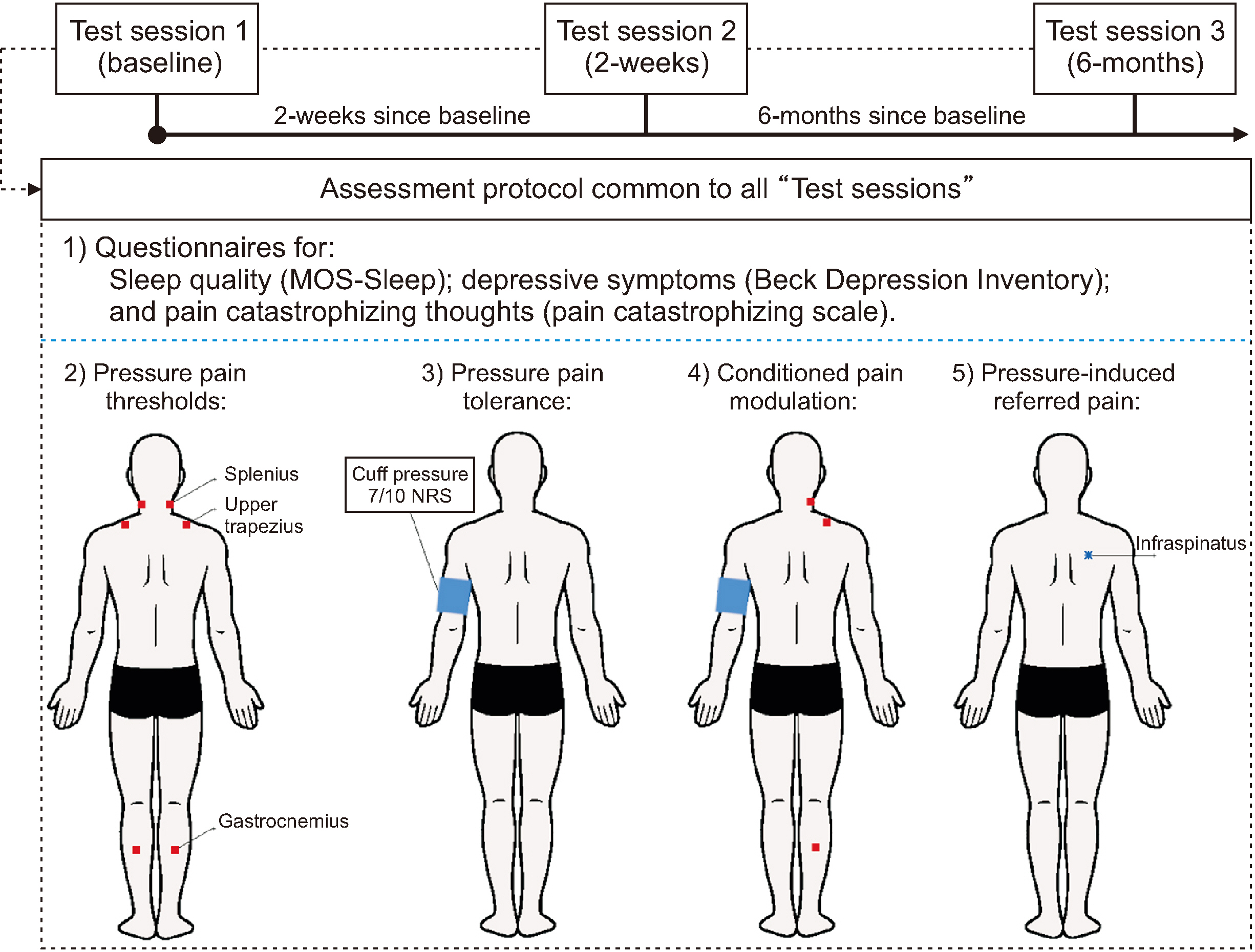
Twenty healthy women participated in three experimental sessions: Baseline, 2 weeks, and 6 months. Measurements included pressure pain thresholds (PPT) in the neck, upper back, and leg; Pressure-cuff pain tolerance around the upper-arm; conditioned pain modulation during a pressure-cuff stimulus; and referred pain following a suprathreshold pressure stimulation. Intraclass correlation coefficients (ICC) and minimum detectable change (MDC) were calculated.
Results
Reliability for PPT was excellent for all sites at 2 weeks (ICC, 0.96–0.99; MDC, 22–55 kPa) and from good to excellent at 6 months (ICC, 0.88–0.95; MDC, 47–91 kPa). ICC for pressure-cuff pain tolerance indicated excellent reliability at both times (0.91–0.97). For conditioned pain modulation, reliability was moderate for all sites at 2 weeks (ICC, 0.57–0.74; MDC, 24%–35%), while it was moderate at the neck (ICC, 0.54; MDC, 27%) and poor at the upper back and leg at 6 months. ICC for referred pain areas was excellent at 2 weeks (0.90) and good at 6 months (0.86).
Conclusions
PPT, pressure pain tolerance, and pressure-induced referred pain should be considered reliable procedures to assess the pain-sensory profile over time. In contrast, conditioned pain modulation was shown to be unstable. Future studies prospectively analyzing the pain-sensory profile will be able to better calculate appropriate sample sizes.
Keyword
Figure
Reference
-
1. McRae M, Hancock MJ. 2017; Adults attending private physiotherapy practices seek diagnosis, pain relief, improved function, education and prevention: a survey. J Physiother. 63:250–6. DOI: 10.1016/j.jphys.2017.08.002. PMID: 28967562. PMID: 8b32b38671cf405ea5abbed6589ae8d5.2. Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. 2021; Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 396:2006–17. Erratum in: Lancet 2021; 397: 198. DOI: 10.1016/S0140-6736(20)32340-0. PMID: 33275908.3. McMahon SB, Dargan P, Lanas A, Wiffen P. 2021; The burden of musculoskeletal pain and the role of topical non-steroidal anti-inflammatory drugs (NSAIDs) in its treatment. Ten underpinning statements from a global pain faculty. Curr Med Res Opin. 37:287–92. DOI: 10.1080/03007995.2020.1847718. PMID: 33155849.4. Mills SEE, Nicolson KP, Smith BH. 2019; Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 123:e273–83. DOI: 10.1016/j.bja.2019.03.023. PMID: 31079836. PMCID: PMC6676152.5. Roy JS, Bouyer LJ, Langevin P, Mercier C. 2017; Beyond the joint: the role of central nervous system reorganizations in chronic musculoskeletal disorders. J Orthop Sports Phys Ther. 47:817–21. DOI: 10.2519/jospt.2017.0608. PMID: 29089002.6. Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD. 2016; The role of psychosocial processes in the development and maintenance of chronic pain. J Pain. 17(9 Suppl):T70–92. DOI: 10.1016/j.jpain.2016.01.001. PMID: 27586832. PMCID: PMC5012303.7. Rabey M, Slater H, O'Sullivan P, Beales D, Smith A. 2015; Somatosensory nociceptive characteristics differentiate subgroups in people with chronic low back pain: a cluster analysis. Pain. 156:1874–84. DOI: 10.1097/j.pain.0000000000000244. PMID: 26020225.8. Lluch E, Nijs J, Courtney CA, Rebbeck T, Wylde V, Baert I, et al. 2018; Clinical descriptors for the recognition of central sensitization pain in patients with knee osteoarthritis. Disabil Rehabil. 40:2836–45. DOI: 10.1080/09638288.2017.1358770. PMID: 28768437.9. Daenen L, Nijs J, Roussel N, Wouters K, Van Loo M, Cras P. 2013; Dysfunctional pain inhibition in patients with chronic whiplash-associated disorders: an experimental study. Clin Rheumatol. 32:23–31. DOI: 10.1007/s10067-012-2085-2. PMID: 22983264.10. Beales D, Mitchell T, Moloney N, Rabey M, Ng W, Rebbeck T. 2021; Masterclass: a pragmatic approach to pain sensitivity in people with musculoskeletal disorders and implications for clinical management for musculoskeletal clinicians. Musculoskelet Sci Pract. 51:102221. DOI: 10.1016/j.msksp.2020.102221. PMID: 32972875.11. Georgopoulos V, Akin-Akinyosoye K, Zhang W, McWilliams DF, Hendrick P, Walsh DA. 2019; Quantitative sensory testing and predicting outcomes for musculoskeletal pain, disability, and negative affect: a systematic review and meta-analysis. Pain. 160:1920–32. DOI: 10.1097/j.pain.0000000000001590. PMID: 31045746. PMCID: PMC6701980.12. Pavlaković G, Petzke F. 2010; The role of quantitative sensory testing in the evaluation of musculoskeletal pain conditions. Curr Rheumatol Rep. 12:455–61. DOI: 10.1007/s11926-010-0131-0. PMID: 20857243. PMCID: PMC3128735.13. Graven-Nielsen T, Arendt-Nielsen L. 2010; Assessment of mechanisms in localized and widespread musculoskeletal pain. Nat Rev Rheumatol. 6:599–606. DOI: 10.1038/nrrheum.2010.107. PMID: 20664523.14. Kanner R. Argoff CE, McCleane G, editors. 2009. Chapter 1 - definitions. Pain management secrets. 3rd ed. Mosby;p. 9–14. DOI: 10.1016/B978-0-323-04019-8.00001-9.15. Nir RR, Yarnitsky D. 2015; Conditioned pain modulation. Curr Opin Support Palliat Care. 9:131–7. DOI: 10.1097/SPC.0000000000000126. PMID: 25699686.16. Doménech-García V, Palsson TS, Boudreau SA, Bellosta-López P, Herrero P, Graven-Nielsen T. 2020; Healthy pain-free individuals with a history of distal radius fracture demonstrate an expanded distribution of experimental referred pain toward the wrist. Pain Med. 21:2850–62. DOI: 10.1093/pm/pnaa228. PMID: 33146396.17. Zhu GC, Böttger K, Slater H, Cook C, Farrell SF, Hailey L, et al. 2019; Concurrent validity of a low-cost and time-efficient clinical sensory test battery to evaluate somatosensory dysfunction. Eur J Pain. 23:1826–38. DOI: 10.1002/ejp.1456. PMID: 31325385. PMCID: PMC6852113.18. Marcuzzi A, Wrigley PJ, Dean CM, Adams R, Hush JM. 2017; The long-term reliability of static and dynamic quantitative sensory testing in healthy individuals. Pain. 158:1217–23. DOI: 10.1097/j.pain.0000000000000901. PMID: 28328574.19. Nothnagel H, Puta C, Lehmann T, Baumbach P, Menard MB, Gabriel B, et al. 2017; How stable are quantitative sensory testing measurements over time? Report on 10-week reliability and agreement of results in healthy volunteers. J Pain Res. 10:2067–78. DOI: 10.2147/JPR.S137391. PMID: 28919806. PMCID: PMC5587201.20. Christensen SWM, Bellosta-López P, Doménech-García V, Herrero P, Palsson TS. 2021; Changes in pain sensitivity and conditioned pain modulation during recovery from whiplash-associated disorders. Clin J Pain. 37:730–9. DOI: 10.1097/AJP.0000000000000970. PMID: 34334693.21. Kottner J, Audigé L, Brorson S, Donner A, Gajewski BJ, Hróbjartsson A, et al. 2011; Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. J Clin Epidemiol. 64:96–106. DOI: 10.1016/j.jclinepi.2010.03.002. PMID: 21130355.22. Tanaka Y, Shigetoh H, Sato G, Fujii R, Imai R, Osumi M, et al. 2021; Classification of circadian pain rhythms and pain characteristics in chronic pain patients: an observational study. Medicine (Baltimore). 100:e26500. DOI: 10.1097/MD.0000000000026500. PMID: 34160466. PMCID: PMC8238338.23. Rejas J, Ribera MV, Ruiz M, Masrramón X. 2007; Psychometric properties of the MOS (Medical Outcomes Study) Sleep Scale in patients with neuropathic pain. Eur J Pain. 11:329–40. DOI: 10.1016/j.ejpain.2006.05.002. PMID: 16765622.24. Azocar F, Areán P, Miranda J, Muñoz RF. 2001; Differential item functioning in a Spanish translation of the Beck Depression Inventory. J Clin Psychol. 57:355–65. DOI: 10.1002/jclp.1017. PMID: 11241365.25. García Campayo J, Rodero B, Alda M, Sobradiel N, Montero J, Moreno S. 2008; Validation of the Spanish version of the Pain Catastrophizing Scale in fibromyalgia. Med Clin (Barc). 131:487–92. Spanish. DOI: 10.1157/13127277. PMID: 19007576.26. Balaguier R, Madeleine P, Vuillerme N. 2016; Is one trial sufficient to obtain excellent pressure pain threshold reliability in the low back of asymptomatic individuals? A test-retest study. PLoS One. 11:e0160866. DOI: 10.1371/journal.pone.0160866. PMID: 27513474. PMCID: PMC4981327. PMID: 54670db9c6824b0a816ddff30805ecdd.27. Yarnitsky D, Bouhassira D, Drewes AM, Fillingim RB, Granot M, Hansson P, et al. 2015; Recommendations on practice of conditioned pain modulation (CPM) testing. Eur J Pain. 19:805–6. DOI: 10.1002/ejp.605. PMID: 25330039.28. Doménech-García V, Palsson TS, Herrero P, Graven-Nielsen T. 2016; Pressure-induced referred pain is expanded by persistent soreness. Pain. 157:1164–72. DOI: 10.1097/j.pain.0000000000000497. PMID: 26808146.29. Doménech-García V, Skuli Palsson T, Boudreau SA, Herrero P, Graven-Nielsen T. 2018; Pressure-induced referred pain areas are more expansive in individuals with a recovered fracture. Pain. 159:1972–9. DOI: 10.1097/j.pain.0000000000001234. PMID: 29608510.30. Boudreau SA, Badsberg S, Christensen SW, Egsgaard LL. 2016; Digital pain drawings: assessing touch-screen technology and 3D body schemas. Clin J Pain. 32:139–45. DOI: 10.1097/AJP.0000000000000230. PMID: 25756558.31. Koo TK, Li MY. 2016; A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 15:155–63. Erratum in: J Chiropr Med 2017; 16: 346. DOI: 10.1016/j.jcm.2017.10.001. PMID: 29276468. PMCID: PMC5731844.32. Furlan L, Sterr A. 2018; The applicability of standard error of measurement and minimal detectable change to motor learning research-a behavioral study. Front Hum Neurosci. 12:95. DOI: 10.3389/fnhum.2018.00095. PMID: 29623034. PMCID: PMC5875129. PMID: e5c75f6fd71d4eefb55d8b336839b2fa.33. Waller R, Straker L, O'Sullivan P, Sterling M, Smith A. 2015; Reliability of pressure pain threshold testing in healthy pain free young adults. Scand J Pain. 9:38–41. Erratum in: Scand J Pain 2016; 13: 17. DOI: 10.1016/j.sjpain.2016.06.008. PMID: 28850526.34. Black CD, Pickowitz KE. 2015; Day-to-day reliability of pressure pain threshold and pain ratings in college-aged men. Int J Rehabil Res. 38:213–8. DOI: 10.1097/MRR.0000000000000111. PMID: 25715228.35. Walton DM, Levesque L, Payne M, Schick J. 2014; Clinical pressure pain threshold testing in neck pain: comparing protocols, responsiveness, and association with psychological variables. Phys Ther. 94:827–37. DOI: 10.2522/ptj.20130369. PMID: 24557645. PMCID: PMC4040424.36. Kvistgaard Olsen J, Fener DK, Waehrens EE, Wulf Christensen A, Jespersen A, Danneskiold-Samsøe B, et al. 2017; Reliability of pain measurements using computerized cuff algometry: a DoloCuff reliability and agreement study. Pain Pract. 17:708–17. DOI: 10.1111/papr.12514. PMID: 27611494.37. Graven-Nielsen T, Vaegter HB, Finocchietti S, Handberg G, Arendt-Nielsen L. 2015; Assessment of musculoskeletal pain sensitivity and temporal summation by cuff pressure algometry: a reliability study. Pain. 156:2193–202. DOI: 10.1097/j.pain.0000000000000294. PMID: 26172551.38. Arroyo-Fernandez R, Bravo-Esteban E, Domenech-Garcia V, Ferri-Morales A. 2020; Pressure-induced referred pain as a biomarker of pain sensitivity in fibromyalgia. Pain Physician. 23:E353–62. DOI: 10.36076/ppj.2020/23/E353. PMID: 32709181.39. Kennedy DL, Kemp HI, Ridout D, Yarnitsky D, Rice ASC. 2016; Reliability of conditioned pain modulation: a systematic review. Pain. 157:2410–9. DOI: 10.1097/j.pain.0000000000000689. PMID: 27559835. PMCID: PMC5228613.40. Lewis GN, Heales L, Rice DA, Rome K, McNair PJ. 2012; Reliability of the conditioned pain modulation paradigm to assess endogenous inhibitory pain pathways. Pain Res Manag. 17:98–102. DOI: 10.1155/2012/610561. PMID: 22518372. PMCID: PMC3393056. PMID: 34b70165674e448c8b28f1466f6caf08.41. Valencia C, Kindler LL, Fillingim RB, George SZ. 2013; Stability of conditioned pain modulation in two musculoskeletal pain models: investigating the influence of shoulder pain intensity and gender. BMC Musculoskelet Disord. 14:182. DOI: 10.1186/1471-2474-14-182. PMID: 23758907. PMCID: PMC3682910.42. Roldan CJ, Abdi S. 2015; Quantitative sensory testing in pain management. Pain Manag. 5:483–91. DOI: 10.2217/pmt.15.37. PMID: 26399563.43. Mason KJ, O'Neill TW, Lunt M, Jones AKP, McBeth J. 2018; Psychosocial factors partially mediate the relationship between mechanical hyperalgesia and self-reported pain. Scand J Pain. 18:59–69. DOI: 10.1515/sjpain-2017-0109. PMID: 29794289.44. Polianskis R, Graven-Nielsen T, Arendt-Nielsen L. 2002; Spatial and temporal aspects of deep tissue pain assessed by cuff algometry. Pain. 100:19–26. DOI: 10.1016/S0304-3959(02)00162-8. PMID: 12435455.45. Jensen B. 2016; Chronic pain assessment from bench to bedside: lessons along the translation continuum. Transl Behav Med. 6:596–604. DOI: 10.1007/s13142-015-0370-8. PMID: 27848210. PMCID: PMC5110487.46. Palsson TS, Christensen SWM, De Martino E, Graven-Nielsen T. 2021; Pain and disability in low back pain can be reduced despite no significant improvements in mechanistic pain biomarkers. Clin J Pain. 37:330–8. DOI: 10.1097/AJP.0000000000000927. PMID: 33830092.47. McPhee ME, Graven-Nielsen T. 2019; Recurrent low back pain patients demonstrate facilitated pronociceptive mechanisms when in pain, and impaired antinociceptive mechanisms with and without pain. Pain. 160:2866–76. DOI: 10.1097/j.pain.0000000000001679. PMID: 31408054.48. Walter SD, Eliasziw M, Donner A. 1998; Sample size and optimal designs for reliability studies. Stat Med. 17:101–10. DOI: 10.1002/(SICI)1097-0258(19980115)17:1<101::AID-SIM727>3.0.CO;2-E. PMID: 9463853.49. Kamper SJ. 2019; Showing confidence (intervals). Braz J Phys Ther. 23:277–8. DOI: 10.1016/j.bjpt.2019.01.003. PMID: 30704908. PMCID: PMC6630104.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Simple Qualitative Sensory Assessment of Patients with Orofacial Sensory Dysfunction
- Prediction of Pain Expression Using the Extended Gate Control Theory of Pain and Fishbein's Model
- Factors Influencing Performance of Pain Assessment and Pain Intervention for Dementia Patients among Long-term Care Hospital Nurses
- The Assessment of Pain
- The Functional Assessment Process in Long-Term Care System for Older Persons