J Rhinol.
2023 Mar;30(1):41-44. 10.18787/jr.2023.00004.
Pneumothorax Induced by Automatic Positive Airway Pressure Therapy for Obstructive Sleep Apnea: A Rare Case Report and Review of the Literature
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Yeouido St. Mary Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- KMID: 2540857
- DOI: http://doi.org/10.18787/jr.2023.00004
Abstract
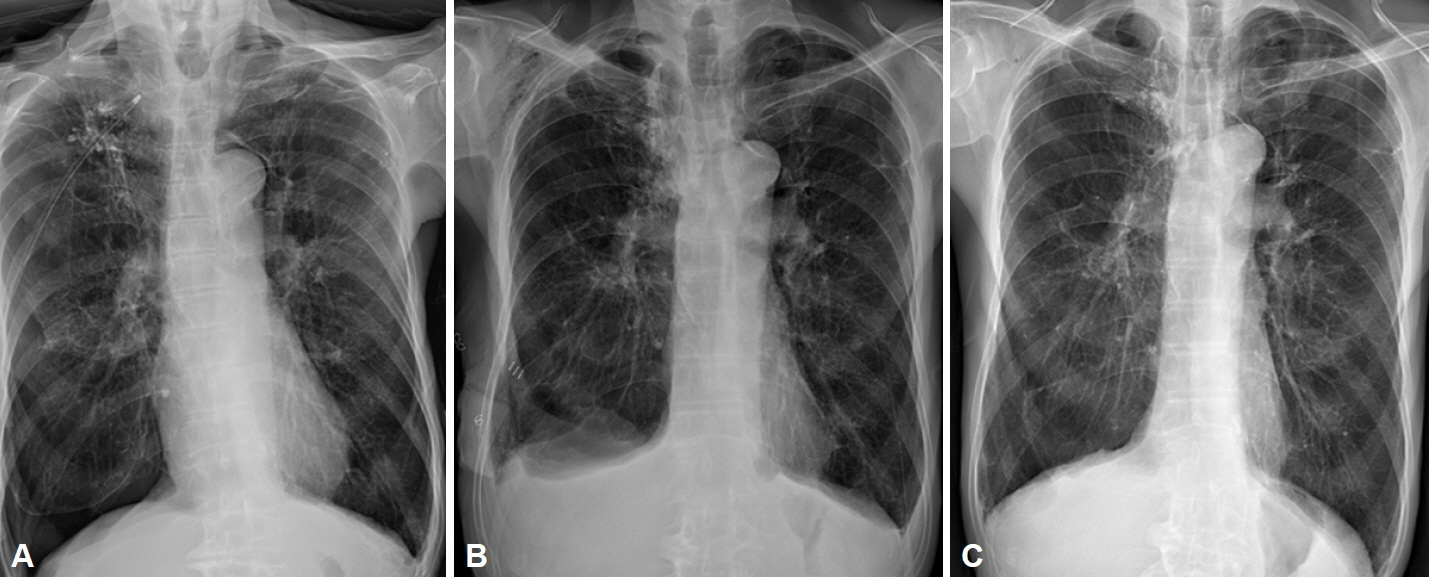
- Positive airway pressure (PAP) therapy is known to be an effective treatment for obstructive sleep apnea (OSA) that does not generally have serious complications. However, pneumothorax following lung barotrauma with the use of PAP has rarely been reported. We recently experienced the case of a 72-year old male patient with chronic obstructive pulmonary disease who developed pneumothorax after the use of automatic PAP (APAP). After 4 months of APAP use with a pressure of 4–8 cm H2O, he complained of sudden severe dyspnea at midnight. He eventually underwent surgical repair for pneumothorax. After 4 months, continuous PAP with low pressure of 5 cm H2O was applied without any complications. In summary, we emphasize the risk of barotrauma when PAP is used by OSA patients with lung disease.
Figure
Reference
-
References
1. Malhotra A, White DP. Obstructive sleep apnoea. Lancet. 2002; 360(9328):237–45.
Article2. Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981; 1(8225):862–5.
Article3. Batool-Anwar S, Goodwin JL, Kushida CA, Walsh JA, Simon RD, Nichols DA, et al. Impact of continuous positive airway pressure (CPAP) on quality of life in patients with obstructive sleep apnea (OSA). J Sleep Res. 2016; 25(6):731–8.
Article4. Langner S, Kolditz M, Kleymann J, Tausche K, Almeida AB, Schweigert M, et al. [Large pneumothorax in a sleep apnea patient with CPAP without previously known lung and thoracic diseases - a case report]. Pneumologie. 2020; 74(4):217–21. German.
Article5. Herrejón Silvestre A, Inchaurraga Alvarez I, Marín González M. [Spontaneous pneumothorax associated with the use of nighttime BiPAP with a nasal mask]. Arch Bronconeumol. 1998; 34(10):512. Spanish.6. Chicote Álvarez E, Arlabán Carpintero M, González-Castro A. Pulmonary edema ex vacuo after drainage of pneumothorax. Med Intensiva (Engl Ed). 2018; 42(9):e24–5.
Article7. Rajdev K, Idiculla PS, Sharma S, Von Essen SG, Murphy PJ, Bista S. Recurrent pneumothorax with CPAP therapy for obstructive sleep apnea. Case Rep Pulmonol. 2020; 2020:8898621.
Article8. Cho S, Yeo Y, Cho IY, Jeon K, Yoo JH. Association between chronic obstructive pulmonary disease risk and nutritional intake: using the 2007–2015 Korea national health and nutrition examination survey data. Korean J Fam Pract. 2021; 11(4):288–95.
Article9. Wang X, Zhang Y, Dong Z, Fan J, Nie S, Wei Y. Effect of continuous positive airway pressure on long-term cardiovascular outcomes in patients with coronary artery disease and obstructive sleep apnea: a systematic review and meta-analysis. Respir Res. 2018; 19(1):61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Massive REM Rebound on Continuous Positive Airway Pressure in Obstructive Sleep Apnea
- The Role of Endothelin-1 in Obstructive Sleep Apnea Syndrome and Pulmonary Hypertension
- CPAP Treatment in Pediatric Obstructive Sleep Apnea
- A Sleepy Man with Chronic Obstructive Pulmonary Disease-Obstructive Sleep Apnea Overlap Syndrome
- Surgical Treatment of Adult Obstructive Sleep Apnea