Clin Endosc.
2023 Mar;56(2):164-168. 10.5946/ce.2022.184.
Intraductal ultrasonography for biliary strictures
- Affiliations
-
- 1Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea
- KMID: 2540731
- DOI: http://doi.org/10.5946/ce.2022.184
Abstract
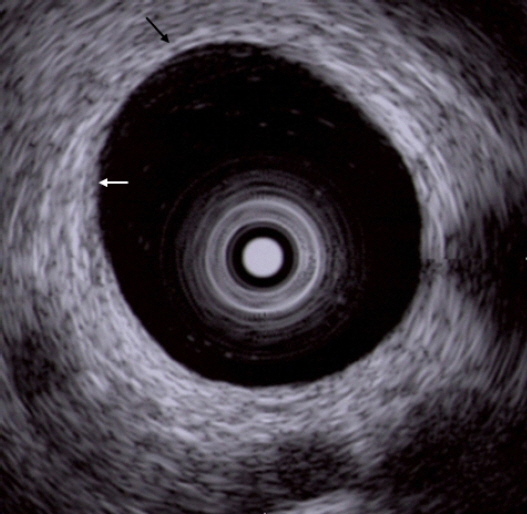
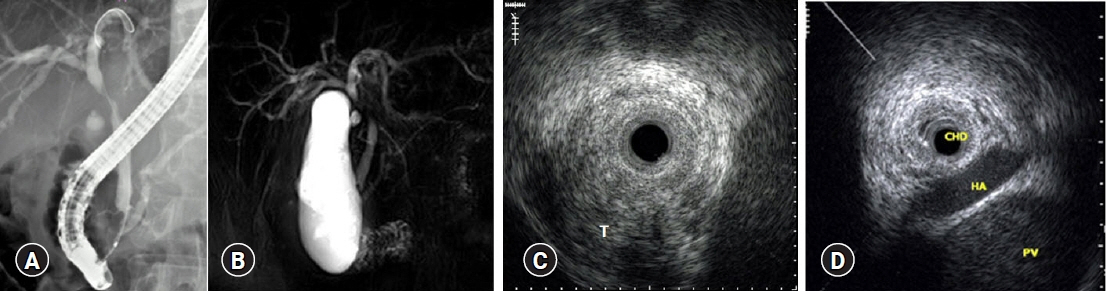
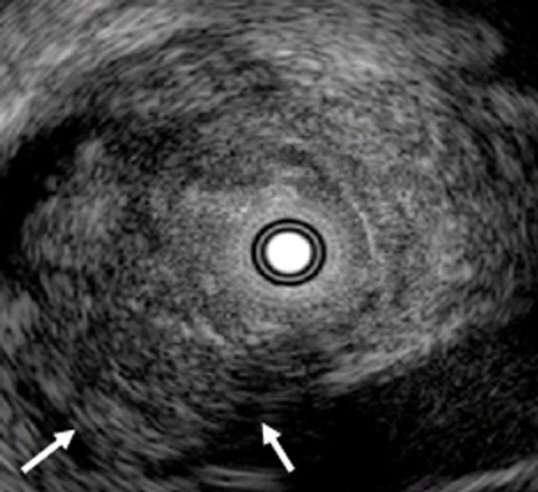
- When diagnosing the nature of biliary strictures, it is sometimes difficult to perform non-invasive methods such as ultrasound, spiral computed imaging, magnetic resonance imaging, or endoscopic ultrasonography. Thus, treatment decisions are usually based on biopsy results. However, brush cytology or biopsy, which is widely used for biliary stenosis, has limitations owing to its low sensitivity and negative predictive value for malignancy. Currently, the most accurate method is bile duct tissue biopsy under direct cholangioscopy. On the other hand, intraductal ultrasonography administered under the guidance of a guidewire has the advantages of easy administration and being less invasive, allowing for adequate examination of the biliary tract and surrounding organs. This review discusses the usefulness and drawbacks of intraductal ultrasonography for biliary strictures.
Figure
Reference
-
1. Tamada K, Ueno N, Tomiyama T, et al. Characterization of biliary strictures using intraductal ultrasonography: comparison with percutaneous cholangioscopic biopsy. Gastrointest Endosc. 1998; 47:341–349.2. Tamada K, Kurihara K, Tomiyama T, et al. How many biopsies should be performed during percutaneous transhepatic cholangioscopy to diagnose biliary tract cancer? Gastrointest Endosc. 1999; 50:653–658.3. Vazquez-Sequeiros E, Baron TH, Clain JE, et al. Evaluation of indeterminate bile duct strictures by intraductal US. Gastrointest Endosc. 2002; 56:372–379.4. Farrell RJ, Agarwal B, Brandwein SL, et al. Intraductal US is a useful adjunct to ERCP for distinguishing malignant from benign biliary strictures. Gastrointest Endosc. 2002; 56:681–687.5. Menzel J, Poremba C, Dietl KH, et al. Preoperative diagnosis of bile duct strictures: comparison of intraductal ultrasonography with conventional endosonography. Scand J Gastroenterol. 2000; 35:77–82.6. Tamada K, Ueno N, Ichiyama M, et al. Assessment of pancreatic parenchymal invasion by bile duct cancer using intraductal ultrasonography. Endoscopy. 1996; 28:492–496.7. Kuroiwa M, Goto H, Hirooka Y, et al. Intraductal ultrasonography for the diagnosis of proximal invasion in extrahepatic bile duct cancer. J Gastroenterol Hepatol. 1998; 13:715–719.8. Tamada K, Nagai H, Yasuda Y, et al. Transpapillary intraductal US prior to biliary drainage in the assessment of longitudinal spread of extrahepatic bile duct carcinoma. Gastrointest Endosc. 2001; 53:300–307.9. Noda Y, Fujita N, Kobayashi G, et al. Intraductal ultrasonography before biliary drainage and transpapillary biopsy in assessment of the longitudinal extent of bile duct cancer. Dig Endosc. 2008; 20:73–78.10. Tamada K, Tomiyama T, Ichiyama M, et al. Influence of biliary drainage catheter on bile duct wall thickness as measured by intraductal ultrasonography. Gastrointest Endosc. 1998; 47:28–32.11. Sakamoto E, Nimura Y, Hayakawa N, et al. The pattern of infiltration at the proximal border of hilar bile duct carcinoma: a histologic analysis of 62 resected cases. Ann Surg. 1998; 227:405–411.12. Tamada K, Ido K, Ueno N, et al. Assessment of hepatic artery invasion by bile duct cancer using intraductal ultrasonography. Endoscopy. 1995; 27:579–583.13. Fujita N, Noda Y, Kobayashi G, et al. Intraductal ultrasonography (IDUS) for the diagnosis of biliopancreatic diseases. Best Pract Res Clin Gastroenterol. 2009; 23:729–742.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prospective Comparison of Intraductal Ultrasonography-Guided Transpapillary Biopsy and Conventional Biopsy on Fluoroscopy in Suspected Malignant Biliary Strictures
- Endoscopic Ultrasonography in the Evaluation of Indeterminate Biliary Strictures
- Advances of Peroral Cholangioscopy and EUS for Indeterminate Biliary Lesions
- Recent advances of diagnostic approaches for indeterminate biliary tract obstruction
- Endoscopic Evaluation of Biliary Strictures: Current and Emerging Techniques