Korean J Women Health Nurs.
2022 Dec;28(4):317-328. 10.4069/kjwhn.2022.12.06.
Development and effects of a high-risk pregnancy emotive role-play program for nursing students: a quasi-experimental study
- Affiliations
-
- 1College of Nursing, Research Institute of Nursing Science, Daegu Catholic University, Daegu, Korea
- KMID: 2540220
- DOI: http://doi.org/10.4069/kjwhn.2022.12.06
Abstract
- Purpose
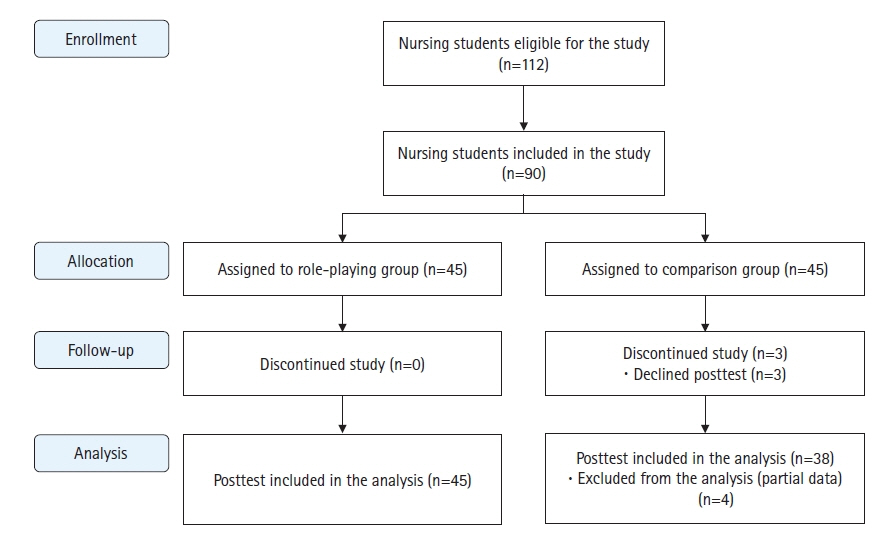
This study aimed to develop an emotive role-play program for nursing students focusingon high-risk pregnancy and analyze its effects on communication skills, clinical performance, andemotional intelligence.Methods: A quasi-experimental nonequivalent comparison group design was adopted with 83nursing students (experimental group, 45; comparison group, 38) who participated voluntarily in anextracurricular program. The preliminary survey was conducted on November 3 and November 4,2020, and the follow-up survey was conducted on November 12, 2020, for the comparison groupand on November 27, 2020, for the experimental group. A program that included five role-play scenarios related to induced labor, preeclampsia, premature rupture of membranes, preterm labor, andinfertility was developed by a group of experts and presented to the experimental group over 11 totalhours across 3 days. Each student participated in a role-play scenario as a patient, family member, ornurse and observed three other scenarios. The comparison group received a workbook after the follow-up evaluation. The independent t-test was performed to analyze changes in communicationskills, clinical performance, and emotional intelligence.Results: Communication skills (t=1.84, p=.035) and clinical performance (t=2.75, p=.004) significantly increased in the experimental group compared to the comparison group. A significant difference was not observed between the experimental and comparison groups for emotional intelligence(t=1.36, p=.088).Conclusion: The emotive role-play program concerning high-risk pregnancy was effective in improving nursing students’ communication skills and clinical performance and can be used in nursingeducation related to high-risk pregnancy and childbirth.
Figure
Reference
-
References
1. Pozzo ML, Brusati V, Cetin I. Clinical relationship and psychological experience of hospitalization in “high-risk” pregnancy. Eur J Obstet Gynecol Reprod Biol. 2010; 149(2):136–142. https://doi.org/10.1016/j.ejogrb.2009.12.009.
Article2. World Health Organization (WHO). Managing complications in pregnancy and childbirth: a guide for midwives and doctors. 2nd ed. Geneva: WHO;2017. p. 492.3. Ahn TG, Kim T, Kim Y, Hwang JY. The current state of maternity care and suggestions for improvement in the management of high-risk pregnancies in South Korea. J Korean Soc Matern Child Health. 2018; 22(3):134–141. https://doi.org/10.21896/jksmch.2018.22.3.134.
Article4. Gourounti C, Karpathiotaki N, Vaslamatzis G. Psychosocial stress in high risk pregnancy. Int Arch Med. 2015; 8(95):https://doi.org/10.3823/1694.
Article5. Ertekin Pinar S, Daglar G, Duran Aksoy O. The effect of stress management training on perceived stress, anxiety and hopelessness levels of women with high-risk pregnancy. J Obstet Gynaecol. 2022; 42(1):17–22. https://doi.org/10.1080/01443615.2020.1867970.
Article6. Henderson J, Redshaw M. Women’s experience of induction of labor: a mixed methods study. Acta Obstet Gynecol Scand. 2013; 92(10):1159–1167. https://doi.org/10.1111/aogs.12211.
Article7. König-Bachmann M, Schwarz C, Zenzmaier C. Women’s experiences and perceptions of induction of labour: Results from a German online-survey. Eur J Midwifery. 2017; 1(2):https://doi.org/10.18332/ejm/76511.
Article8. Toker E, Kömürcü N. Effect of Turkish classical music on prenatal anxiety and satisfaction: a randomized comparisonled trial in pregnant women with pre-eclampsia. Complement Ther Med. 2017; 30:1–9. https://doi.org/10.1016/j.ctim.2016.11.005.
Article9. Kim EM, Hong S. Impact of uncertainty on the anxiety of hospitalized pregnant women diagnosed with preterm labor: focusing on mediating effect of uncertainty appraisal and coping style. J Korean Acad Nurs. 2018; 48(4):485–496. https://doi.org/10.4040/jkan.2018.48.4.485.
Article10. Mirtabar SM, Faramarzi M, Khazaei R, Dini M. Efficacy of psychotherapy for anxiety reduction in hospital management of women successfully treated for preterm labor: a randomized comparisonled trial. Women Health. 2020; 60(10):1151–1163. https://doi.org/10.1080/03630242.2020.1803464.
Article11. Kim M, Nam H, Youn M. Infertility stress, depression, and resilience in women with infertility treatments. J Korean Acad Community Health Nurs. 2016; 30(1):93–104. https://doi.org/10.5932/JKPHN.2016.30.1.93.
Article12. Kim HJ, Chun N. Effects of a supportive program on uncertainty, anxiety, and maternal-fetal attachment in women with high-risk pregnancy. Korean J Women Health Nurs. 2020; 26(2):180–190. https://doi.org/10.4069/kjwhn.2020.06.17.
Article13. Mayer JD, Salovey P. What is emotional intelligence? In emotional development and emotional intelligence: implications for educators. New York: Basic Books;1997. p. 3–31.14. Lewis GM, Neville C, Ashkanasy NM. Emotional intelligence and affective events in nurse education: a narrative review. Nurse Educ Today. 2017; 53:34–40. https://doi.org/10.1016/j.nedt.2017.04.001.
Article15. Lee OS, Gu MO. Development and effects of emotional intelligence program for undergraduate nursing students: mixed methods research. J Korean Acad Nurs. 2014; 44(6):682–696. https://doi.org/10.4040/jkan.2014.44.6.682.
Article16. Rankin B. Emotional intelligence: enhancing values-based practice and compassionate care in nursing. J Adv Nurs. 2013; 69(12):2717–2725. https://doi.org/10.1111/jan.12161.
Article17. Hwang SK, Lee YJ. Interpersonal communication competence and social anxiety in nursing students. J Korean Acad Soc Nurs Educ. 2015; 21(4):518–527. https://doi.org/10.5977/jkasne.2015.21.4.518.
Article18. Xie J, Ding S, Wang C, Liu A. An evaluation of nursing students’ communication ability during practical clinical training. Nurse Educ Today. 2013; 33(8):823–827. https://doi.org/10.1016/j.nedt.2012.02.011.
Article19. Do ES, Seo YS. Factors influencing clinical competence in nursing students. J Korean Acad Fundam Nurs. 2014; 21(3):283–291. https://doi.org/10.7739/jkafn.2014.21.3.283.
Article20. Jang S, Kim S, Park N. Factors influencing metacognition, communication skills, and confidence in the performance of core basic nursing skills on clinical competency in nursing students. J Korean Acad Soc Nurs Educ. 2019; 25(4):448–458. https://doi.org/10.5977/jkasne.2019.25.4.448.
Article21. Trankle SA, Shanmugam S, Lewis E, Nicholson M, Hillman K, Cardona M. Are we making progress on communication with people who are near the end of life in the Australian health system? A thematic analysis. Health Commun. 2020; 35(2):158–167. https://doi.org/10.1080/10410236.2018.1548335.
Article22. Gelis A, Cervello S, Rey R, Llorca G, Lambert P, Franck N, et al. Peer role-play for training communication skills in medical students: a systematic review. Simul Healthc. 2020; 15(2):106–111. https://doi.org/10.1097/SIH.0000000000000412.
Article23. Seo DH, Jeong IJ. The effects of role playing on empathy and communication competence for nursing students in psychiatric mental health nursing practicum. J Korea Entertain Ind Assoc. 2019; 13(4):263–270. https://doi.org/10.21184/jkeia.2019.6.13.4.263.
Article24. Rotter B, Braband B. Confidence and competence in palliative care: a comparison of traditional and nontraditional transfer nursing students’ lived learning experiences. J Hosp Palliat Nurs. 2020; 22(3):196–203. https://doi.org/10.1097/NJH.0000000000000643.
Article25. Schlegel C, Woermann U, Shaha M, Rethans JJ, van der Vleuten C. Effects of communication training on real practice performance: a role-play module versus a standardized patient module. J Nurs Educ. 2012; 51(1):16–22. https://doi.org/10.3928/01484834-20111116-02.
Article26. Heidarzadeh H, Heidarzadeh Z, Azadi A. Comparison of pre-hospital triage training by role playing and lecture on nursing students’ knowledge, attitude and performance. Nurs Open. 2020; 7(4):935–942. https://doi.org/10.1002/nop2.464.
Article27. Ahmady S, Shahbazi S, Khajeali N. Comparing the effect of traditional and role-play training methods on nursing students’ performance and satisfaction in the principles of patient education course. J Educ Health Promot. 2021; 10:146. https://doi.org/10.4103/jehp.jehp_722_20.
Article28. Park E. Effects of family nursing practicum using role play on emotional intelligence, communication ability, and family nursing performance of nursing students. J Korean Acad Soc Nurs Educ. 2013; 19(4):656–662. https://doi.org/10.5977/jkasne.2013.19.4.656.
Article29. Noh YG, Lee I. Effect of stepwise communication education program using SBAR among nursing students: focusing on scenarios and nursing case-based role playing. J Korean Acad Soc Nurs Educ. 2018; 24(2):115–126. https://doi.org/10.5977/jkasne.2018.24.2.115.
Article30. Wheeler CA, McNelis AM. Nursing student perceptions of a community-based home visit experienced by a role-play simulation. Nurs Educ Perspect. 2014; 35(4):259–261. https://doi.org/10.5480/12-932.1.
Article31. Ulrich DL, Gillespie GL, Boesch MC, Bateman KM, Grubb PL. Reflective responses following a role-play simulation of nurse bullying. Nurs Educ Perspect. 2017; 38(4):203–205. https://doi.org/10.1097/01.NEP.0000000000000144.
Article32. Jung HJ. The development of compensated learning program using role-playing and measurement of learning outcomes on maternity nursing practical education for nursing students. J Korea Entertain Ind Assoc. 2015; 9(1):137–146. https://doi.org/10.21184/jkeia.2015.02.9.0.137.
Article33. Cho EA. Effects of nursing education using role play of delivery on communication ability and self-directed learning of nursing students. J Korea Entertain Ind Assoc. 2015; 9(4):351–360. https://doi.org/10.21184/jkeia.2015.12.9.4.351.
Article34. Des Jarlais DC, Lyles C, Crepaz N; Trend Group. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004; 94(3):361–366. https://doi.org/10.2105/ajph.94.3.361.
Article35. Shaftel FR, Shaftel GA. Role playing in the curriculum. 2nd ed. Hoboken (NJ): Prentice-Hall;1982. p. 362.36. Yoo MJ. A case study on the effect of communication training program on nurse’s communication ability, emotional intelligence (EQ), self-esteem and interpersonal ability. J Korea Acad-Ind Coop Soc. 2018; 19(6):280–290. https://doi.org/10.5762/KAIS.2018.19.6.280.
Article37. Yoon S. Study on clinical nurse’s performance and satisfaction of using communication skills by interpersonal caring technique [master’s thesis]. Seoul: Ewha Womans University;2005. 87.38. Yang JJ, Park MY. The relationship of clinical competency and self-directed learning in nursing students. J Korean Acad Soc Nurs Educ. 2004; 10(2):271–277.39. Lee WH, Kim CJ, Yoo JS, Hur HK, Kim KS, Lim SM. Development of a clinical competency measurement tool for student. Yeonsei Univ J Nurs. 1990; 13:17–29.40. Wong CS, Law KS. The effects of leader and follower emotional intelligence on performance and attitude: an exploratory study. In : Hooper A, editor. Leadership perspectives. London: Routledge;2017. p. 97–128.41. Jung HW. An empirical study on the effect of emotional intelligence on organizational effectiveness [dissertation]. Busan: Pusan National University;2007. 191.42. Bosse HM, Schultz JH, Nickel M, Lutz T, Möltner A, Jünger J, et al. The effect of using standardized patients or peer role play on ratings of undergraduate communication training: a randomized comparisonled trial. Patient Educ Couns. 2012; 87(3):300–306. https://doi.org/10.1016/j.pec.2011.10.007.
Article43. Seybert AL, Kane-Gill SL. Elective course in acute care using online learning and patient simulation. Am J Pharm Educ. 2011; 75(3):54. https://doi.org/10.5688/ajpe75354.
Article44. Ryoo EN, Ha EH, Cho JY. Comparison of learning effects using high-fidelity and multi-mode simulation: an application of emergency care for a patient with cardiac arrest. J Korean Acad Nurs. 2013; 43(2):185–193. https://doi.org/10.4040/jkan.2013.43.2.185.
Article45. Park SA, Kim HY. Development and effects of a labor nursing education program using a high-fidelity simulator for nursing students. Korean J Women Health Nurs. 2020; 26(3):240–249. https://doi.org/10.4069/kjwhn.2020.09.18.
Article46. Kim J, Heo N, Jeon HJ, Jung D. Effects of simulation education on the communication competence, academic self-efficacy, and attitude about the elderly for nursing students: a learning approach based on an elderly-with-cognition-disorder scenario. J Korean Acad Soc Nurs Educ. 2015; 21(1):54–64. https://doi.org/10.5977/jkasne.2015.21.1.54.
Article47. Lee SJ. The effects of simulation training with hybrid model for nursing students on nursing performance ability and self confidence. Korean J Adult Nurs. 2013; 25(1):170–182. https://doi.org/10.7475/kjan.2013.25.1.170.
Article48. Oh HS, Kim HY. The effects of interpersonal relationship training program based on emotional intelligence in nursing college students. J East-West Nurs Res. 2013; 19(1):15–22. https://doi.org/10.14370/jewnr.2013.19.1.015.
Article49. Kim MS. Influence of metacognition and emotional intelligence on self-leadership in nursing students. J Korean Acad Nurs Adm. 2019; 25(2):146–155. https://doi.org/10.11111/jkana.2019.25.2.146.
Article50. Shin ES, Lee S. The emotional intelligence, defense mechanism and interpersonal caring behavior by enneagram personality types in nursing students. J Korean Acad Soc Nurs Educ. 2016; 22(4):514–526. https://doi.org/10.5977/jkasne.2016.22.4.514.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of a nursing leadership program on self-leadership, interpersonal relationships, clinical performance, problem-solving abilities, and nursing professionalism among nursing students in South Korea: a quasi-experimental study
- Effects of a Rational Emotive Behavior Therapy Counseling Program on Self-efficacy and Adjustment to College Life for Nursing Freshmen
- The effects of team-based learning on nursing students’ learning performance with a focus on high-risk pregnancy in Korea: a quasi-experimental study
- Effects of a Well-dying Program on Nursing Students
- Development and evaluation of a pediatric nursing competency-building program for nursing students in South Korea: a quasi-experimental study