Acute Crit Care.
2022 Nov;37(4):561-570. 10.4266/acc.2022.00444.
Association between timing of intubation and mortality in patients with idiopathic pulmonary fibrosis
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 2Department of Critical Care Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2540144
- DOI: http://doi.org/10.4266/acc.2022.00444
Abstract
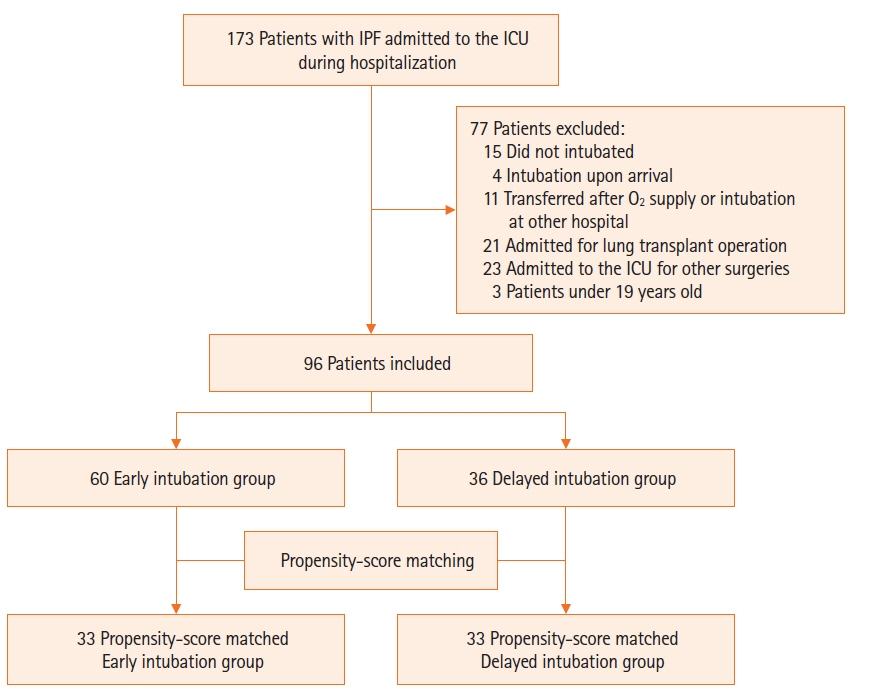
- Background
Delayed intubation is associated with poor prognosis in patients with respiratory failure. However, the effect of delayed intubation in patients with idiopathic pulmonary fibrosis (IPF) remains unknown. This study aimed to analyze whether timing of intubation after high-concentration oxygen therapy was associated with worse clinical outcomes in IPF patients. Methods: This retrospective propensity score-matched study enrolled adult patients with IPF who underwent mechanical ventilation between January 2011 and July 2021. Patients were divided into early and delayed intubation groups. Delayed intubation was defined as use of high-concentration oxygen therapy for at least 48 hours before tracheal intubation. The primary outcome was intensive care unit (ICU) mortality, and a conditional logistic regression model was used to evaluate the association between timing of intubation and clinical outcomes. Results: The median duration of high-concentration oxygen therapy before intubation was 0.5 days in the early intubation group (n=60) and 5.1 days in the delayed intubation group (n=36). The ICU mortality rate was 56.7% and 75% in the early and delayed intubation groups, respectively, before propensity matching (P=0.075). After matching for demographic and clinical covariates, 33 matched pairs were selected. In the propensity-matched cohort, delayed intubation significantly increased the risk of ICU mortality (adjusted odds ratio, 3.99; 95% confidence interval, 1.02–15.63; P=0.046). However, in-hospital mortality did not differ significantly between the groups. Conclusions: In patients with IPF, delayed intubation after initiation of high-concentration oxygen therapy was significantly associated with increased risk of ICU mortality compared to early intubation.
Keyword
Figure
Reference
-
1. Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011; 183:788–824.
Article2. Raghu G, Rochwerg B, Zhang Y, Garcia CA, Azuma A, Behr J, et al. An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis: an update of the 2011 clinical practice guideline. Am J Respir Crit Care Med. 2015; 192:e3–19.
Article3. Mollica C, Paone G, Conti V, Ceccarelli D, Schmid G, Mattia P, et al. Mechanical ventilation in patients with end-stage idiopathic pulmonary fibrosis. Respiration. 2010; 79:209–15.
Article4. Mallick S. Outcome of patients with idiopathic pulmonary fibrosis (IPF) ventilated in intensive care unit. Respir Med. 2008; 102:1355–9.
Article5. Weill D, Benden C, Corris PA, Dark JH, Davis RD, Keshavjee S, et al. A consensus document for the selection of lung transplant candidates: 2014: an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2015; 34:1–15.
Article6. Fernández Fabrellas E, Peris Sánchez R, Sabater Abad C, Juan Samper G. Prognosis and follow-up of idiopathic pulmonary fibrosis. Med Sci (Basel). 2018; 6:51.
Article7. Alqalyoobi S, Fernández Pérez ER, Oldham JM. In-hospital mortality trends among patients with idiopathic pulmonary fibrosis in the United States between 2013-2017: a comparison of academic and non-academic programs. BMC Pulm Med. 2020; 20:289.
Article8. Ni YN, Luo J, Yu H, Liu D, Ni Z, Cheng J, et al. Can high-flow nasal cannula reduce the rate of endotracheal intubation in adult patients with acute respiratory failure compared with conventional oxygen therapy and noninvasive positive pressure ventilation?: a systematic review and meta-analysis. Chest. 2017; 151:764–75.
Article9. Kang BJ, Koh Y, Lim CM, Huh JW, Baek S, Han M, et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med. 2015; 41:623–32.
Article10. Kangelaris KN, Ware LB, Wang CY, Janz DR, Zhuo H, Matthay MA, et al. Timing of intubation and clinical outcomes in adults with acute respiratory distress syndrome. Crit Care Med. 2016; 44:120–9.
Article11. Thomson CC, Duggal A, Bice T, Lederer DJ, Wilson KC, Raghu G. 2018 Clinical practice guideline summary for clinicians: diagnosis of idiopathic pulmonary fibrosis. Ann Am Thorac Soc. 2019; 16:285–90.12. Rengasamy S, Nassef B, Bilotta F, Pugliese F, Nozari A, Ortega R. Administration of supplemental oxygen. N Engl J Med. 2021; 385:e9.
Article13. Ley B, Ryerson CJ, Vittinghoff E, Ryu JH, Tomassetti S, Lee JS, et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med. 2012; 156:684–91.
Article14. Austin PC. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med. 2008; 27:2037–49.
Article15. D’Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998; 17:2265–81.
Article16. Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011; 10:150–61.
Article17. Bang H, Robins JM. Doubly robust estimation in missing data and causal inference models. Biometrics. 2005; 61:962–73.
Article18. Li X, Shen C. Doubly robust estimation of causal effect: upping the odds of getting the right answers. Circ Cardiovasc Qual Outcomes. 2020; 13:e006065.19. Leisman DE. Ten pearls and pitfalls of propensity scores in critical care research: a guide for clinicians and researchers. Crit Care Med. 2019; 47:176–85.20. Schrader M, Sathananthan M, Jeganathan N. Patients with idiopathic pulmonary fibrosis admitted to the ICU with acute respiratory failure: a reevaluation of the risk factors and outcomes. J Intensive Care Med. 2022; 37:342–51.
Article21. Kelly BT, Thao V, Dempsey TM, Sangaralingham LR, Payne SR, Teague TT, et al. Outcomes for hospitalized patients with idiopathic pulmonary fibrosis treated with antifibrotic medications. BMC Pulm Med. 2021; 21:239.
Article22. Blivet S, Philit F, Sab JM, Langevin B, Paret M, Guérin C, et al. Outcome of patients with idiopathic pulmonary fibrosis admitted to the ICU for respiratory failure. Chest. 2001; 120:209–12.
Article23. Lee HY, Lee J, Jung YS, Kwon WY, Oh DK, Park MH, et al. Preexisting clinical frailty is associated with worse clinical outcomes in patients with sepsis. Crit Care Med. 2022; 50:780–90.
Article24. Lee HY, Cho J, Kwak N, Lee J, Park YS, Lee CH, et al. Prognostic impact of malignant diseases in idiopathic pulmonary fibrosis. Sci Rep. 2020; 10:18260.
Article25. Bauer PR, Gajic O, Nanchal R, Kashyap R, Martin-Loeches I, Sakr Y, et al. Association between timing of intubation and outcome in critically ill patients: a secondary analysis of the ICON audit. J Crit Care. 2017; 42:1–5.
Article26. Park S. High-flow nasal cannula for respiratory failure in adult patients. Acute Crit Care. 2021; 36:275–85.
Article27. Ferreyro BL, Angriman F, Munshi L, Del Sorbo L, Ferguson ND, Rochwerg B, et al. Association of noninvasive oxygenation strategies with all-cause mortality in adults with acute hypoxemic respiratory failure: a systematic review and meta-analysis. JAMA. 2020; 324:57–67.
Article28. Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med. 2017; 195:438–42.
Article29. Brochard L. Ventilation-induced lung injury exists in spontaneously breathing patients with acute respiratory failure: yes. Intensive Care Med. 2017; 43:250–2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two cases of idiopathic pulmonary fibrosis
- Pharmacological treatment of idiopathic pulmonary fibrosis and fibrosing interstitial lung diseases: current trends and future directions
- A Case of Spontaneous Pneumomediastinum and Pneumopericardium in a Patient with Acute Exacerbation of Idiopathic Pulmonary Fibrosis
- Idiopathic Pulmonary Fibrosis and Nonspecific Interstitial Pneumonia
- Pharmacological treatment of pulmonary fibrosis