Arch Hand Microsurg.
2023 Mar;28(1):33-38. 10.12790/ahm.22.0060.
High-resolution ultrasonography is a more useful primary diagnostic tool than magnetic resonance imaging for subungual glomus tumors: a single-center retrospective study
- Affiliations
-
- 1Department of Orthopaedic Surgery, Wonju Yonsei Hospital, Wonju, Korea
- 2Department of Orthopaedic Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- KMID: 2540028
- DOI: http://doi.org/10.12790/ahm.22.0060
Abstract
- Purpose
Ultrasonography (US) and magnetic resonance imaging (MRI), which has better resolution, have been suggested as appropriate diagnostic tools for digits; however, comparative studies of both modalities are scarce. This study compared the diagnostic performance of high-resolution US and MRI in characterizing subungual glomus tumors.
Methods
We retrospectively analyzed the data of consecutive patients who were examined with high-resolution US and MRI before surgical exploration for subungual tumors from January 2017 to April 2020. The patients’ clinical data and radiological findings were collected. Historical reports for diagnostic confirmation and measurements of mass size were reviewed. We conducted the McNemar test and evaluated the degree of agreement between the size measurements made using both techniques.
Results
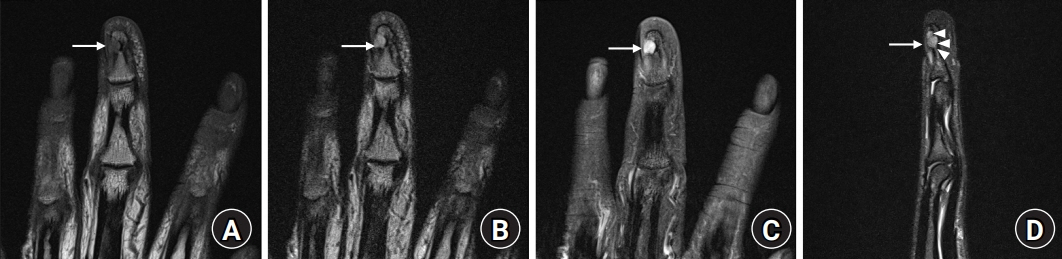
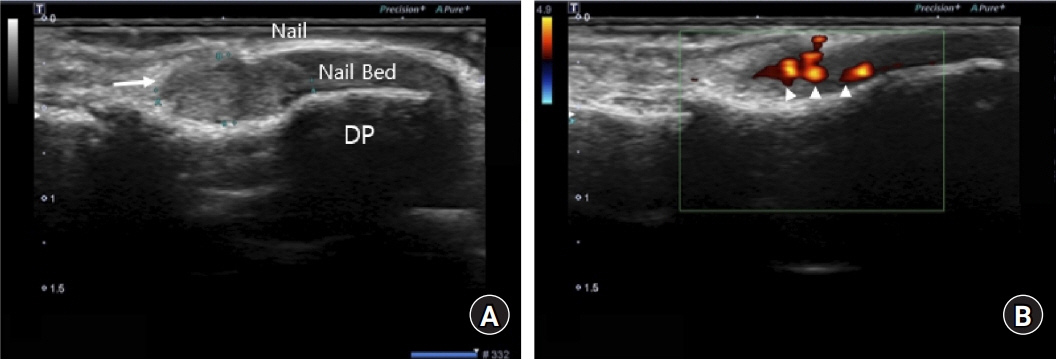
Overall, 22 patients (age range, 19–72 years) underwent surgical exploration and had subungual glomus tumors. The mean duration from initial symptom presentation to diagnosis was 7 years (range, 5–30) years. Only nine patients (40.9%) presented with the symptomatic triad of pain, cold sensitivity, and tenderness. MRI detected lesions in 19 cases (86.4%); three cases (13.6%) were undetected. Contrastingly, US was able to detect all lesions. Nine patients (40.9%) had visibly rich blood flow in tumor tissues on Doppler US. MRI and US showed bone erosion in eight and 15 cases, respectively.
Conclusion
The detection rate of high-resolution US for subungual glomus tumors was as high as that of MRI. US can be applied easily and quickly and can be more useful as a primary diagnostic tool.
Figure
Reference
-
References
1. McDermott EM, Weiss AP. Glomus tumors. J Hand Surg Am. 2006; 31:1397–400.2. Tang CY, Tipoe T, Fung B. Where is the lesion?: glomus tumours of the hand. Arch Plast Surg. 2013; 40:492–5.3. Kim DH. Glomus tumor of the finger tip and MRI appearance. Iowa Orthop J. 1999; 19:136–8.4. Dahlin LB, Besjakov J, Veress B. A glomus tumour: classic signs without magnetic resonance imaging findings. Scand J Plast Reconstr Surg Hand Surg. 2005; 39:123–5.5. Carroll RE, Berman AT. Glomus tumors of the hand: review of the literature and report on twenty-eight cases. J Bone Joint Surg Am. 1972; 54:691–703.6. Jawalkar H, Maryada VR, Brahmajoshyula V, Kotha GK. Subungual glomus tumors of the hand: treated by transungual excision. Indian J Orthop. 2015; 49:403–7.7. Hung EH, Griffith JF, Yip SW, et al. Accuracy of ultrasound in the characterization of superficial soft tissue tumors: a prospective study. Skeletal Radiol. 2020; 49:883–92.8. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–74.9. Zha G, Niu X, Liu Y, Xiao L, Hu J, Yi J. The application of MRI in preoperative localization of glomus tumors of the fingertip. Int J Clin Exp Pathol. 2016; 9:12627–31.10. Wortsman X, Jemec GB. Role of high-variable frequency ultrasound in preoperative diagnosis of glomus tumors: a pilot study. Am J Clin Dermatol. 2009; 10:23–7.11. González-Llanos F, López-Barea F, Isla A, Fernández-Prieto A, Zubillaga A, Alvarez F. Periosteal glomus tumor of the femur: a case report. Clin Orthop Relat Res. 2000; (380):199–203.12. Matloub HS, Muoneke VN, Prevel CD, Sanger JR, Yousif NJ. Glomus tumor imaging: use of MRI for localization of occult lesions. J Hand Surg Am. 1992; 17:472–5.13. Pandey CR, Singh N, Tamang B. Subungual glomus tumours: is magnetic resonance imaging or ultrasound necessary for diagnosis? Malays Orthop J. 2017; 11:47–51.14. Al-Qattan MM, Al-Namla A, Al-Thunayan A, Al-Subhi F, El-Shayeb AF. Magnetic resonance imaging in the diagnosis of glomus tumours of the hand. J Hand Surg Br. 2005; 30:535–40.15. Drapé JL, Idy-Peretti I, Goettmann S, et al. Subungual glomus tumors: evaluation with MR imaging. Radiology. 1995; 195:507–15.16. Laidlaw A, Henwood S. Patients with multiple sclerosis: their experiences and perceptions of the MRI investigation. J Diagn Radiogr Imaging. 2003; 5:19–25.17. Törnqvist E, Månsson A, Larsson EM, Hallström I. It’s like being in another world: patients’ lived experience of magnetic resonance imaging. J Clin Nurs. 2006; 15:954–61.18. Munn Z, Jordan Z. The patient experience of high technology medical imaging: a systematic review of the qualitative evidence. Radiography. 2011; 17:323–31.19. Wang PJ, Zhang Y, Zhao JJ. Treatment of subungual glomus tumors using the nail bed margin approach. Dermatol Surg. 2013; 39:1689–94.20. Matsunaga A, Ochiai T, Abe I, et al. Subungual glomus tumour: evaluation of ultrasound imaging in preoperative assessment. Eur J Dermatol. 2007; 17:67–9.21. Chen SH, Chen YL, Cheng MH, Yeow KM, Chen HC, Wei FC. The use of ultrasonography in preoperative localization of digital glomus tumors. Plast Reconstr Surg. 2003; 112:115–20.22. Fan Z, Wu G, Ji B, et al. Color Doppler ultrasound morphology of glomus tumors of the extremities. Springerplus. 2016; 5:1319.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Subungual Epidermal Cyst
- Glomus Tumors: Symptom Variations and Magnetic Resonance Imaging for Diagnosis
- An Unusual Cause of Knee Pain: Periosteal Glomus Tumor of the Distal Femur
- Ultrasonographic Findings of Subungual Glomus Tumors: An Analysis of 20 Cases
- Distribution of Glomus Tumors in Fingers