Clin Exp Otorhinolaryngol.
2023 Feb;16(1):20-27. 10.21053/ceo.2022.01039.
Improved Bone Conduction Hearing After Middle Ear Surgery: Investigation of the Improvement Mechanism
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Konyang University College of Medicine, Daejeon, Korea
- 2Department of Medical Sciences, Ajou University Graduate School of Medicine, Suwon, Korea
- 3Department of Otolaryngology, Ajou University School of Medicine, Suwon, Korea
- KMID: 2539765
- DOI: http://doi.org/10.21053/ceo.2022.01039
Abstract
Objectives
. When performing middle ear operations, such as ossiculoplasty or stapes surgery, patients and surgeons expect an improvement in air conduction (AC) hearing, but generally not in bone conduction (BC). However, BC improvement has often been observed after surgery, and the present study investigated this phenomenon.
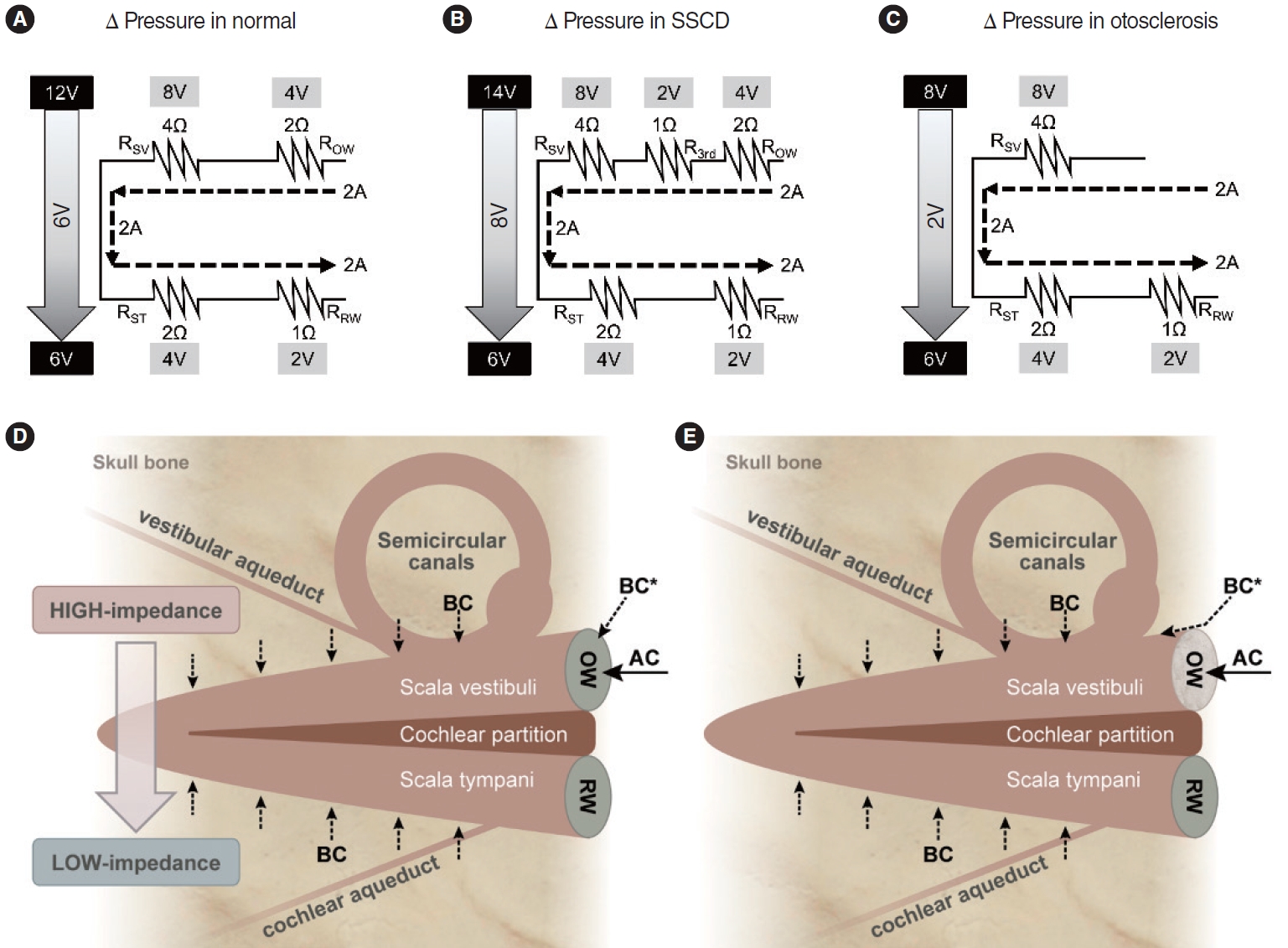
Methods
. We reviewed the preoperative and postoperative surgical outcomes of 583 patients who underwent middle ear surgery. BC improvement was defined as a BC threshold decrease of >15 dB at two or more frequencies. Subjects in group A underwent staged ossiculoplasty after canal wall up mastoidectomy (CWUM), group B underwent staged ossiculoplasty after canal wall down mastoidectomy (CWDM), group C underwent ossiculoplasty only (thus, they had no prior history of CWUM or CWDM), and group D received stapes surgery. We created a hypothetical circuit model to explain this phenomenon.
Results
. BC improvement was detected in 12.8% of group A, 9.1% of group B, and 8.5% of group C. The improvement was more pronounced in group D (27.0%). A larger gain in AC hearing was weakly correlated with greater BC improvement (Pearson’s r=0.395 in group A, P<0.001; r=0.375 in group B, P<0.001; r=0.296 in group C, P<0.001; r=0.422 in group D, P=0.009). Notably, patients with otosclerosis even experienced postoperative BC improvements as large as 10.0 dB, from a mean value of 30.3 dB (standard error [SE], 3.2) preoperatively to 20.3 dB (SE, 3.2) postoperatively, at 1,000 Hz, as well as an improvement of 9.2 dB at 2,000 Hz, from 37.8 dB (SE, 2.6) to 28.6 dB (SE, 3.1).
Conclusion
. BC improvement may be explained by a hypothetical circuit model applying the third window theory. Surgeons should keep in mind the possibility of BC improvement when making a management plan.
Keyword
Figure
Reference
-
1. Kileny PR, Zwolan TA, Slagar HK. Diagnostic audiology and electrophysiologic assessment of hearing. In : Flint PW, Francis HW, Haughey BH, Lesperance MM, Lund VJ, Robbins KT, editors. Cummings otolaryngology: head and neck surgery. 7th ed. Elsevier;2021. p. 2021–41.2. Richter U, Brinkmann K. Threshold of hearing by bone conduction: a contribution to international standardization. Scand Audiol. 1981; 10(4):235–7.3. Stenfelt S, Goode RL. Bone-conducted sound: physiological and clinical aspects. Otol Neurotol. 2005; Nov. 26(6):1245–61.
Article4. Khanna SM, Tonndorf J, Queller JE. Mechanical parameters of hearing by bone conduction. J Acoust Soc Am. 1976; Jul. 60(1):139–54.
Article5. Stenfelt S. Simultaneous cancellation of air and bone conduction tones at two frequencies: extension of the famous experiment by von Bekesy. Hear Res. 2007; Mar. 225(1-2):105–16.6. Stenfelt S, Puria S, Hato N, Goode RL. Basilar membrane and osseous spiral lamina motion in human cadavers with air and bone conduction stimuli. Hear Res. 2003; Jul. 181(1-2):131–43.
Article7. Mauldin L, Jerger J. Auditory brain stem evoked responses to boneconducted signals. Arch Otolaryngol. 1979; Nov. 105(11):656–61.
Article8. Purcell D, Kunov H, Madsen P, Cleghorn W. Distortion product otoacoustic emissions stimulated through bone conduction. Ear Hear. 1998; Oct. 19(5):362–70.
Article9. Kobayashi T, Sakurai T, Okitsu T, Yuasa R, Kawase T, Kusakari J, et al. Labyrinthine fistulae caused by cholesteatoma: improved bone conduction by treatment. Am J Otol. 1989; Jan. 10(1):5–10.10. Vijayendra H, Parikh B. Bone conduction improvement after surgery for conductive hearing loss. Indian J Otolaryngol Head Neck Surg. 2011; Jul. 63(3):201–4.
Article11. Kitahara T, Kamakura T, Ohta Y, Morihana T, Horii A, Uno A, et al. Chronic otitis media with cholesteatoma with canal fistula and bone conduction threshold after tympanoplasty with mastoidectomy. Otol Neurotol. 2014; Jul. 35(6):981–8.
Article12. Lee HS, Hong SD, Hong SH, Cho YS, Chung WH. Ossicular chain reconstruction improves bone conduction threshold in chronic otitis media. J Laryngol Otol. 2008; Apr. 122(4):351–6.
Article13. Milner RM, Weller CR, Brenman AK. Elevated bone conduction thresholds associated with middle ear fluid in adults. Int J Pediatr Otorhinolaryngol. 1983; Nov. 6(2):163–9.
Article14. Tuz M, Dogru H, Uygur K, Gedikli O. Improvement in bone conduction threshold after tympanoplasty. Otolaryngol Head Neck Surg. 2000; Dec. 123(6):775–8.
Article15. Kobayashi K, Kodama H, Takezawa H, Suzuki T, Kataura A. Elevation of bone conduction threshold in children with middle ear effusion. Int J Pediatr Otorhinolaryngol. 1988; Nov. 16(2):95–100.
Article16. Prodanovic S, Stenfelt S. Consequences of mastoidectomy on bone conducted sound based on simulations in a whole human head. Otol Neurotol. 2020; Oct. 41(9):e1158–66.
Article17. Stenfelt S. Acoustic and physiologic aspects of bone conduction hearing. Adv Otorhinolaryngol. 2011; 71:10–21.
Article18. Homma K, Du Y, Shimizu Y, Puria S. Ossicular resonance modes of the human middle ear for bone and air conduction. J Acoust Soc Am. 2009; Feb. 125(2):968–79.
Article19. Iversen MM, Rabbitt RD. Biomechanics of third window syndrome. Front Neurol. 2020; Aug. 11:891.
Article20. Merchant SN, Rosowski JJ. Conductive hearing loss caused by thirdwindow lesions of the inner ear. Otol Neurotol. 2008; Apr. 29(3):282–9.
Article21. Ho ML, Moonis G, Halpin CF, Curtin HD. Spectrum of third window abnormalities: semicircular canal dehiscence and beyond. AJNR Am J Neuroradiol. 2017; Jan. 38(1):2–9.
Article22. Bae YJ, Shim YJ, Choi BS, Kim JH, Koo JW, Song JJ. “Third window” and “single window” effects impede surgical success: analysis of retrofenestral otosclerosis involving the internal auditory canal or round window. J Clin Med. 2019; Aug. 8(8):1182.
Article23. Rosowski JJ, Songer JE, Nakajima HH, Brinsko KM, Merchant SN. Clinical, experimental, and theoretical investigations of the effect of superior semicircular canal dehiscence on hearing mechanisms. Otol Neurotol. 2004; May. 25(3):323–32.
Article24. Lee SY, Bae YJ, Kim M, Song JJ, Choi BY, Koo JW. Changes in vestibulo-ocular reflex gain after surgical plugging of superior semicircular canal dehiscence. Front Neurol. 2020; Jul. 11:694.
Article25. Minor LB. Clinical manifestations of superior semicircular canal dehiscence. Laryngoscope. 2005; Oct. 115(10):1717–27.
Article26. Chole RA, McKenna M. Pathophysiology of otosclerosis. Otol Neurotol. 2001; Mar. 22(2):249–57.
Article27. Quesnel AM, Ishai R, McKenna MJ. Otosclerosis: temporal bone pathology. Otolaryngol Clin North Am. 2018; Apr. 51(2):291–303.28. Tonndorf J, Khanna S, Fingerhood BJ. The input impedance of the inner ear in cats. Ann Otol Rhinol Laryngol. 1966; Sep. 75(3):752–63.29. Ohm GS. Die galvanische Kette, mathematisch bearbeitet. 1st ed. T.H. Riemann;1827.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Stapedectomy with Total Ossicular Replacement Prosthesis in Stapes Fixation without Malleus and Incus
- Effects of middle ear and temporal bone pathology on bone conduction hearing level in chronic otitis media
- Experience of BAHA(Bone Anchored Hearing Aid) Surgery
- Frequency-Specific Hearing Results After Surgery for Chronic Ear Diseases
- Management of Congenital Aural Atresia and Microtia