Ann Rehabil Med.
2023 Feb;47(1):45-51. 10.5535/arm.22149.
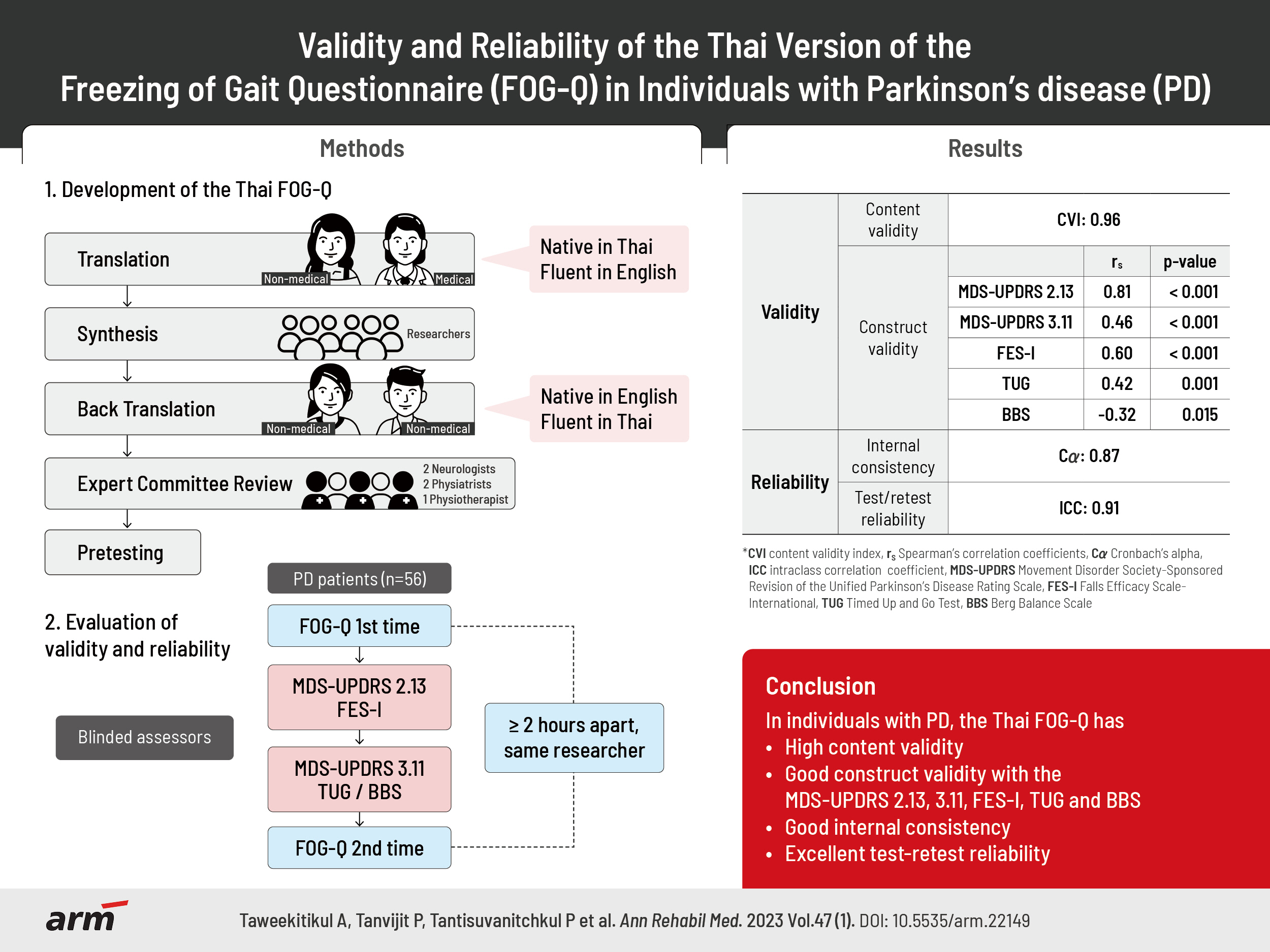
Validity and Reliability of the Thai Version of the Freezing of Gait Questionnaire in Individuals With Parkinson’s disease
- Affiliations
-
- 1Department of Rehabilitation Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
- 2Department of Rehabilitation Medicine, Maharaj Nakhon Si Thammarat Hospital, Nakhon Si Thammarat, Thailand
- 3Rehabilitation Center, Vejthani Hospital, Bangkok, Thailand
- 4Department of Medicine, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
- 5Facultyof Physical Therapy, Mahidol University, Nakhon Pathom, Thailand
- KMID: 2539727
- DOI: http://doi.org/10.5535/arm.22149
Abstract
Objective
To evaluate the validity and reliability of the Thai version of the Freezing of Gait Questionnaire (FOG-Q) in individuals with Parkinson’s disease (PD).
Methods
The FOG-Q was translated into Thai according to the standard process. Fifty-six individuals with PD participated in the study. The content validity was assessed using the content validity index (CVI). The construct validity was evaluated by correlating Thai FOG-Q with Thai version of the Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) items 2.13 and 3.11, Thai version of the Falls Efficacy Scale-International (FES-I), Timed Up and Go test (TUG) and Berg Balance Scale (BBS) using Spearman’s correlation coefficient (rS). The correlation between Thai FOG-Q and clinical characteristics, for example, duration of PD and modified Hoehn and Yahr (mH&Y) stage was evaluated. Internal consistency and test-retest reliability were evaluated with Cronbach’s alpha (Cα) and intraclass correlation coefficient (ICC), respectively.
Results
The Thai FOG-Q had high content validity (CVI=0.96). The mean FOG-Q score was 9.0±4.9. The construct validity showed a strong positive correlation with MDS-UPDRS item 2.13 (rS=0.81), and moderate correlations with MDS-UPDRS item 3.11, FES-I, and TUG (rS=0.42–0.60). A negative correlation with BBS was found (rS=-0.32). It had a moderate correlation with mH&Y stage (rS=0.40). The Thai FOG-Q had good internal consistency (Cα=0.87) with excellent test-retest reliability (ICC=0.91).
Conclusion
The Thai FOG-Q has excellent validity and reliability. It is a useful instrument for the evaluation of FOG in individuals with PD.
Figure
Reference
-
1. Nutt JG, Bloem BR, Giladi N, Hallett M, Horak FB, Nieuwboer A. Freezing of gait: moving forward on a mysterious clinical phenomenon. Lancet Neurol. 2011; 10:734–44.2. Tan DM, McGinley JL, Danoudis ME, Iansek R, Morris ME. Freezing of gait and activity limitations in people with Parkinson’s disease. Arch Phys Med Rehabil. 2011; 92:1159–65.3. Forsaa EB, Larsen JP, Wentzel-Larsen T, Alves G. A 12-year population-based study of freezing of gait in Parkinson’s disease. Parkinsonism Relat Disord. 2015; 21:254–8.4. Giladi N, Treves TA, Simon ES, Shabtai H, Orlov Y, Kandinov B, et al. Freezing of gait in patients with advanced Parkinson’s disease. J Neural Transm (Vienna). 2001; 108:53–61.5. Giladi N, McMahon D, Przedborski S, Flaster E, Guillory S, Kostic V, et al. Motor blocks in Parkinson’s disease. Neurology. 1992; 42:333–9.6. Bloem BR, Hausdorff JM, Visser JE, Giladi N. Falls and freezing of gait in Parkinson’s disease: a review of two interconnected, episodic phenomena. Mov Disord. 2004; 19:871–84.7. Lamberti P, Armenise S, Castaldo V, de Mari M, Iliceto G, Tronci P, et al. Freezing gait in Parkinson’s disease. Eur Neurol. 1997; 38:297–301.8. Georgy E. Freezing of gait in Parkinson’s disease: impact on falls risk, walking aids utilization, and assistance-seeking behavior. Eur J Adapt Phys Act. 2010; 3:49–59.9. Giladi N, McDermott MP, Fahn S, Przedborski S, Jankovic J, Stern M, et al. Freezing of gait in PD: prospective assessment in the DATATOP cohort. Neurology. 2001; 56:1712–21.10. Moore O, Peretz C, Giladi N. Freezing of gait affects quality of life of peoples with Parkinson’s disease beyond its relationships with mobility and gait. Mov Disord. 2007; 22:2192–5.11. Santos García D, de Deus Fonticoba T, Suárez Castro E, Borrué C, Mata M, Solano Vila B, et al. Non-motor symptoms burden, mood, and gait problems are the most significant factors contributing to a poor quality of life in non-demented Parkinson’s disease patients: results from the COPPADIS Study Cohort. Parkinsonism Relat Disord. 2019; 66:151–7.12. Giladi N, Shabtai H, Simon ES, Biran S, Tal J, Korczyn AD. Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat Disord. 2000; 6:165–70.13. Bloem BR, Marinus J, Almeida Q, Dibble L, Nieuwboer A, Post B, et al. Measurement instruments to assess posture, gait, and balance in Parkinson’s disease: critique and recommendations. Mov Disord. 2016; 31:1342–55.14. Giladi N, Tal J, Azulay T, Rascol O, Brooks DJ, Melamed E, et al. Validation of the freezing of gait questionnaire in patients with Parkinson’s disease. Mov Disord. 2009; 24:655–61.15. Nilsson MH, Hagell P. Freezing of Gait Questionnaire: validity and reliability of the Swedish version. Acta Neurol Scand. 2009; 120:331–4.16. Baggio JA, Curtarelli MB, Rodrigues GR, Tumas V. Validity of the Brazilian version of the freezing of gait questionnaire. Arq Neuropsiquiatr. 2012; 70:599–603.17. Vogler A, Janssens J, Nyffeler T, Bohlhalter S, Vanbellingen T. German translation and validation of the “freezing of gait questionnaire” in patients with Parkinson’s disease. Parkinsons Dis. 2015; 2015:982058.18. Tambasco N, Simoni S, Eusebi P, Ripandelli F, Brahimi E, Sacchini E, et al. The validation of an Italian version of the Freezing of Gait Questionnaire. Neurol Sci. 2015; 36:759–64.19. Candan SA, Çatıker A, Özcan TŞ. Psychometric properties of the Turkish version of the freezing of gait questionnaire for patients with Parkinson’s disease. Neurol Sci Neurophysiol. 2019; 36:44–50.20. Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008; 23:2129–70.21. Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing. 2005; 34:614–9.22. Jonasson SB, Nilsson MH, Lexell J. Psychometric properties of four fear of falling rating scales in people with Parkinson’s disease. BMC Geriatr. 2014; 14:66.23. Winser SJ, Kannan P, Bello UM, Whitney SL. Measures of balance and falls risk prediction in people with Parkinson’s disease: a systematic review of psychometric properties. Clin Rehabil. 2019; 33:1949–62.24. Thiamwong L. Psychometric testing of the Falls Efficacy Scale-International (FES-I) in Thai older adults. Songkla Med J. 2011; 29:277–87.25. Morris S, Morris ME, Iansek R. Reliability of measurements obtained with the Timed “Up & Go” test in people with Parkinson disease. Phys Ther. 2001; 81:810–8.26. Krzysztoń K, Stolarski J, Kochanowski J. Evaluation of balance disorders in Parkinson’s disease using simple diagnostic tests-not so simple to choose. Front Neurol. 2018; 9:932.27. Brusse KJ, Zimdars S, Zalewski KR, Steffen TM. Testing functional performance in people with Parkinson disease. Phys Ther. 2005; 85:134–41.28. Qutubuddin AA, Pegg PO, Cifu DX, Brown R, McNamee S, Carne W. Validating the Berg Balance Scale for patients with Parkinson’s disease: a key to rehabilitation evaluation. Arch Phys Med Rehabil. 2005; 86:789–92.29. Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000; 25:3186–91.30. Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018; 126:1763–8.31. Taber KS. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018; 48:1273–96.32. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016;15:155-63. Erratum in: J Chiropr Med. 2017; 16:346.33. Elbers RG, van Wegen EE, Verhoef J, Kwakkel G. Is gait speed a valid measure to predict community ambulation in patients with Parkinson’s disease? J Rehabil Med. 2013; 45:370–5.34. Adkin AL, Frank JS, Jog MS. Fear of falling and postural control in Parkinson’s disease. Mov Disord. 2003; 18:496–502.35. Park JH, Kang YJ, Horak FB. What is wrong with balance in Parkinson’s disease? J Mov Disord. 2015; 8:109–14.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Validation of the Thai Version of the Movement Disorder Society-Sponsored Revision of the Unified Parkinson's Disease Rating Scale
- The Validity and Reliability of a Screening Questionnaire for Parkinson's Disease in a Community
- Evaluating the Dimensionality and Reliability of the Thai Self-Care of Hypertension Inventory Version 2.0
- Deep Brain Stimulation of the Subthalamic and Pedunculopontine Nucleus in a Patient with Parkinson's Disease
- High Frequency Repetitive Transcranial Magnetic Stimulation for Freezing of Gait and Nonmotor Symptoms in Parkinson's Disease