Ann Hepatobiliary Pancreat Surg.
2023 Feb;27(1):40-48. 10.14701/ahbps.22-043.
Simultaneous resection of synchronous colorectal liver metastasis: Feasibility and development of a prediction model
- Affiliations
-
- 1Division of Gastrointestinal and Hepatopancreaticobiliary Surgery, Department of Surgical Oncology, Tata Memorial Hospital, Mumbai, India
- 2Homi Bhabha National Institute, Mumbai, India
- KMID: 2539512
- DOI: http://doi.org/10.14701/ahbps.22-043
Abstract
- Backgrounds/Aims
Timing of resection for synchronous colorectal liver metastasis (CRLM) has been debated for decades. The aim of the present study was to assess the feasibility of simultaneous resection of CRLM in terms of major complications and develop a prediction model for safe resections.
Methods
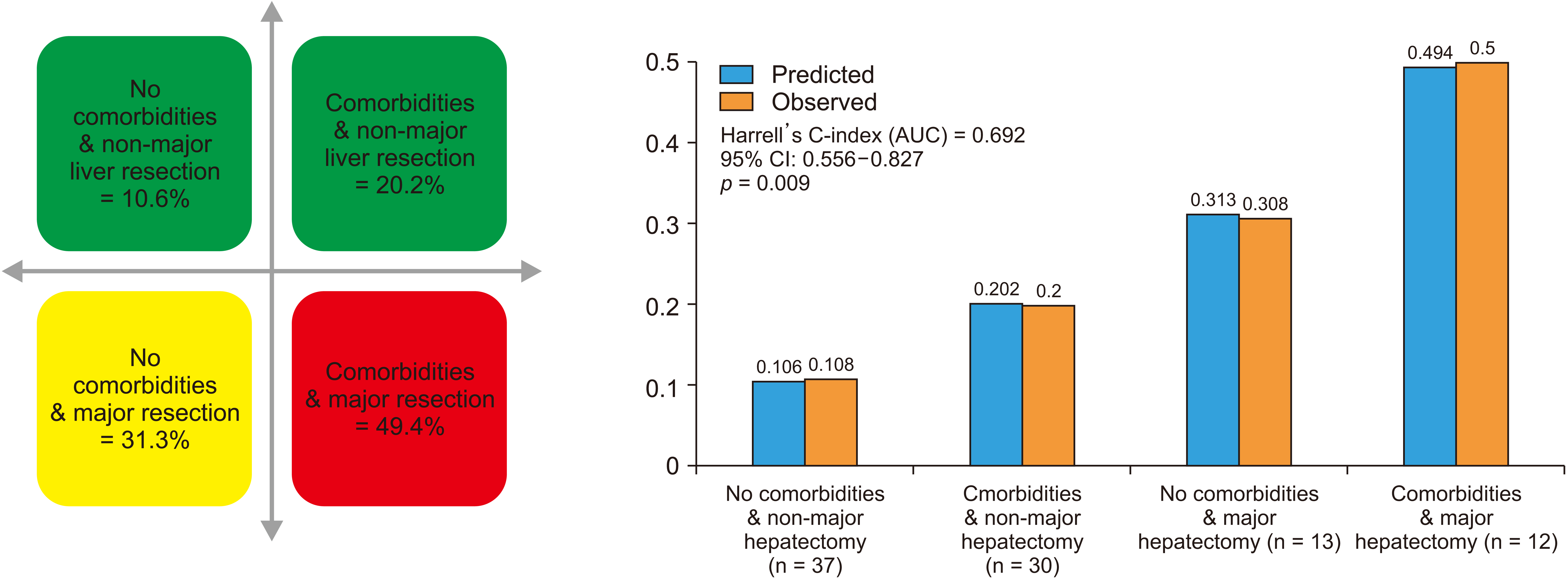
A retrospective single-center study of synchronous, resectable CRLM, operated between 2013 and 2021 was conducted. Upper limit of 95% confidence interval (CI) of major complications (≥ grade IIIA) was set at 40% as the safety threshold. Logistic regression was used to determine predictors of morbidity. Prediction model was internally validated by bootstrap estimates, Harrell’s C-index, and correlation of predicted and observed estimates.
Results
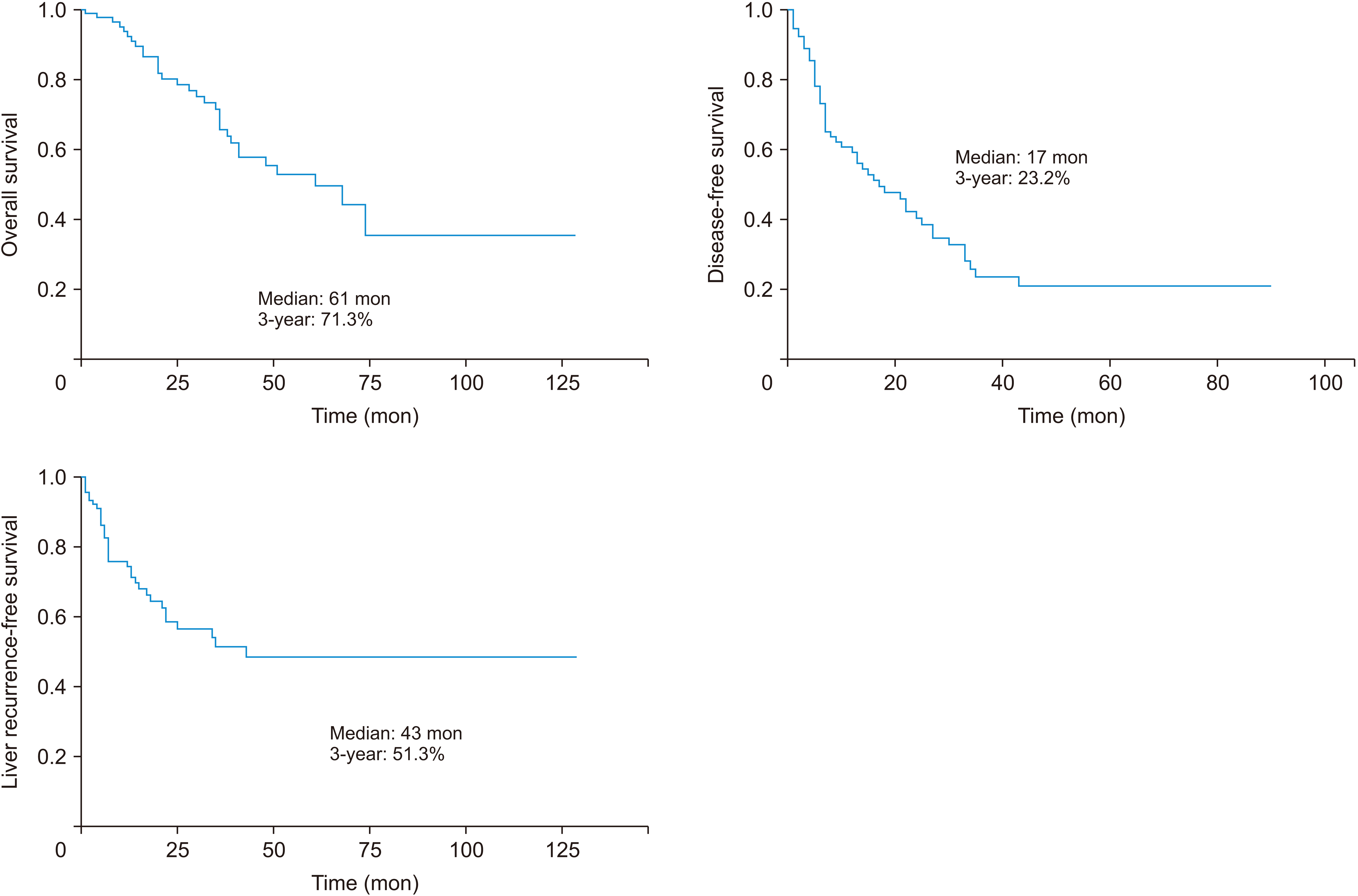
Ninety-two patients were operated. Of them, 41.3% had rectal cancers. Major hepatectomy (≥ 4 segments) was performed for 25 patients (27.2%). Major complications occurred in 20 patients (21.7%, 95% CI: 13.8%–31.5%). Predictors of complications were the presence of comorbidities and major hepatectomy (area under the ROC curve: 0.692). Unacceptable level of morbidity (≥ 40%) was encountered in patients with comorbidities who underwent major hepatectomy.
Conclusions
Simultaneous bowel and CRLM resection appear to be safe. However, caution should be exercised when combining major liver resections with bowel resection in patients with comorbid conditions.
Figure
Reference
-
1. Engstrand J, Nilsson H, Strömberg C, Jonas E, Freedman J. 2018; Colorectal cancer liver metastases - a population-based study on incidence, management and survival. BMC Cancer. 18:78. DOI: 10.1186/s12885-017-3925-x. PMID: 29334918. PMCID: PMC5769309.
Article2. Patil PS, Saklani A, Gambhire P, Mehta S, Engineer R, De'Souza A, et al. 2017; Colorectal cancer in India: an audit from a tertiary center in a low prevalence area. Indian J Surg Oncol. 8:484–490. DOI: 10.1007/s13193-017-0655-0. PMID: 29203978. PMCID: PMC5705504.
Article3. Baltatzis M, Chan AK, Jegatheeswaran S, Mason JM, Siriwardena AK. 2016; Colorectal cancer with synchronous hepatic metastases: systematic review of reports comparing synchronous surgery with sequential bowel-first or liver-first approaches. Eur J Surg Oncol. 42:159–165. DOI: 10.1016/j.ejso.2015.11.002. PMID: 26733368.
Article4. Bogach J, Wang J, Griffiths C, Parpia S, Saskin R, Hallet J, et al. 2020; Simultaneous versus staged resection for synchronous colorectal liver metastases: a population-based cohort study. Int J Surg. 74:68–75. DOI: 10.1016/j.ijsu.2019.12.009. PMID: 31843676.
Article5. Snyder RA, Hao S, Irish W, Zervos EE, Tuttle-Newhall JE, Parikh AA. 2020; Thirty-day morbidity after simultaneous resection of colorectal cancer and colorectal liver metastasis: American College of Surgeons NSQIP analysis. J Am Coll Surg. 230:617–627.e9. DOI: 10.1016/j.jamcollsurg.2019.12.018. PMID: 32007534.
Article6. Tsilimigras DI, Sahara K, Hyer JM, Diaz A, Moris D, Bagante F, et al. 2021; Trends and outcomes of simultaneous versus staged resection of synchronous colorectal cancer and colorectal liver metastases. Surgery. 170:160–166. DOI: 10.1016/j.surg.2021.01.041. PMID: 33674128.
Article7. Boudjema K, Locher C, Sabbagh C, Ortega-Deballon P, Heyd B, Bachellier P, et al. 2021; Simultaneous versus delayed resection for initially resectable synchronous colorectal cancer liver metastases: a prospective, open-label, randomized, controlled trial. Ann Surg. 273:49–56. DOI: 10.1097/SLA.0000000000003848. PMID: 32209911.
Article8. Serrano PE, Parpia S, Karanicolas P, Gallinger S, Wei AC, Simunovic M, et al. 2022; Simultaneous resection for synchronous colorectal cancer liver metastases: a feasibility clinical trial. J Surg Oncol. 125:671–677. DOI: 10.1002/jso.26764. PMID: 34878649.
Article9. Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. 1999; Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 230:309–318. discussion 318–321. DOI: 10.1097/00000658-199909000-00004. PMID: 10493478. PMCID: PMC1420876.
Article10. Dindo D, Demartines N, Clavien PA. 2004; Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 240:205–213. DOI: 10.1097/01.sla.0000133083.54934.ae. PMID: 15273542. PMCID: PMC1360123.11. Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, et al. 2011; Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 149:680–688. DOI: 10.1016/j.surg.2010.12.002. PMID: 21316725.
Article12. Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. 2011; Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 149:713–724. DOI: 10.1016/j.surg.2010.10.001. PMID: 21236455.
Article13. Rahbari NN, Garden OJ, Padbury R, Maddern G, Koch M, Hugh TJ, et al. 2011; Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford). 13:528–535. DOI: 10.1111/j.1477-2574.2011.00319.x. PMID: 21762295. PMCID: PMC3163274.
Article14. Joshi R, Thomas MJ, Bansode R, Mitra A, Chaudhari V, Desouza A, et al. 2016; Hepatic resections and enhanced recovery pathway: an Indian encounter. Clin Nutr ESPEN. 12:E54. DOI: 10.1016/j.clnesp.2016.02.078.
Article15. Smith GC, Seaman SR, Wood AM, Royston P, White IR. 2014; Correcting for optimistic prediction in small data sets. Am J Epidemiol. 180:318–324. DOI: 10.1093/aje/kwu140. PMID: 24966219. PMCID: PMC4108045.
Article16. Shubert CR, Habermann EB, Bergquist JR, Thiels CA, Thomsen KM, Kremers WK, et al. 2015; A NSQIP review of major morbidity and mortality of synchronous liver resection for colorectal metastasis stratified by extent of liver resection and type of colorectal resection. J Gastrointest Surg. 19:1982–1994. DOI: 10.1007/s11605-015-2895-z. PMID: 26239515.
Article17. Chan AKC, Mason JM, Baltatzis M, Siriwardena AK. 2022; Management of colorectal cancer with synchronous liver metastases: an inception cohort study (CoSMIC). Ann Surg Oncol. 29:1939–1951. DOI: 10.1245/s10434-021-11017-7. PMID: 34716838.18. PelvEx Collaborative. 2020; Simultaneous pelvic exenteration and liver resection for primary rectal cancer with synchronous liver metastases: results from the. Colorectal Dis. 22:1258–1262. DOI: 10.1111/codi.15064. PMID: 32294308.19. Kazi M, Kumar NAN, Rohila J, Sukumar V, Engineer R, Ankathi S, et al. 2021; Minimally invasive versus open pelvic exenterations for rectal cancer: a comparative analysis of perioperative and 3-year oncological outcomes. BJS Open. 5:zrab074. DOI: 10.1093/bjsopen/zrab074. PMID: 34518872. PMCID: PMC8438253.
Article20. Kanemitsu Y, Shimizu Y, Mizusawa J, Inaba Y, Hamaguchi T, Shida D, et al. 2021; Hepatectomy followed by mFOLFOX6 versus hepatectomy alone for liver-only metastatic colorectal cancer (JCOG0603): a phase II or III randomized controlled trial. J Clin Oncol. 39:3789–3799. DOI: 10.1200/JCO.21.01032. PMID: 34520230.
Article21. Bridgewater JA, Pugh SA, Maishman T, Eminton Z, Mellor J, Whitehead A, et al. 2020; Systemic chemotherapy with or without cetuximab in patients with resectable colorectal liver metastasis (New EPOC): long-term results of a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol. 21:398–411. DOI: 10.1016/S1470-2045(19)30798-3. PMID: 32014119.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oncologic outcomes following metastasectomy in colorectal cancer patients developing distant metastases after initial treatment
- Simultaneous Laparoscopy-Assisted Resection for Colorectal Cancer and Metastases
- Laparoscopic combined colorectal and liver resections for primary colorectal cancer with synchronous liver metastases
- Surgical resection of synchronous and metachronous lung and liver metastases of colorectal cancers
- Aggressive surgical resection for concomitant liver and lung metastasis in colorectal cancer