Ewha Med J.
2023 Jan;46(1):e1. 10.12771/emj.2023.e1.
Relationship between the Stimulated Peak Growth Hormone Level and Metabolic Parameters in Children with Growth Hormone Deficiency
- Affiliations
-
- 1Department of Pediatrics, SMG-SNU Boramae Medical Center, Seoul, Korea
- KMID: 2539442
- DOI: http://doi.org/10.12771/emj.2023.e1
Abstract
Objectives
This study investigated the relationship between the stimulated peak growth hormone (PGH) level and comprehensive metabolic markers for glucose and lipid metabolism, and liver steatosis in prepubertal children with GH deficiency (GHD).
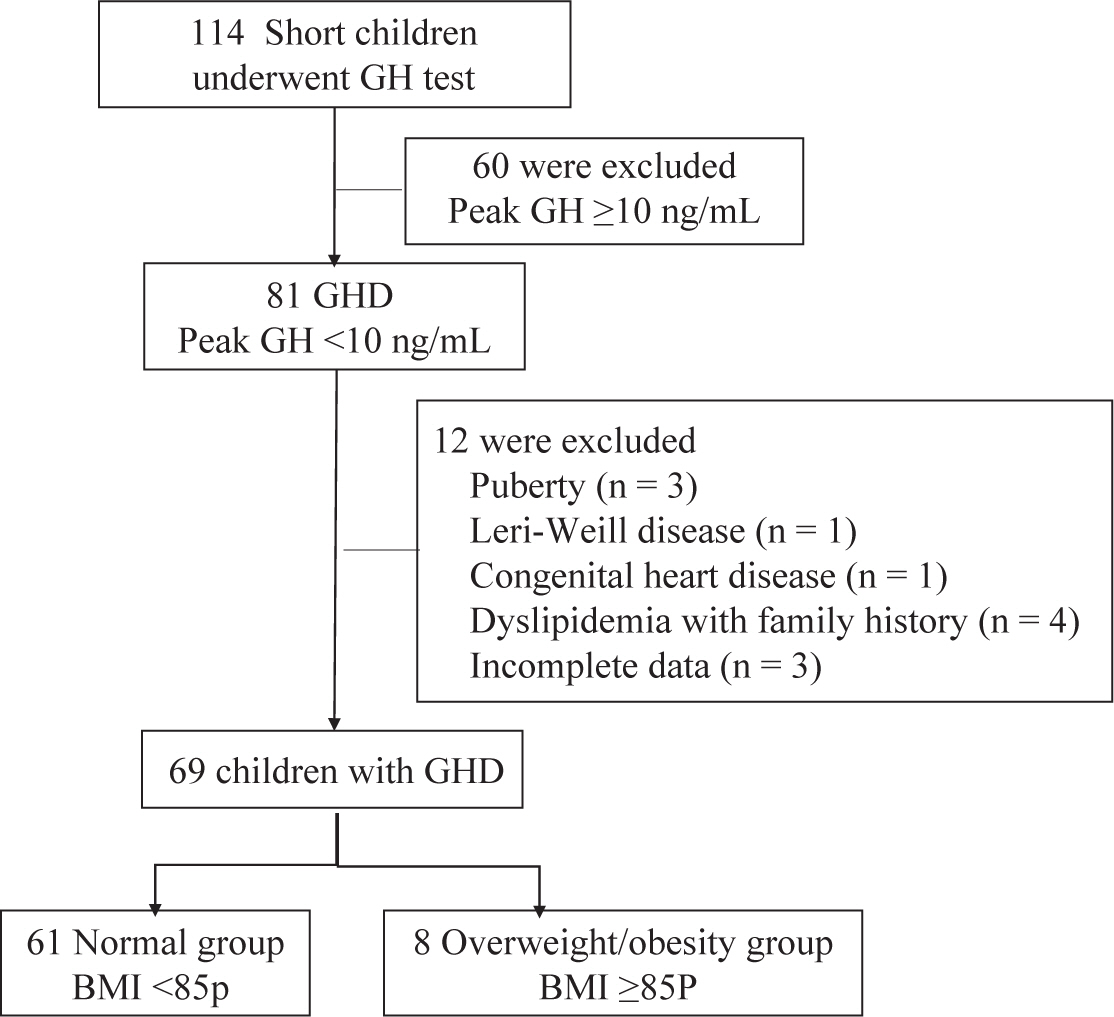
Methods
Sixty-nine prepubertal children with GHD were divided into overweight/obesity (body mass index [BMI]≥85th percentile) and normal BMI groups. The associations between PGH level and metabolic parameters including homeostatic model assessment-insulin resistance (HOMA-IR), lipid profiles, AST, and ALT were evaluated.
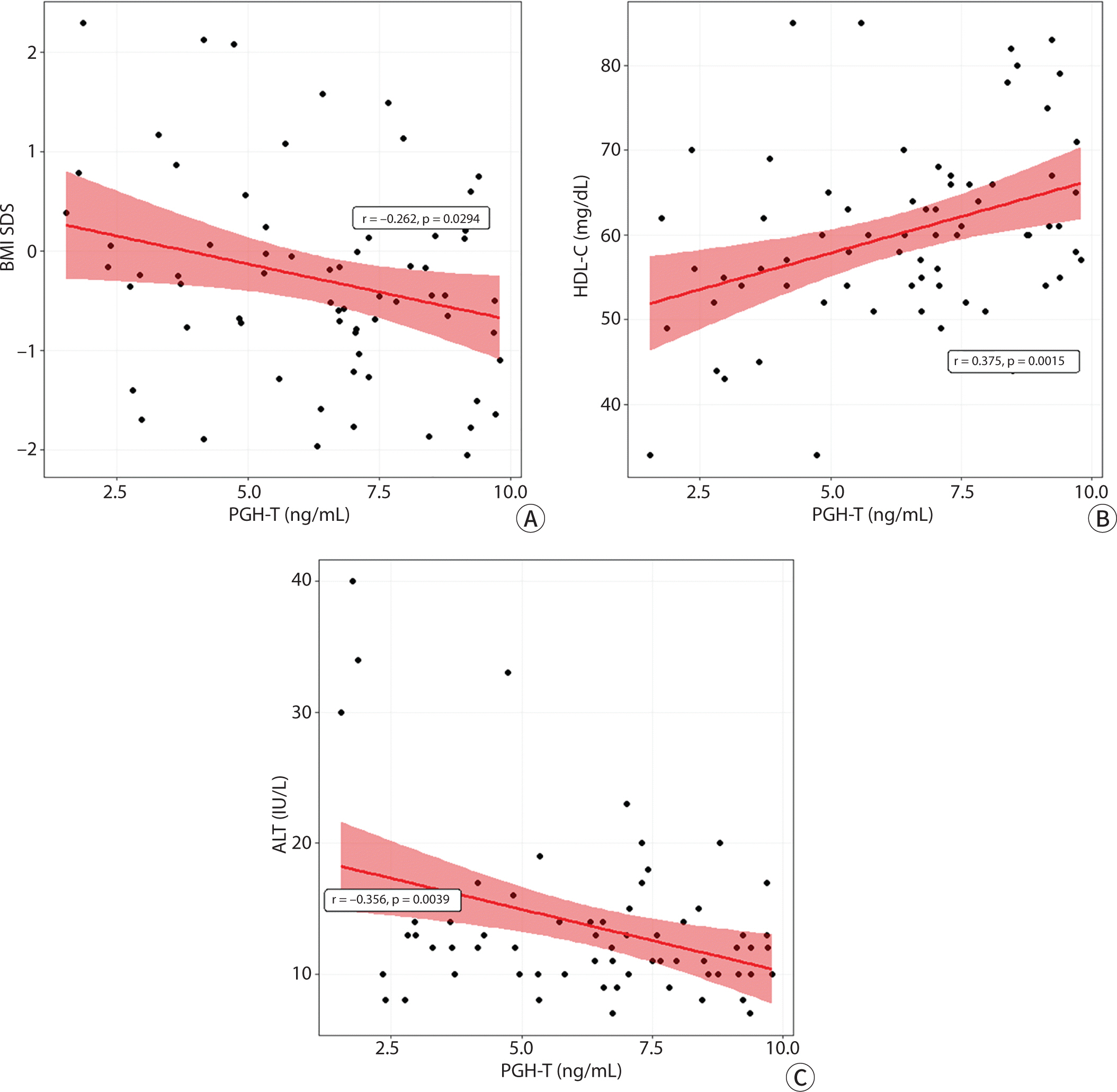
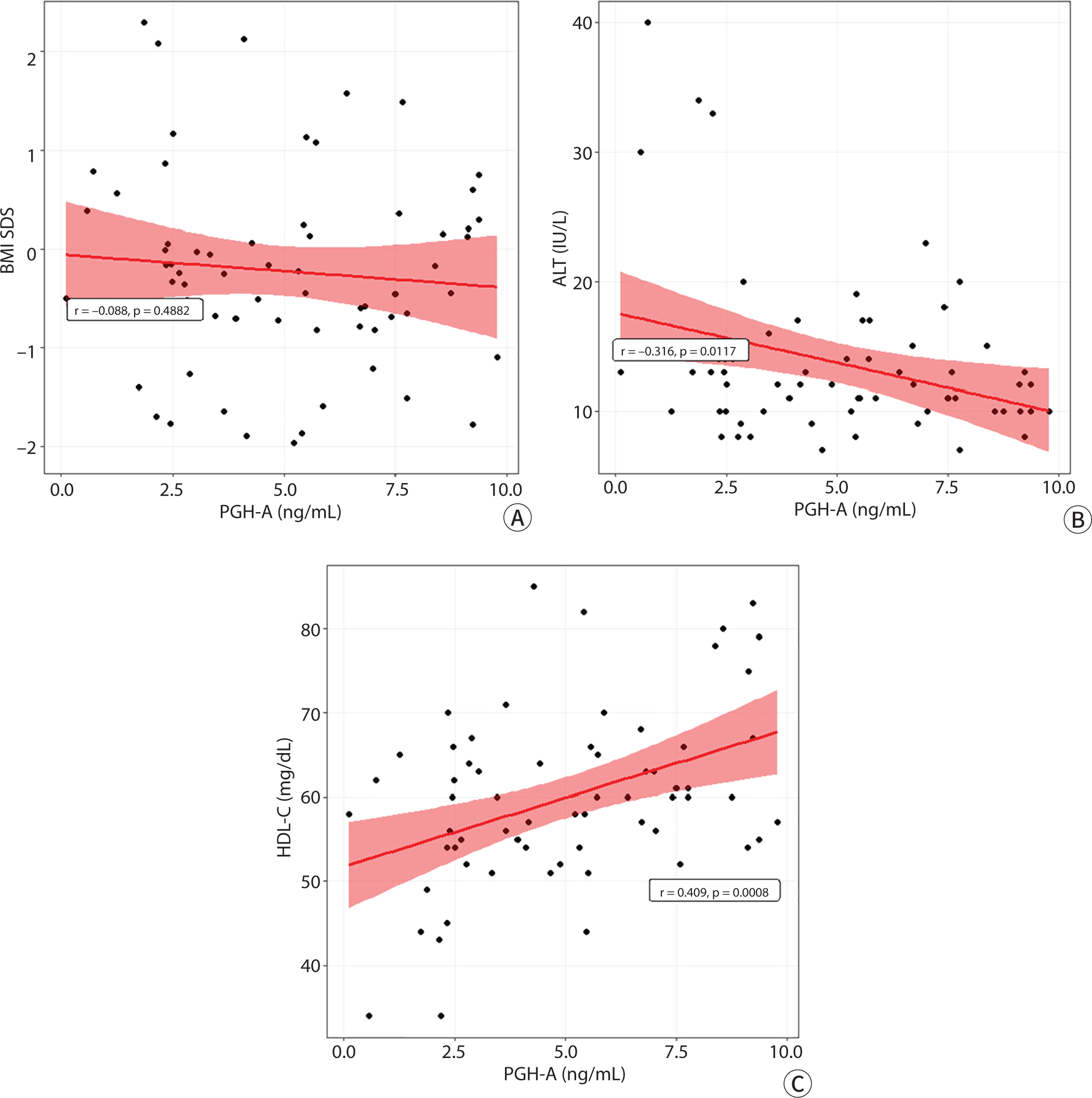
Results
The LDL cholesterol level was significantly higher in the overweight/obesity group than in the normal BMI group. PGH level was negatively associated with the BMI SD score (SDS) (r= −0.26, P=0.029) and ALT (r=−0.36, P=0.004) levels, whereas it was positively associated with the HDL-cholesterol (HDL-C) level (r=0.38, P=0.002). In multivariate analyses, PGH level was positively associated with HDL-C level (P=0.002) and negatively associated with ALT level (P=0.028) after adjusting for age, sex, BMI SDS, HOMA-IR, and TG level.
Conclusion
PGH level in pre-pubertal children with GHD was positively and negatively associated with HDL-C and ALT, respectively, even if they were within normal range, regardless of BMI.
Keyword
Figure
Reference
-
References
1. Cappa M, Loche S. Evaluation of growth disorders in the paediatric clinic. J Endocrinol Invest. 2003; 26:S54–S63.2. Tassoni P, Cacciari E, Cau M, Colli C, Tosi M, Zucchini S, et al. Variability of growth hormone response to pharmacological and sleep tests performed twice in short children. J Clin Endocrinol Metab. 1990; 71(1):230–234. DOI: 10.1210/jcem-71-1-230. PMID: 2370294.3. Devesa J, Lima L, Lois N, Fraga C, Lechuga MJ, Arce V, et al. Reasons for the variability in growth hormone (GH) responses to GHRH challenge: the endogenous hypothalamic-somatotroph rhythm (HSR). Clin Endocrinol. 1989; 30(4):367–377. DOI: 10.1111/j.1365-2265.1989.tb00434.x. PMID: 2574645.4. Loche S, Guzzetti C, Pilia S, Ibba A, Civolani P, Porcu M, et al. Effect of body mass index on the growth hormone response to clonidine stimulation testing in children with short stature. Clin Endocrinol. 2011; 74(6):726–731. DOI: 10.1111/j.1365-2265.2011.03988.x. PMID: 21521260.5. Stanley TL, Levitsky LL, Grinspoon SK, Misra M. Effect of body mass index on peak growth hormone response to provocative testing in children with short stature. J Clin Endocrinol Metab. 2009; 94(12):4875–4881. DOI: 10.1210/jc.2009-1369. PMID: 19890023. PMCID: PMC2795667.6. Yang A, Cho SY, Kwak MJ, Kim SJ, Park SW, Jin DK, et al. Impact of BMI on peak growth hormone responses to provocative tests and therapeutic outcome in children with growth hormone deficiency. Sci Rep. 2019; 9(1):16181. DOI: 10.1038/s41598-019-52644-1. PMID: 31700044. PMCID: PMC6838176.7. Lee NY, Kim SE, Kim S, Ahn MB, Kim SH, Cho WK, et al. Effect of body mass index on peak growth hormone level after growth hormone stimulation test in children with short stature. Ann Pediatr Endocrinol Metab. 2021; 26(3):192–198. DOI: 10.6065/apem.2040246.123. PMID: 34015903. PMCID: PMC8505037.8. Misra M, Bredella MA, Tsai P, Mendes N, Miller KK, Klibanski A. Lower growth hormone and higher cortisol are associated with greater visceral adiposity, intramyocellular lipids, and insulin resistance in overweight girls. Am J Physiol Endocrinol Metab. 2008; 295(2):E385–E392. DOI: 10.1152/ajpendo.00052.2008. PMID: 18544645. PMCID: PMC2519763.9. Barrett J, Maranda L, Nwosu BU. The relationship between subnormal peak-stimulated growth hormone levels and auxological characteristics in obese children. Front Endocrinol. 2014; 5:35. DOI: 10.3389/fendo.2014.00035. PMID: 24723909. PMCID: PMC3971160.10. Stanley TL, Feldpausch MN, Murphy CA, Grinspoon SK, Makimura H. Discordance of IGF-1 and GH stimulation testing for altered GH secretion in obesity. Growth Horm IGF Res. 2014; 24(1):10–15. DOI: 10.1016/j.ghir.2013.11.001. PMID: 24291224. PMCID: PMC3946615.11. Wilson JR, Utz AL, Devin JK. Effects of gender, body weight, and blood glucose dynamics on the growth hormone response to the glucagon stimulation test in patients with pituitary disease. Growth Horm IGF Res. 2016; 26:24–31. DOI: 10.1016/j.ghir.2015.12.005. PMID: 26774402. PMCID: PMC4716555.12. Abawi O, Augustijn D, Hoeks SE, de Rijke YB, van den Akker ELT. Impact of body mass index on growth hormone stimulation tests in children and adolescents: a systematic review and meta-analysis. Crit Rev Clin Lab Sci. 2021; 58(8):576–595. DOI: 10.1080/10408363.2021.1956423. PMID: 34431447.13. Møller N, Jørgensen JO. Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. Endocr Rev. 2009; 30(2):152–177. DOI: 10.1210/er.2008-0027. PMID: 19240267.14. Sperling MA. Traditional and novel aspects of the metabolic actions of growth hormone. Growth Horm IGF Res. 2016; 28:69–75. DOI: 10.1016/j.ghir.2015.06.005. PMID: 26194064.15. Cordido F, Garcia-Buela J, Sangiao-Alvarellos S, Martinez T, Vidal O. The decreased growth hormone response to growth hormone releasing hormone in obesity is associated to cardiometabolic risk factors. Mediators Inflamm. 2010; 2010:434562. DOI: 10.1155/2010/434562. PMID: 20150954. PMCID: PMC2817384.16. Lo J, You SM, Wei J, Canavan B, Grinspoon S. Relationship of peak growth hormone to cardiovascular parameters, waist circumference, lipids and glucose in-HIV infected patients and healthy adults. Clin Endocrinol. 2009; 71(6):815–822. DOI: 10.1111/j.1365-2265.2009.03603.x. PMID: 19508594. PMCID: PMC2889024.17. Nishizawa H, Iguchi G, Murawaki A, Fukuoka H, Hayashi Y, Kaji H, et al. Nonalcoholic fatty liver disease in adult hypopituitary patients with GH deficiency and the impact of GH replacement therapy. Eur J Endocrinol. 2012; 167(1):67–74. DOI: 10.1530/EJE-12-0252. PMID: 22535644.18. Diniz RD, Souza RM, Salvatori R, Franca A, Gomes-Santos E, Ferrão TO, et al. Liver status in congenital, untreated, isolated GH deficiency. Endocr Connect. 2014; 3(3):132–137. DOI: 10.1530/EC-14-0078. PMID: 25117570. PMCID: PMC4151384.19. Lee YJ, Choi Y, Yoo HW, Lee YA, Shin CH, Choi HS, et al. Metabolic impacts of discontinuation and resumption of recombinant human growth hormone treatment during the transition period in patients with childhood-onset growth hormone deficiency. Endocrinol Metab. 2022; 37(2):359–368. DOI: 10.3803/EnM.2021.1384. PMID: 35504604. PMCID: PMC9081298.20. Kang SJ, Kwon A, Jung MK, Chae HW, Kim S, Koh H, et al. High prevalence of nonalcoholic fatty liver disease among adolescents and young adults with hypopituitarism due to growth hormone deficiency. Endocr Pract. 2021; 27(11):1149–1155. DOI: 10.1016/j.eprac.2021.06.003. PMID: 34126247.21. Prodam F, Savastio S, Genoni G, Babu D, Giordano M, Ricotti R, et al. Effects of growth hormone (GH) therapy withdrawal on glucose metabolism in not confirmed GH deficient adolescents at final height. PLoS One. 2014; 9(1):e87157. DOI: 10.1371/journal.pone.0087157. PMID: 24498035. PMCID: PMC3907518.22. LaFranchi S, Hanna CE, Illingworth DR. Effect of growth hormone replacement on development of hypothyroidism and hyperlipidemia. J Pediatr. 1985; 106(4):588–593. DOI: 10.1016/S0022-3476(85)80077-9. PMID: 3981312.23. Chen M, Gan D, Luo Y, Rampersad S, Xu L, Yang S, et al. Effect of recombinant human growth hormone therapy on blood lipid and carotid intima-media thickness in children with growth hormone deficiency. Pediatr Res. 2018; 83(5):954–960. DOI: 10.1038/pr.2017.271. PMID: 29206809. PMCID: PMC6023698.24. Liang S, Zhang D, Qi J, Song X, Xue J. Reduced peak stimulated growth hormone is associated with hyperuricemia in obese children and adolescents. Sci Rep. 2018; 8(1):7931. DOI: 10.1038/s41598-018-26276-w. PMID: 29785038. PMCID: PMC5962610.25. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61(5):135–149. DOI: 10.3345/kjp.2018.61.5.135. PMID: 29853938. PMCID: PMC5976563.26. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18(6):499–502. DOI: 10.1093/clinchem/18.6.499. PMID: 4337382.27. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28(7):412–419. DOI: 10.1007/BF00280883. PMID: 3899825.28. Ciresi A, Giordano C. Glucose metabolism in children with growth hormone deficiency. Front Endocrinol. 2018; 9:321. DOI: 10.3389/fendo.2018.00321. PMID: 29942285. PMCID: PMC6005337.29. Cañete R, Valle M, Martos R, Sánchez-Carrión A, Cañete MD, van Donkelaar EL. Short-term effects of GH treatment on coagulation, fibrinolysis, inflammation biomarkers, and insulin resistance status in prepubertal children with GH deficiency. Eur J Endocrinol. 2012; 167(2):255–260. DOI: 10.1530/EJE-12-0214. PMID: 22645201.30. Husbands S, Ong KK, Gilbert J, Wass JA, Dunger DB. Increased insulin sensitivity in young, growth hormone deficient children. Clin Endocrinol. 2001; 55(1):87–92. DOI: 10.1046/j.1365-2265.2001.01298.x. PMID: 11453956.31. Vahl N, Klausen I, Christiansen JS, Jørgensen JO. Growth hormone (GH) status is an independent determinant of serum levels of cholesterol and triglycerides in healthy adults. Clin Endocrinol. 1999; 51(3):309–316. DOI: 10.1046/j.1365-2265.1999.00772.x. PMID: 10469010.32. Carmichael JD, Danoff A, Milani D, Roubenoff R, Lesser ML, Livote E, et al. GH peak response to GHRH-arginine: relationship to insulin resistance and other cardiovascular risk factors in a population of adults aged 50-90. Clin Endocrinol. 2006; 65(2):169–177. DOI: 10.1111/j.1365-2265.2006.02569.x. PMID: 16886956. PMCID: PMC1618818.33. Zhao Q, Chu Y, Pan Y, Zhang M, Ban B. Association between triglyceride glucose index and peak growth hormone in children with short stature. Sci Rep. 2021; 11(1):1969. DOI: 10.1038/s41598-021-81564-2. PMID: 33479436. PMCID: PMC7820337.34. Dichtel LE, Corey KE, Misdraji J, Bredella MA, Schorr M, Osganian SA, et al. The association between IGF-1 levels and the histologic severity of nonalcoholic fatty liver disease. Clin Transl Gastroenterol. 2017; 8(1):e217. DOI: 10.1038/ctg.2016.72. PMID: 28125073. PMCID: PMC5288606.35. Dichtel LE, Corey KE, Haines MS, Chicote ML, Kimball A, Colling C, et al. The GH/IGF-1 axis is associated with intrahepatic lipid content and hepatocellular damage in overweight/obesity. J Clin Endocrinol Metab. 2022; 107(9):e3624–3632. DOI: 10.1210/clinem/dgac405. PMID: 35779256.36. Ji B, Zhang M, Zhao Q, Chu Y, Li Y, Pan H, et al. Association between alanine aminotransferase and growth hormone: a retrospective cohort study of short children and adolescents. Biomed Res Int. 2019; 2019:5939372. DOI: 10.1155/2019/5939372. PMID: 31073528. PMCID: PMC6470421.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical effects of yeast derived recombinant methionyl growth hormone in growth hormone deficiency
- Effect of yeast-derived methionyl recombinant growth hormone on growth hormone deficient dwarf
- Relationship of Insulin like Growth Factor I with Pharmacologically Stimulated Growth Hormone Secretion in Growth Hormone Deficient Children
- The mechanism of Arginine-stimulated growth hormone secretion
- Quantification of human urinary growth hormone and its clinical significance in the diagnosis of growth hormone deficiency