Healthc Inform Res.
2023 Jan;29(1):23-30. 10.4258/hir.2023.29.1.23.
Clinical Decision Support System for Geriatric Dental Treatment Using a Bayesian Network and a Convolutional Neural Network
- Affiliations
-
- 1Faculty of Dentistry, Srinakharinwirot University, Bangkok, Thailand
- 2Faculty of Dentistry, Thammasat University, Pathumthani, Thailand
- 3ODDS, Bangkok, Thailand
- KMID: 2539395
- DOI: http://doi.org/10.4258/hir.2023.29.1.23
Abstract
Objectives
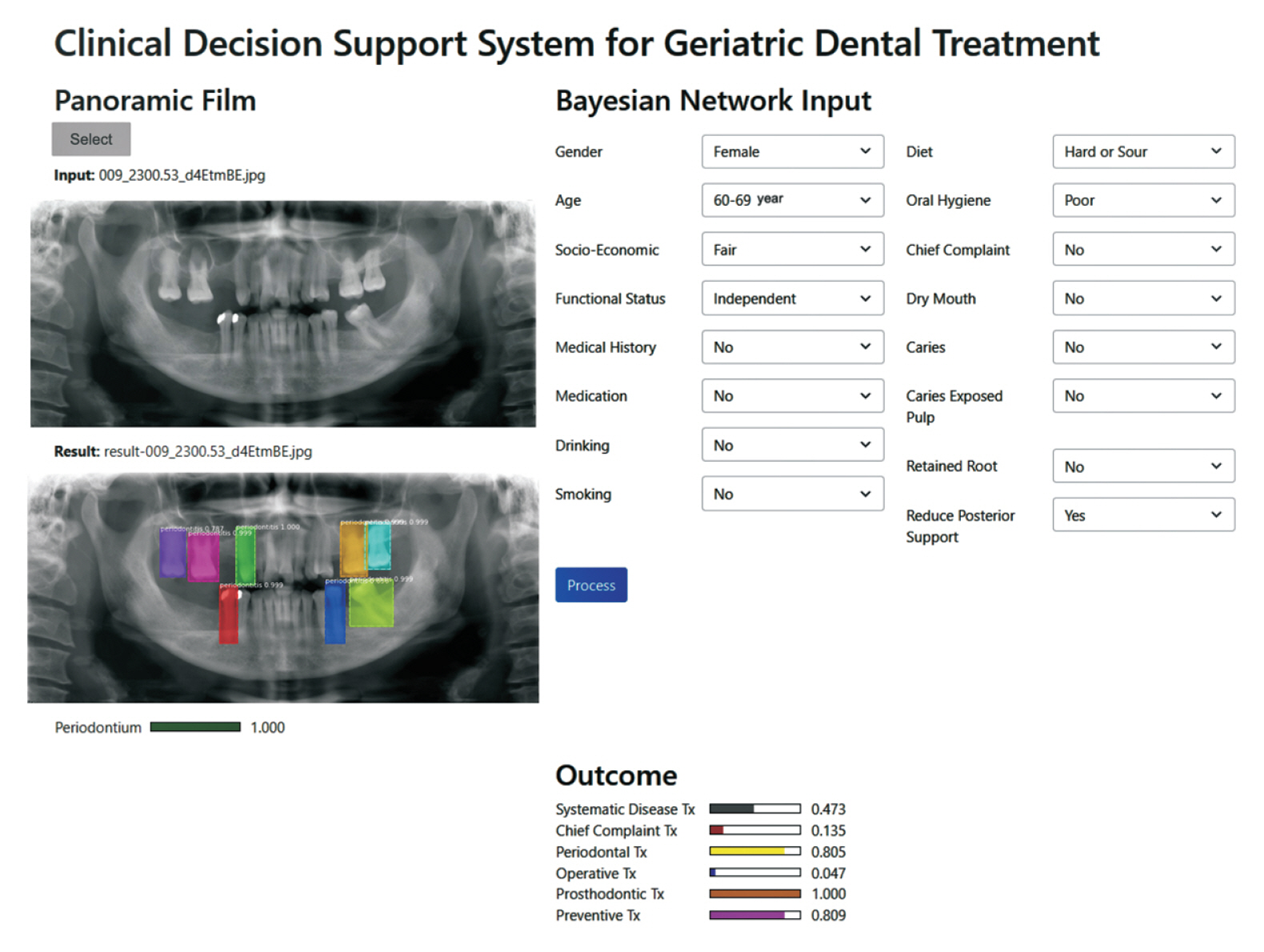
The aim of this study was to evaluate the performance of a clinical decision support system (CDSS) for therapeutic plans in geriatric dentistry. The information that needs to be considered in a therapeutic plan includes not only the patient’s oral health status obtained from an oral examination, but also other related factors such as underlying diseases, socioeconomic characteristics, and functional dependency.
Methods
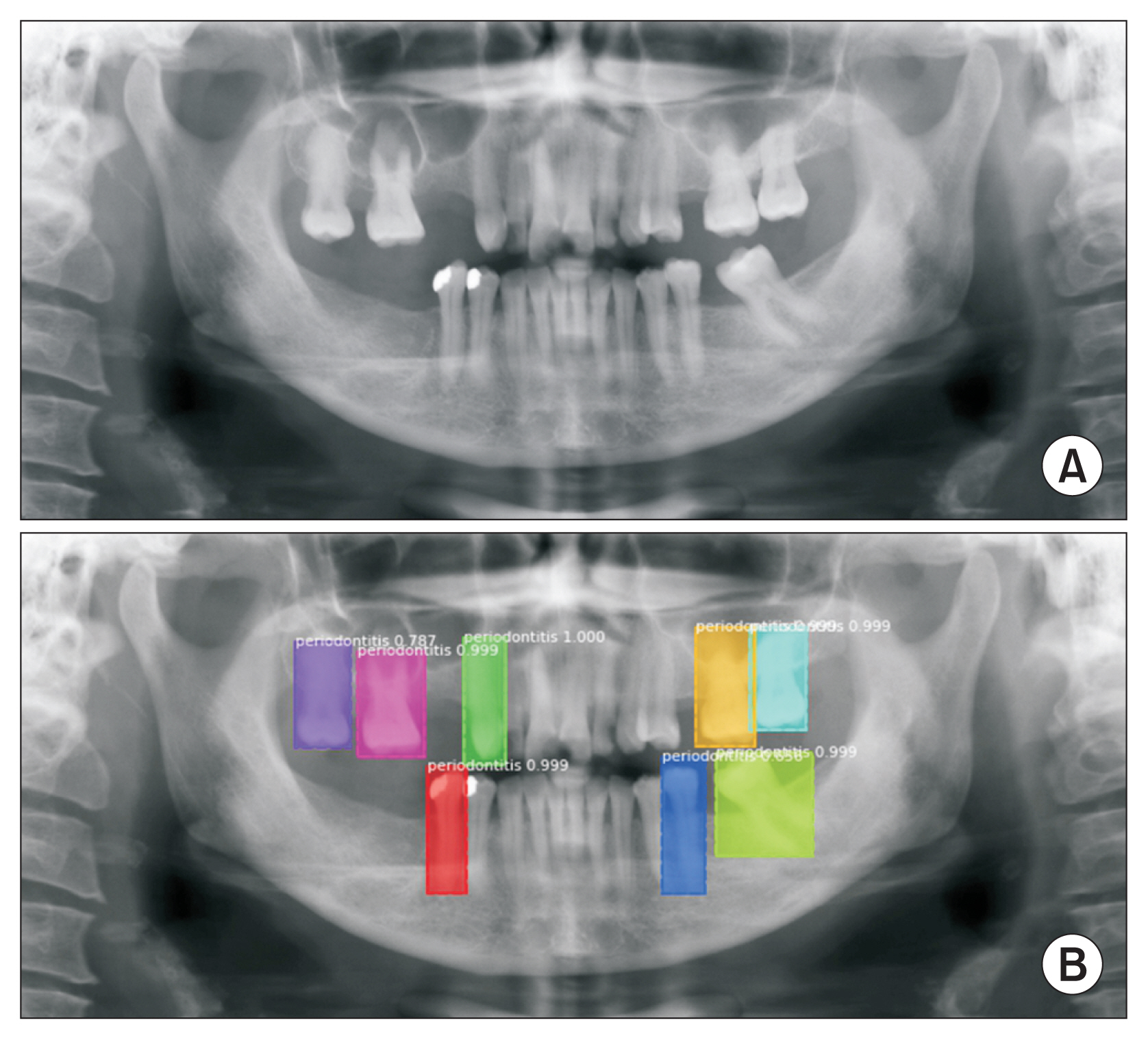
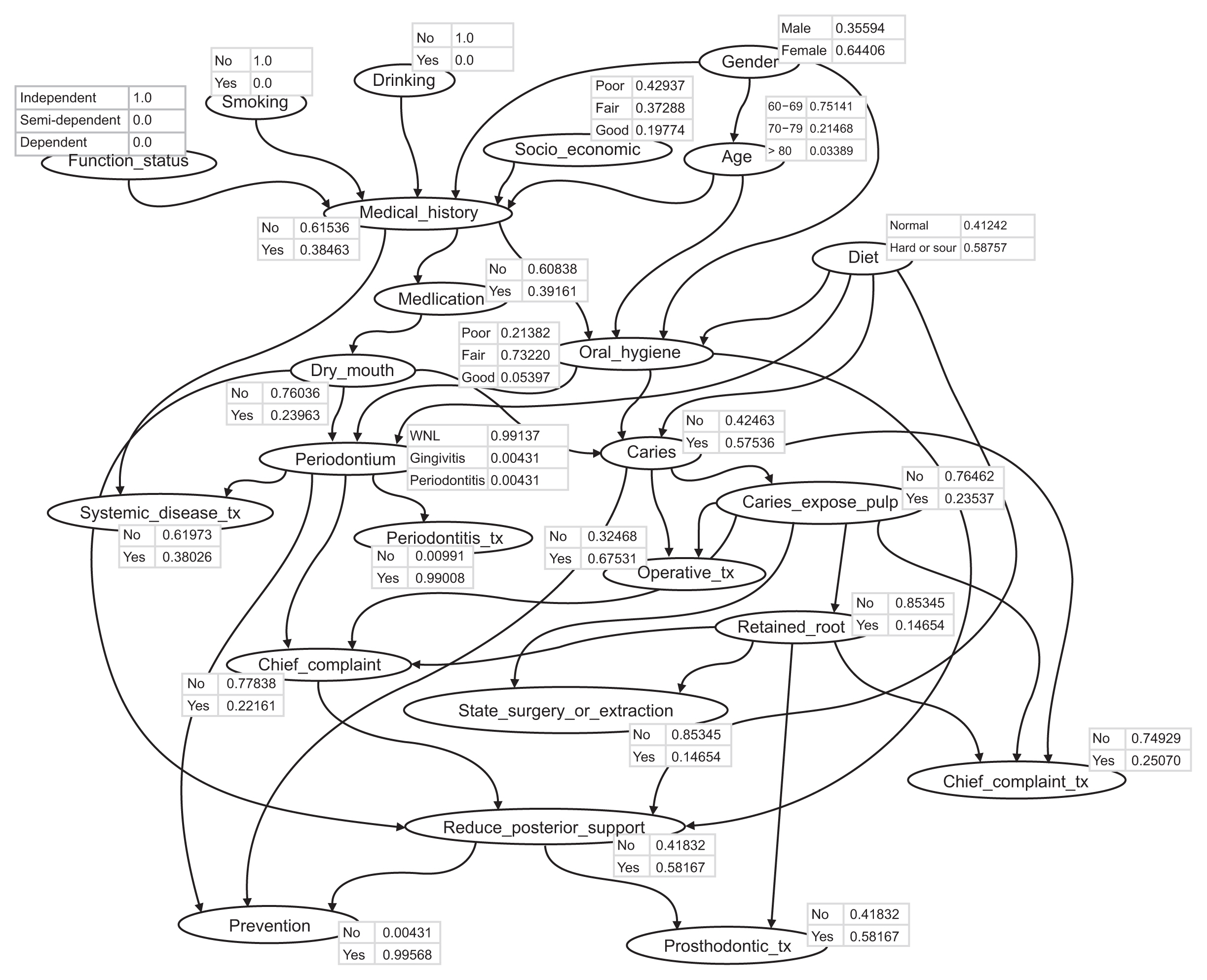
A Bayesian network (BN) was used as a framework to construct a model of contributing factors and their causal relationships based on clinical knowledge and data. The faster R-CNN (regional convolutional neural network) algorithm was used to detect oral health status, which was part of the BN structure. The study was conducted using retrospective data from 400 patients receiving geriatric dental care at a university hospital between January 2020 and June 2021.
Results
The model showed an F1-score of 89.31%, precision of 86.69%, and recall of 82.14% for the detection of periodontally compromised teeth. A receiver operating characteristic curve analysis showed that the BN model was highly accurate for recommending therapeutic plans (area under the curve = 0.902). The model performance was compared to that of experts in geriatric dentistry, and the experts and the system strongly agreed on the recommended therapeutic plans (kappa value = 0.905).
Conclusions
This research was the first phase of the development of a CDSS to recommend geriatric dental treatment. The proposed system, when integrated into the clinical workflow, is expected to provide general practitioners with expert-level decision support in geriatric dental care.
Figure
Reference
-
References
1. Strehler BL. Understanding aging. Barnett YA, Barnett CR, editors. Aging methods and protocols. Totowa (NJ): Humana Press;2000. p. 1–19. https://doi.org/10.1385/1-59259-070-5:1 .2. Petersen PE, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005; 33(2):81–92. https://doi.org/10.1111/j.1600-0528.2004.00219.x .3. Mealey BL, Oates TW; American Academy of Periodontology. Diabetes mellitus and periodontal diseases. J Periodontol. 2006; 77(8):1289–303. https://doi.org/10.1902/jop.2006.050459 .4. Meurman JH, Sanz M, Janket SJ. Oral health, atherosclerosis, and cardiovascular disease. Crit Rev Oral Biol Med. 2004; 15(6):403–13. https://doi.org/10.1177/154411130401500606 .5. Smith BJ, Shay K. What predicts oral health stability in a long-term care population? Spec Care Dentist. 2005; 25(3):150–7. https://doi.org/10.1111/j.1754-4505.2005.tb01426.x .6. Patel VL, Shortliffe EH, Stefanelli M, Szolovits P, Berthold MR, Bellazzi R, et al. The coming of age of artificial intelligence in medicine. Artif Intell Med. 2009; 46(1):5–17. https://doi.org/10.1016/j.artmed.2008.07.017 .7. Warin K, Limprasert W, Suebnukarn S, Jinaporntham S, Jantana P. Automatic classification and detection of oral cancer in photographic images using deep learning algorithms. J Oral Pathol Med. 2021; 50(9):911–8. https://doi.org/10.1111/jop.13227 .8. Shortliffe EH, Sepulveda MJ. Clinical decision support in the era of artificial intelligence. JAMA. 2018; 320(21):2199–200. https://doi.org/10.1001/jama.2018.17163 .9. Lauritzen SL. The EM algorithm for graphical association models with missing data. Comput Stat Data Anal. 1995; 19(2):191–201. https://doi.org/10.1016/0167-9473(93)E0056-A .10. Ren S, He K, Girshick R, Sun J. Faster R-CNN: towards real-time object detection with region proposal networks. IEEE Trans Pattern Anal Mach Intell. 2017; 39(6):1137–49. https://doi.org/10.1109/TPAMI.2016.2577031 .11. Jiao Y, Du P. Performance measures in evaluating machine learning based bioinformatics predictors for classifications. Quant Biol. 2016; 4(4):320–30. https://doi.org/10.1007/s40484-016-0081-2 .12. Taheri Moghadam S, Sadoughi F, Velayati F, Ehsanzadeh SJ, Poursharif S. The effects of clinical decision support system for prescribing medication on patient outcomes and physician practice performance: a systematic review and meta-analysis. BMC Med Inform Decis Mak. 2021; 21(1):98. https://doi.org/10.1186/s12911-020-01376-8 .13. Damoiseaux-Volman BA, van der Velde N, Ruige SG, Romijn JA, Abu-Hanna A, Medlock S. Effect of interventions with a clinical decision support system for hospitalized older patients: systematic review mapping implementation and design factors. JMIR Med Inform. 2021; 9:e28023. https://doi.org/10.2196/28023 .14. Abdellatif A, Bouaud J, Lafuente-Lafuente C, Belmin J, Seroussi B. Computerized decision support systems for nursing homes: a scoping review. J Am Med Dir Assoc. 2021; 22:984–94. https://doi.org/10.1016/j.jamda.2021.01.080 .15. Kim M, Yun J, Cho Y, Shin K, Jang R, Bae HJ, et al. Deep learning in medical imaging. Neurospine. 2019; 16(4):657–68. https://doi.org/10.14245/ns.1938396.198 .16. Min S, Lee B, Yoon S. Deep learning in bioinformatics. Brief Bioinform. 2017; 18(5):851–69. https://doi.org/10.1093/bib/bbw068 .17. Panayides AS, Amini A, Filipovic ND, Sharma A, Tsaftaris SA, Young A, et al. AI in medical imaging informatics: current challenges and future directions. IEEE J Biomed Health Inform. 2020; 24(7):1837–57. https://doi.org/10.1109/JBHI.2020.2991043 .18. Thanathornwong B, Suebnukarn S. Automatic detection of periodontal compromised teeth in digital panoramic radiographs using faster regional convolutional neural networks. Imaging Sci Dent. 2020; 50(2):169–74. https://doi.org/10.5624/isd.2020.50.2.169 .19. Khan HA, Haider MA, Ansari HA, Ishaq H, Kiyani A, Sohail K, et al. Automated feature detection in dental periapical radiographs by using deep learning. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021; 131(6):711–20. https://doi.org/10.1016/j.oooo.2020.08.024 .20. Kompa B, Snoek J, Beam AL. Second opinion needed: communicating uncertainty in medical machine learning. NPJ Digit Med. 2021; 4(1):4. https://doi.org/10.1038/s41746-020-00367-3 .21. Wang G, Jia QS, Qiao J, Bi J, Liu C. A sparse deep belief network with efficient fuzzy learning framework. Neural Netw. 2020; 121:430–40. https://doi.org/10.1016/j.neunet.2019.09.035 .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Hybrid Bayesian Network Model for Predicting Breast Cancer Prognosis
- Convolutional Neural Network Based Sinogram Extrapolation for Truncated CT: Preliminary Study
- Deep learning convolutional neural network algorithms for the early detection and diagnosis of dental caries on periapical radiographs: A systematic review
- The development of a decision support system for diagnosing nasal allergy
- Bayesian-Based Decision Support System for Assessing the Needs for Orthodontic Treatment