Brain Tumor Res Treat.
2023 Jan;11(1):22-27. 10.14791/btrt.2022.0033.
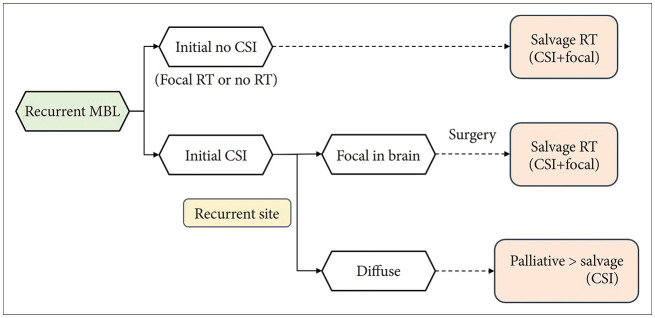
Role of Radiotherapy in Patients With Relapsed Medulloblastoma
- Affiliations
-
- 1Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2539326
- DOI: http://doi.org/10.14791/btrt.2022.0033
Abstract
- During the last three decades, the management of medulloblastoma (MBL) has made enormous progress with a multidisciplinary approach, incorporating surgery, radiotherapy (RT), and chemotherapy. Despite this improvement, 20%–30% of patients with MBL remain at risk of disease recurrence, with its relapse being possibly fatal. To date, the salvage treatment for relapse remains challenging, and various approaches have been suggested for the retreatment. In this review, I have described the characteristics of patients with relapsed MBL, patterns of relapse and the most commonly prescribed treatment. Further, I have reviewed the studies on re-irradiation and its associated issues to conclusively suggest the RT recommendations for patients with relapsed MBL.
Keyword
Figure
Reference
-
1. Packer RJ, Sutton LN, D'Angio G, Evans AE, Schut L. Management of children with primitive neuroectodermal tumors of the posterior fossa/ medulloblastoma. Pediatr Neurosci. 1985-86; 12:272–282. PMID: 3039477.2. Packer RJ, Goldwein J, Nicholson HS, Vezina LG, Allen JC, Ris MD, et al. Treatment of children with medulloblastomas with reduced-dose craniospinal radiation therapy and adjuvant chemotherapy: a children’s cancer group study. J Clin Oncol. 1999; 17:2127–2136. PMID: 10561268.3. Gajjar A, Chintagumpala M, Ashley D, Kellie S, Kun LE, Merchant TE, et al. Risk-adapted craniospinal radiotherapy followed by high-dose chemotherapy and stem-cell rescue in children with newly diagnosed medulloblastoma (St Jude Medulloblastoma-96): long-term results from a prospective, multicentre trial. Lancet Oncol. 2006; 7:813–820. PMID: 17012043.4. Packer RJ, Gajjar A, Vezina G, Rorke-Adams L, Burger PC, Robertson PL, et al. Phase III study of craniospinal radiation therapy followed by adjuvant chemotherapy for newly diagnosed average-risk medulloblastoma. J Clin Oncol. 2006; 24:4202–4208. PMID: 16943538.5. Carrie C, Grill J, Figarella-Branger D, Bernier V, Padovani L, Habrand JL, et al. Online quality control, hyperfractionated radiotherapy alone and reduced boost volume for standard risk medulloblastoma: long-term results of MSFOP 98. J Clin Oncol. 2009; 27:1879–1883. PMID: 19273707.6. Lannering B, Rutkowski S, Doz F, Pizer B, Gustafsson G, Navajas A, et al. Hyperfractionated versus conventional radiotherapy followed by chemotherapy in standard-risk medulloblastoma: results from the randomized multicenter HIT-SIOP PNET 4 trial. J Clin Oncol. 2012; 30:3187–3193. PMID: 22851561.7. Packer RJ, Zhou T, Holmes E, Vezina G, Gajjar A. Survival and secondary tumors in children with medulloblastoma receiving radiotherapy and adjuvant chemotherapy: results of children’s oncology group trial A9961. Neuro Oncol. 2013; 15:97–103. PMID: 23099653.8. Bowers DC, Gargan L, Weprin BE, Mulne AF, Elterman RD, Munoz L, et al. Impact of site of tumor recurrence upon survival for children with recurrent or progressive medulloblastoma. J Neurosurg. 2007; 107(1 Suppl):5–10. PMID: 17644914.9. Sabel M, Fleischhack G, Tippelt S, Gustafsson G, Doz F, Kortmann R, et al. Relapse patterns and outcome after relapse in standard risk medulloblastoma: a report from the HIT-SIOP-PNET4 study. J Neurooncol. 2016; 129:515–524. PMID: 27423645.
Article10. Koschmann C, Bloom K, Upadhyaya S, Geyer JR, Leary SE. Survival after relapse of medulloblastoma. J Pediatr Hematol Oncol. 2016; 38:269–273. PMID: 26907655.11. Johnston DL, Keene D, Strother D, Taneva M, Lafay-Cousin L, Fryer C, et al. Survival following tumor recurrence in children with medulloblastoma. J Pediatr Hematol Oncol. 2018; 40:e159–e163. PMID: 29432312.12. von Bueren AO, von Hoff K, Pietsch T, Gerber NU, Warmuth-Metz M, Deinlein F, et al. Treatment of young children with localized medulloblastoma by chemotherapy alone: results of the prospective, multicenter trial HIT 2000 confirming the prognostic impact of histology. Neuro Oncol. 2011; 13:669–679. PMID: 21636711.13. Dhall G, Grodman H, Ji L, Sands S, Gardner S, Dunkel IJ, et al. Outcome of children less than three years old at diagnosis with non-metastatic medulloblastoma treated with chemotherapy on the “head start” I and II protocols. Pediatr Blood Cancer. 2008; 50:1169–1175. PMID: 18293379.14. Muller K, Mynarek M, Zwiener I, Siegler N, Zimmermann M, Christiansen H, et al. Postponed is not canceled: role of craniospinal radiation therapy in the management of recurrent infant medulloblastoma--an experience from the HIT-REZ 1997 & 2005 studies. Int J Radiat Oncol Biol Phys. 2014; 88:1019–1024. PMID: 24661654.15. Hill RM, Richardson S, Schwalbe EC, Hicks D, Lindsey JC, Crosier S, et al. Time, pattern, and outcome of medulloblastoma relapse and their association with tumour biology at diagnosis and therapy: a multicentre cohort study. Lancet Child Adolesc Health. 2020; 4:865–874. PMID: 33222802.16. Ramaswamy V, Remke M, Bouffet E, Faria CC, Perreault S, Cho YJ, et al. Recurrence patterns across medulloblastoma subgroups: an integrated clinical and molecular analysis. Lancet Oncol. 2013; 14:1200–1207. PMID: 24140199.
Article17. Warmuth-Metz M, Blashofer S, von Bueren AO, von Hoff K, Bison B, Pohl F, et al. Recurrence in childhood medulloblastoma. J Neurooncol. 2011; 103:705–711. PMID: 21069427.
Article18. Huybrechts S, Le Teuff G, Tauziede-Espariat A, Rossoni C, Chivet A, Indersie E, et al. Prognostic clinical and biologic features for overall survival after relapse in childhood medulloblastoma. Cancers (Basel). 2020; 13:53. PMID: 33375523.
Article19. Lobon MJ, Bautista F, Riet F, Dhermain F, Canale S, Dufour C, et al. Re-irradiation of recurrent pediatric ependymoma: modalities and outcomes: a twenty-year survey. Springerplus. 2016; 5:879. PMID: 27386327.
Article20. Zacharoulis S, Ashley S, Moreno L, Gentet JC, Massimino M, Frappaz D. Treatment and outcome of children with relapsed ependymoma: a multi-institutional retrospective analysis. Childs Nerv Syst. 2010; 26:905–911. PMID: 20039045.
Article21. Eaton BR, Chowdhry V, Weaver K, Liu L, Ebb D, MacDonald SM, et al. Use of proton therapy for re-irradiation in pediatric intracranial ependymoma. Radiother Oncol. 2015; 116:301–308. PMID: 26243681.
Article22. Tsang DS, Murray L, Ramaswamy V, Zapotocky M, Tabori U, Bartels U, et al. Craniospinal irradiation as part of re-irradiation for children with recurrent intracranial ependymoma. Neuro Oncol. 2019; 21:547–557. PMID: 30452715.
Article23. Bakst RL, Dunkel IJ, Gilheeney S, Khakoo Y, Becher O, Souweidane MM, et al. Reirradiation for recurrent medulloblastoma. Cancer. 2011; 117:4977–4982. PMID: 21495027.24. Wetmore C, Herington D, Lin T, Onar-Thomas A, Gajjar A, Merchant TE. Reirradiation of recurrent medulloblastoma: does clinical benefit outweigh risk for toxicity? Cancer. 2014; 120:3731–3737. PMID: 25080363.
Article25. Gupta T, Maitre M, Sastri GJ, Krishnatry R, Shirsat N, Epari S, et al. Outcomes of salvage re-irradiation in recurrent medulloblastoma correlate with age at initial diagnosis, primary risk-stratification, and molecular subgrouping. J Neurooncol. 2019; 144:283–291. PMID: 31236820.
Article26. Tsang DS, Sarhan N, Ramaswamy V, Nobre L, Yee R, Taylor MD, et al. Re-irradiation for children with recurrent medulloblastoma in Toronto, Canada: a 20-year experience. J Neurooncol. 2019; 145:107–114. PMID: 31468270.
Article27. Baroni LV, Freytes C, Fernandez Ponce N, Oller A, Pinto N, Gonzalez A, et al. Craniospinal irradiation as part of re-irradiation for children with recurrent medulloblastoma. J Neurooncol. 2021; 155:53–61. PMID: 34505229.
Article28. Grodman H, Wolfe L, Kretschmar C. Outcome of patients with recurrent medulloblastoma or central nervous system germinoma treated with low dose continuous intravenous etoposide along with dose-intensive chemotherapy followed by autologous hematopoietic stem cell rescue. Pediatr Blood Cancer. 2009; 53:33–36. PMID: 19326417.
Article29. Lefkowitz IB, Packer RJ, Siegel KR, Sutton LN, Schut L, Evans AE. Results of treatment of children with recurrent medulloblastoma/primitive neuroectodermal tumors with lomustine, cisplatin, and vincristine. Cancer. 1990; 65:412–417. PMID: 2153428.
Article30. Dunkel IJ, Gardner SL, Garvin JH Jr, Goldman S, Shi W, Finlay JL. High-dose carboplatin, thiotepa, and etoposide with autologous stem cell rescue for patients with previously irradiated recurrent medulloblastoma. Neuro Oncol. 2010; 12:297–303. PMID: 20167818.
Article31. Padovani L, Andre N, Gentet JC, Figarella Branger D, Scavarda D, Verschuur A, et al. Reirradiation and concomitant metronomic temozolomide: an efficient combination for local control in medulloblastoma disease? J Pediatr Hematol Oncol. 2011; 33:600–604. PMID: 22042276.32. Veninga T, Langendijk HA, Slotman BJ, Rutten EH, van der Kogel AJ, Prick MJ, et al. Reirradiation of primary brain tumours: survival, clinical response and prognostic factors. Radiother Oncol. 2001; 59:127–137. PMID: 11325440.
Article33. Sminia P, Mayer R. External beam radiotherapy of recurrent glioma: radiation tolerance of the human brain. Cancers (Basel). 2012; 4:379–399. PMID: 24213316.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Subfrontal Recurrence of Medulloblastoma after Postoperative Whole Neuroaxis Irradiation
- Medulloblastoma Mimicking an Extraaxial Tumor on Radiological Examination
- Medulloblastoma in Adult: 2 Cases Report
- Postoperative External Beam Radiotherapy for Medulloblastoma
- Molecular Pathologic Classification of Medulloblastoma