Intest Res.
2023 Jan;21(1):137-147. 10.5217/ir.2021.00173.
Real-world effectiveness and safety of ustekinumab induction therapy for Korean patients with Crohn’s disease: a KASID prospective multicenter study
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Clinical Epidemiology and Biostatistics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Inflammatory Bowel Disease Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 4Digestive Diseases Research Center, University of Ulsan College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 6Department of Internal Medicine, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea
- 7Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- KMID: 2539012
- DOI: http://doi.org/10.5217/ir.2021.00173
Abstract
- Background/Aims
We investigated the real-world effectiveness and safety of ustekinumab (UST) as induction treatment for Koreans with Crohn’s disease (CD).
Methods
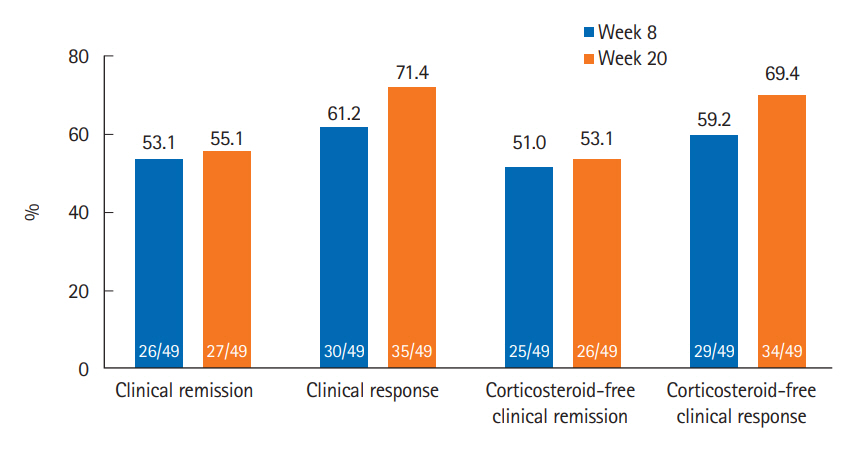
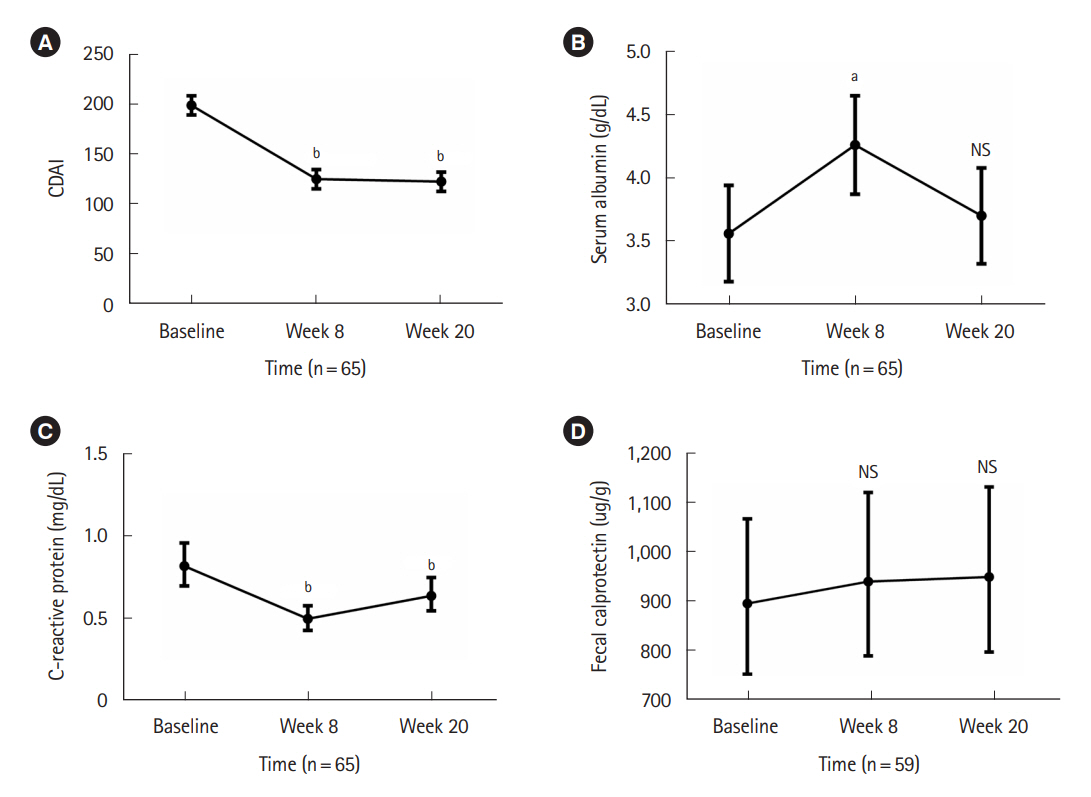
CD patients who started UST were prospectively enrolled from 4 hospitals in Korea. All enrolled patients received intravenous UST infusion at week 0 and subcutaneous UST injection at week 8. Clinical outcomes were assessed using Crohn’s Disease Activity Index (CDAI) scores at weeks 8 and 20 among patients with active disease (CDAI ≥150) at baseline. Clinical remission was defined as a CDAI <150, and clinical response was defined as a reduction in CDAI ≥70 points from baseline. Safety and factors associated with clinical remission at week 20 were also analyzed.
Results
Sixty-five patients were enrolled between January 2019 and December 2020. Among 49 patients with active disease at baseline (CDAI ≥150), clinical remission and clinical response at week 8 were achieved in 26 (53.1%) and 30 (61.2%) patients, respectively. At week 20, 27 (55.1%) and 35 (71.4%) patients achieved clinical remission and clinical response, respectively. Twenty-seven patients (41.5%) experienced adverse events, with serious adverse events in 3 patients (4.6%). One patient (1.5%) stopped UST therapy due to poor response. Underweight (body mass index <18.5 kg/m2) (odds ratio [OR], 0.085; 95% confidence interval [CI], 0.014–0.498; P=0.006) and elevated C-reactive protein at baseline (OR, 0.133; 95% CI, 0.022–0.823; P=0.030) were inversely associated with clinical remission at week 20.
Conclusions
UST was effective and well-tolerated as induction therapy for Korean patients with CD.
Keyword
Figure
Cited by 1 articles
-
Corrigendum: Real-world effectiveness and safety of ustekinumab induction therapy for Korean patients with Crohn’s disease: a KASID prospective multicenter study
Kyunghwan Oh, Hee Seung Hong, Nam Seok Ham, Jungbok Lee, Sang Hyoung Park, Suk-Kyun Yang, Hyuk Yoon, You Sun Kim, Chang Hwan Choi, Byong Duk Ye
Intest Res. 2023;21(2):273-273. doi: 10.5217/ir.2021.00173.e.
Reference
-
1. Ben-Horin S, Chowers Y. Review article: loss of response to antiTNF treatments in Crohn’s disease. Aliment Pharmacol Ther. 2011; 33:987–995.
Article2. Barber GE, Yajnik V, Khalili H, et al. Genetic markers predict primary non-response and durable response to anti-TNF biologic therapies in Crohn’s disease. Am J Gastroenterol. 2016; 111:1816–1822.
Article3. Gisbert JP, Marín AC, McNicholl AG, Chaparro M. Systematic review with meta-analysis: the efficacy of a second anti-TNF in patients with inflammatory bowel disease whose previous anti-TNF treatment has failed. Aliment Pharmacol Ther. 2015; 41:613–623.
Article4. Gisbert JP, Chaparro M. Use of a third anti-TNF after failure of two previous anti-TNFs in patients with inflammatory bowel disease: is it worth it? Scand J Gastroenterol. 2015; 50:379–386.
Article5. Cohen A, Ahmed N, Sant’Anna A. Ustekinumab for the treatment of refractory pediatric Crohn’s disease: a single-center experience. Intest Res. 2021; 19:217–224.
Article6. Benson JM, Peritt D, Scallon BJ, et al. Discovery and mechanism of ustekinumab: a human monoclonal antibody targeting interleukin-12 and interleukin-23 for treatment of immune-mediated disorders. MAbs. 2011; 3:535–545.7. Peluso I, Pallone F, Monteleone G. Interleukin-12 and Th1 immune response in Crohn’s disease: pathogenetic relevance and therapeutic implication. World J Gastroenterol. 2006; 12:5606–5610.
Article8. Neurath MF. IL-23: a master regulator in Crohn disease. Nat Med. 2007; 13:26–28.
Article9. Sandborn WJ, Feagan BG, Fedorak RN, et al. A randomized trial of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with moderate-to-severe Crohn’s disease. Gastroenterology. 2008; 135:1130–1141.
Article10. Sandborn WJ, Gasink C, Gao LL, et al. Ustekinumab induction and maintenance therapy in refractory Crohn’s disease. N Engl J Med. 2012; 367:1519–1528.
Article11. Feagan BG, Sandborn WJ, Gasink C, et al. Ustekinumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2016; 375:1946–1960.12. Wils P, Bouhnik Y, Michetti P, et al. Subcutaneous ustekinumab provides clinical benefit for two-thirds of patients with Crohn’s disease refractory to anti-tumor necrosis factor agents. Clin Gastroenterol Hepatol. 2016; 14:242–250.
Article13. Khorrami S, Ginard D, Marín-Jiménez I, et al. Ustekinumab for the treatment of refractory Crohn’s disease: the Spanish experience in a large multicentre open-label cohort. Inflamm Bowel Dis. 2016; 22:1662–1669.14. Eberl A, Hallinen T, Af Björkesten CG, et al. Ustekinumab for Crohn’s disease: a nationwide real-life cohort study from Finland (FINUSTE). Scand J Gastroenterol. 2019; 54:718–725.
Article15. Iborra M, Beltrán B, Fernández-Clotet A, et al. Real-world short-term effectiveness of ustekinumab in 305 patients with Crohn’s disease: results from the ENEIDA registry. Aliment Pharmacol Ther. 2019; 50:278–288.16. Kubesch A, Rueter L, Farrag K, et al. Short and long-term effectiveness of ustekinumab in patients with Crohn’s disease: realworld data from a German IBD cohort. J Clin Med. 2019; 8:2140.
Article17. Liefferinckx C, Verstockt B, Gils A, et al. Long-term clinical effectiveness of ustekinumab in patients with Crohn’s disease who failed biologic therapies: a national cohort study. J Crohns Colitis. 2019; 13:1401–1409.
Article18. Biemans VB, van der Meulen-de Jong AE, van der Woude CJ, et al. Ustekinumab for Crohn’s disease: results of the ICC Registry, a nationwide prospective observational cohort study. J Crohns Colitis. 2020; 14:33–45.
Article19. Casas Deza D, García López S, Lafuente Blasco M, et al. Efficacy and safety of ustekinumab in real clinical practice: retrospective multicentre study. ARAINF cohort. Gastroenterol Hepatol. 2020; 43:126–132.
Article20. Gonczi L, Szanto K, Farkas K, et al. Clinical efficacy, drug sustainability and serum drug levels in Crohn’s disease patients treated with ustekinumab: a prospective, multicenter cohort from Hungary. Dig Liver Dis. 2022; 54:207–213.
Article21. Plevris N, Fulforth J, Siakavellas S, et al. Real-world effectiveness and safety of ustekinumab for the treatment of Crohn’s disease: the Scottish ustekinumab cohort. J Gastroenterol Hepatol. 2021; 36:2067–2075.
Article22. Sandborn WJ, Feagan BG, Danese S, et al. Safety of ustekinumab in inflammatory bowel disease: pooled safety analysis of results from phase 2/3 studies. Inflamm Bowel Dis. 2021; 27:994–1007.
Article23. Miyazaki T, Watanabe K, Kojima K, et al. Efficacies and related issues of ustekinumab in Japanese patients with Crohn’s disease: a preliminary study. Digestion. 2020; 101:53–59.
Article24. Murate K, Maeda K, Nakamura M, et al. Endoscopic activity and serum TNF-α level at baseline are associated with clinical response to ustekinumab in Crohn’s disease patients. Inflamm Bowel Dis. 2020; 26:1669–1681.
Article25. Yokoyama S, Asano T, Nagano K, et al. Safety and effectiveness of ustekinumab in Crohn’s disease: interim results of post-marketing surveillance in Japan. J Gastroenterol Hepatol. 2021; 36:3069–3076.
Article26. Park SH, Kim YJ, Rhee KH, et al. A 30-year trend analysis in the epidemiology of inflammatory bowel disease in the Songpa-Kangdong district of Seoul, Korea in 1986-2015. J Crohns Colitis. 2019; 13:1410–1417.
Article27. Kaibullayeva J, Ualiyeva A, Oshibayeva A, Dushpanova A, Marshall JK. Prevalence and patient awareness of inflammatory bowel disease in Kazakhstan: a cross-sectional study. Intest Res. 2020; 18:430–437.
Article28. Sood A, Kaur K, Mahajan R, et al. Colitis and Crohn’s Foundation (India): a first nationwide inflammatory bowel disease registry. Intest Res. 2021; 19:206–216.
Article29. Sood A, Kaur K, Singh A, et al. Trends of inflammatory bowel disease at a tertiary care center in northern India. Intest Res. 2021; 19:282–290.
Article30. Liu JZ, van Sommeren S, Huang H, et al. Association analyses identify 38 susceptibility loci for inflammatory bowel disease and highlight shared genetic risk across populations. Nat Genet. 2015; 47:979–986.
Article31. Yang SK. How does the epidemiology of inflammatory bowel disease differ between East and West? A Korean perspective. Inflamm Intest Dis. 2017; 2:95–101.
Article32. Jung S, Ye BD, Lee HS, et al. Identification of three novel susceptibility loci for inflammatory bowel disease in Koreans in an extended genome-wide association study. J Crohns Colitis. 2021; 15:1898–1907.
Article33. Yang SK, Park M, Lim J, et al. Contribution of IL23R but not ATG16L1 to Crohn’s disease susceptibility in Koreans. Inflamm Bowel Dis. 2009; 15:1385–1390.
Article34. Zhang J, Chen J, Gu J, Guo H, Chen W. Association of IL23R and ATG16L1 with susceptibility of Crohn’s disease in Chinese population. Scand J Gastroenterol. 2014; 49:1201–1206.
Article35. Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005; 19 Suppl A:5A–36A.
Article36. Honap S, Meade S, Ibraheim H, Irving PM, Jones MP, Samaan MA. Effectiveness and safety of ustekinumab in inflammatory bowel disease: a systematic review and meta-analysis. Dig Dis Sci. 2022; 67:1018–1035.
Article37. Hibi T, Imai Y, Murata Y, Matsushima N, Zheng R, Gasink C. Efficacy and safety of ustekinumab in Japanese patients with moderately to severely active Crohn’s disease: a subpopulation analysis of phase 3 induction and maintenance studies. Intest Res. 2017; 15:475–486.
Article38. Greenup AJ, Rosenfeld G, Bressler B. Ustekinumab use in Crohn’s disease: a Canadian tertiary care centre experience. Scand J Gastroenterol. 2017; 52:1354–1359.
Article39. Verstockt B, Dreesen E, Noman M, et al. Ustekinumab exposure-outcome analysis in Crohn’s disease only in part explains limited endoscopic remission rates. J Crohns Colitis. 2019; 13:864–872.
Article40. Lorenzo González L, Valdés Delgado T, Vázquez Morón JM, et al. Ustekinumab in Crohn’s disease: real-world outcomes and predictors of response. Rev Esp Enferm Dig. 2022; 114:272–279.
Article41. Monin L, Dubois S, Reenaers C, et al. Ustekinumab in bio-naïve and bio-failure Crohn’s disease patients: Results from a « real-life » monocentric cohort. Dig Liver Dis. 2021; 53:72–78.
Article42. Forss A, Clements M, Myrelid P, et al. Prospective observational study on Stelara (ustekinumab) assessing effectiveness in Crohn’s disease (PROSE): a 16-week follow-up. Scand J Gastroenterol. 2021; 56:680–686.
Article43. Harris RJ, McDonnell M, Young D, et al. Early real-world effectiveness of ustekinumab for Crohn’s disease. Frontline Gastroenterol. 2019; 11:111–116.
Article44. Loly C, Belaiche J, Louis E. Predictors of severe Crohn’s disease. Scand J Gastroenterol. 2008; 43:948–954.
Article45. Agrawal M, Spencer EA, Colombel JF, Ungaro RC. Approach to the management of recently diagnosed inflammatory bowel disease patients: a user’s guide for adult and pediatric gastroenterologists. Gastroenterology. 2021; 161:47–65.
Article46. Wong EC, Marshall JK, Reinisch W, Narula N. Body mass index does not impact clinical efficacy of ustekinumab in Crohn’s disease: a post hoc analysis of the IM-UNITI Trial. Inflamm Bowel Dis. 2021; 27:848–854.
Article47. Gisbert JP, Chaparro M. Predictors of primary response to biologic treatment [anti-TNF, vedolizumab, and ustekinumab] in patients with inflammatory bowel disease: from basic science to clinical practice. J Crohns Colitis. 2020; 14:694–709.
Article48. Dulai P, Guizzetti L, Ma T, et al. Clinical prediction model and decision support tool for ustekinumab in Crohn’s disease. Am J Gastroenterol. 2019; 114:S373.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrigendum: Real-world effectiveness and safety of ustekinumab induction therapy for Korean patients with Crohn’s disease: a KASID prospective multicenter study
- The Phase 3 Trials of Ustekinumab as Induction and Maintenance Therapy for Crohn's Disease
- Efficacy and safety of ustekinumab in Japanese patients with moderately to severely active Crohn's disease: a subpopulation analysis of phase 3 induction and maintenance studies
- Ustekinumab is effective in biological refractory Crohn's disease patients–regardless of approval study selection criteria
- Long-term safety and effectiveness of adalimumab in Japanese patients with Crohn’s disease: 3-year results from a real-world study