Clin Endosc.
2023 Jan;56(1):23-37. 10.5946/ce.2022.139.
Submucosal endoscopy: the present and future
- Affiliations
-
- 1Asian Institute of Gastroenterology, Hyderabad, India
- KMID: 2538748
- DOI: http://doi.org/10.5946/ce.2022.139
Abstract
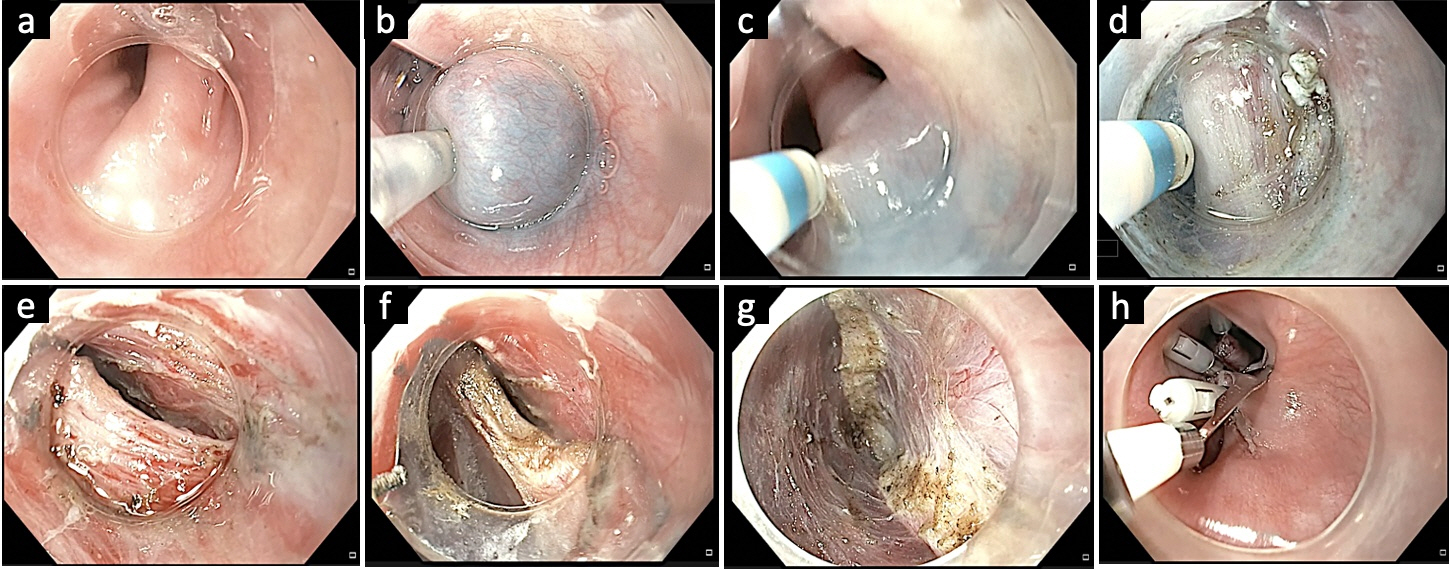
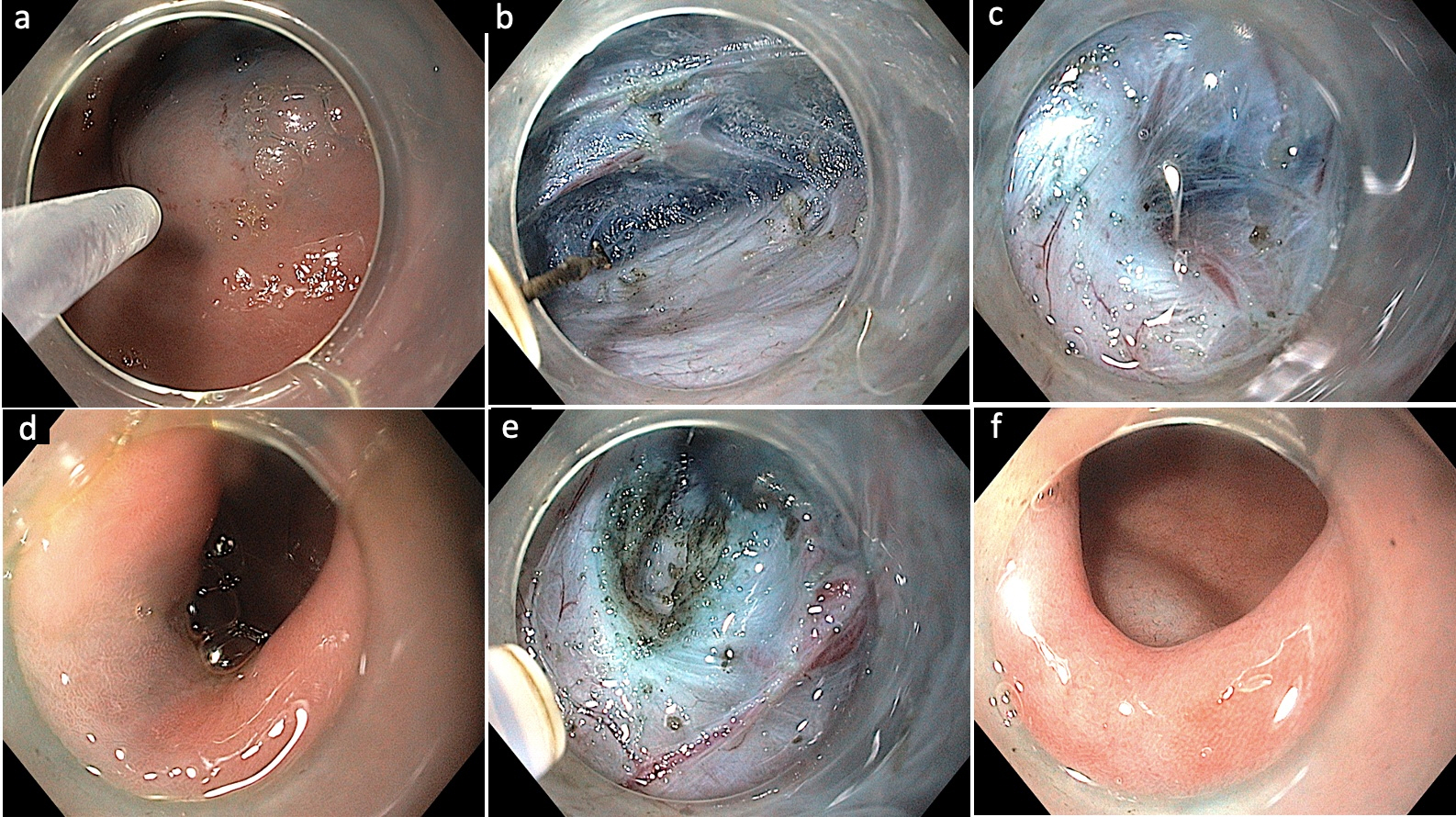
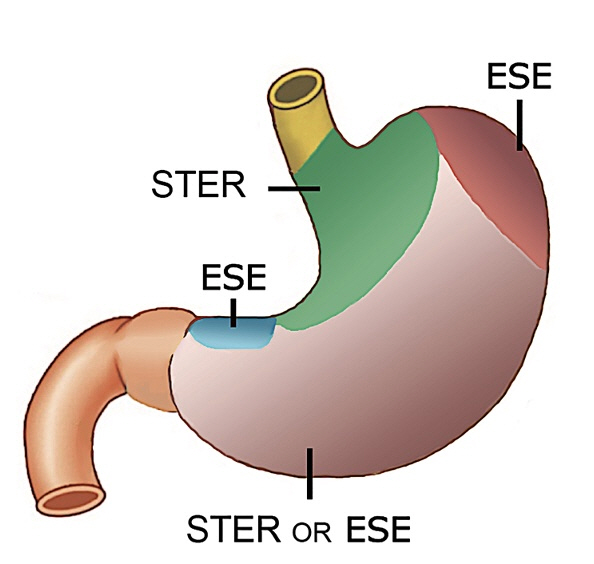
- Submucosal endoscopy or third-space endoscopy utilizes the potential space between the mucosal and muscularis layers of the gastrointestinal tract to execute therapeutic interventions for various diseases. Over the last decade, endoscopic access to the submucosal space has revolutionized the field of therapeutic endoscopy. Submucosal endoscopy was originally used to perform endoscopic myotomy in patients with achalasia cardia, and its use has grown exponentially since. Currently, submucosal endoscopy is widely used to resect subepithelial tumors and to manage refractory gastroparesis and Zenker’s diverticulum. While the utility of submucosal endoscopy has stood the test of time in esophageal motility disorders and subepithelial tumors, its durability remains to be established in conditions such as Zenker’s diverticulum and refractory gastroparesis. Other emerging indications for submucosal endoscopy include esophageal epiphrenic diverticulum, Hirschsprung’s disease, and esophageal strictures not amenable to conventional endoscopic treatment. The potential of submucosal endoscopy to provide easy and safe access to the mediastinum and peritoneal spaces may open doors to novel indications and rejuvenate the interest of endoscopists in natural orifice transluminal endoscopic surgery in the future. This review focuses on the current spectrum, recent updates, and future direction of submucosal endoscopy in the gastrointestinal tract.
Figure
Cited by 1 articles
-
Prevalence, natural progression, and clinical practices of upper gastrointestinal subepithelial lesions in Korea: a multicenter study
Younghee Choe, Yu Kyung Cho, Gwang Ha Kim, Jun-Ho Choi, Eun Soo Kim, Ji Hyun Kim, Eun Kwang Choi, Tae Hyeon Kim, Seong-Hun Kim, Do Hoon Kim
Clin Endosc. 2023;56(6):744-753. doi: 10.5946/ce.2023.005.
Reference
-
1. Sumiyama K, Gostout CJ, Rajan E, et al. Transesophageal mediastinoscopy by submucosal endoscopy with mucosal flap safety valve technique. Gastrointest Endosc. 2007; 65:679–683.2. Sumiyama K, Gostout CJ, Rajan E, et al. Submucosal endoscopy with mucosal flap safety valve. Gastrointest Endosc. 2007; 65:688–694.3. Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007; 39:761–764.4. Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010; 42:265–271.5. Nabi Z, Reddy DN. Third space endoscopy: the future of treating gastrointestinal dysmotility. Curr Opin Gastroenterol. 2021; 37:462–469.6. Werner YB, von Renteln D, Noder T, et al. Early adverse events of per-oral endoscopic myotomy. Gastrointest Endosc. 2017; 85:708–718.7. Nabi Z, Reddy DN, Ramchandani M. Adverse events during and after per-oral endoscopic myotomy: prevention, diagnosis, and management. Gastrointest Endosc. 2018; 87:4–17.8. Haito-Chavez Y, Inoue H, Beard KW, et al. Comprehensive analysis of adverse events associated with per oral endoscopic myotomy in 1826 patients: an international multicenter study. Am J Gastroenterol. 2017; 112:1267–1276.9. Nabi Nabi, Talukdar R, Beard R, et al. Outcomes of per-oral endoscopic myotomy in children: a systematic review and meta-analysis. Dysphagia. 2022; 37:1468–1481.10. Zhong C, Huang S, Xia H, et al. Role of peroral endoscopic myotomy in geriatric patients with achalasia: a systematic review and meta-analysis. Dig Dis. 2022; 40:106–114.11. Khan MA, Kumbhari V, Ngamruengphong S, et al. Is POEM the answer for management of spastic esophageal disorders? A systematic review and meta-analysis. Dig Dis Sci. 2017; 62:35–44.12. Nabi Z, Ramchandani M, Chavan R, et al. Peroral endoscopic myotomy in treatment-naïve achalasia patients versus prior treatment failure cases. Endoscopy. 2018; 50:358–370.13. Nabi Z, Ramchandani M, Basha J, et al. Outcomes of per-oral endoscopic myotomy in sigmoid and advanced sigmoid achalasia. J Gastrointest Surg. 2021; 25:530–532.14. Guo H, Yang H, Zhang X, et al. Long-term outcomes of peroral endoscopic myotomy for patients with achalasia: a retrospective single-center study. Dis Esophagus. 2017; 30:1–6.15. Hernández Mondragón OV, González Martinez MA, Blancas Valencia JM, et al. Long-term quality of life after peroral endoscopic myotomy remains compromised in patients with achalasia type III. Endoscopy. 2017; 49:1209–1218.16. Teitelbaum EN, Dunst CM, Reavis KM, et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc. 2018; 32:421–427.17. Liu XY, Cheng J, Chen WF, et al. A risk-scoring system to predict clinical failure for patients with achalasia after peroral endoscopic myotomy. Gastrointest Endosc. 2020; 91:33–40.18. Brewer Gutierrez OI, Moran RA, Familiari P, et al. Long-term outcomes of per-oral endoscopic myotomy in achalasia patients with a minimum follow-up of 4 years: a multicenter study. Endosc Int Open. 2020; 8:E650–E655.19. Filicori F, Dunst CM, Sharata A, et al. Long-term outcomes following POEM for non-achalasia motility disorders of the esophagus. Surg Endosc. 2019; 33:1632–1639.20. He C, Li M, Lu B, et al. Long-term efficacy of peroral endoscopic myotomy for patients with achalasia: outcomes with a median follow-up of 36 months. Dig Dis Sci. 2019; 64:803–810.21. Podboy AJ, Hwang JH, Rivas H, et al. Long-term outcomes of per-oral endoscopic myotomy compared to laparoscopic Heller myotomy for achalasia: a single-center experience. Surg Endosc. 2021; 35:792–801.22. Tefas C, Boroș C, Ciobanu L, et al. POEM: five years of experience in a single east European center. J Gastrointestin Liver Dis. 2020; 29:323–328.23. Nabi Z, Chavan R, Ramchandani M, et al. Long-term outcomes of per-oral endoscopic myotomy in spastic esophageal motility disorders: a large, single-center study. J Clin Gastroenterol. 2021; 55:594–601.24. Onimaru M, Inoue H, Fujiyoshi Y, et al. Long-term clinical results of per-oral endoscopic myotomy (POEM) for achalasia: first report of more than 10-year patient experience as assessed with a questionnaire-based survey. Endosc Int Open. 2021; 9:E409–E416.25. McKay SC, Dunst CM, Sharata AM, et al. POEM: clinical outcomes beyond 5 years. Surg Endosc. 2021; 35:5709–5716.26. Modayil RJ, Zhang X, Rothberg B, et al. Peroral endoscopic myotomy: 10-year outcomes from a large, single-center U.S. series with high follow-up completion and comprehensive analysis of long-term efficacy, safety, objective GERD, and endoscopic functional luminal assessment. Gastrointest Endosc. 2021; 94:930–942.27. Campagna RA, Cirera A, Holmstrom AL, et al. Outcomes of 100 patients more than 4 years after POEM for achalasia. Ann Surg. 2021; 273:1135–1140.28. Sanaka MR, Chadalavada P, Covut F, et al. Clinical success and correlation of Eckardt scores with barium esophagram after peroral endoscopic myotomy in achalasia. J Gastrointest Surg. 2021; 25:278–281.29. Xu S, Chai N, Tang X, et al. Outcomes of peroral endoscopic myotomy in challenging achalasia patients: a long-term follow-up study. Surg Endosc. 2021; 35:3732–3743.30. Andolfi C, Fisichella PM. Meta-analysis of clinical outcome after treatment for achalasia based on manometric subtypes. Br J Surg. 2019; 106:332–341.31. Ponds FA, Fockens P, Lei A, et al. Effect of peroral endoscopic myotomy vs pneumatic dilation on symptom severity and treatment outcomes among treatment-naïve patients with achalasia: a randomized clinical trial. JAMA. 2019; 322:134–144.32. Werner YB, Hakanson B, Martinek J, et al. Endoscopic or surgical myotomy in patients with idiopathic achalasia. N Engl J Med. 2019; 381:2219–2229.33. Jung HK, Hong SJ, Lee OY, et al. 2019 Seoul consensus on esophageal achalasia guidelines. J Neurogastroenterol Motil. 2020; 26:180–203.34. Khashab MA, Vela MF, Thosani N, et al. ASGE guideline on the management of achalasia. Gastrointest Endosc. 2020; 91:213–227.35. Oude Nijhuis RA, Zaninotto G, Roman S, et al. European guidelines on achalasia: United European Gastroenterology and European Society of Neurogastroenterology and Motility recommendations. United European Gastroenterol J. 2020; 8:13–33.36. Vaezi MF, Pandolfino JE, Yadlapati RH, et al. ACG clinical guidelines: diagnosis and management of achalasia. Am J Gastroenterol. 2020; 115:1393–1411.37. Weusten BL, Barret M, Bredenoord AJ, et al. Endoscopic management of gastrointestinal motility disorders - part 1: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2020; 52:498–515.38. Repici A, Cappello A, Spadaccini M, et al. Cap-assisted endoscopic septotomy of Zenker's diverticulum: early and long-term outcomes. Am J Gastroenterol. 2021; 116:1853–1858.39. Costamagna G, Iacopini F, Bizzotto A, et al. Prognostic variables for the clinical success of flexible endoscopic septotomy of Zenker's diverticulum. Gastrointest Endosc. 2016; 83:765–773.40. Huberty V, El Bacha S, Blero D, et al. Endoscopic treatment for Zenker's diverticulum: long-term results (with video). Gastrointest Endosc. 2013; 77:701–707.41. Zhang LY, Nieto J, Ngamruengphong S, et al. Zenker's diverticulum: advancing beyond the tunnel. VideoGIE. 2021; 6:562–567.42. Repici A, Spadaccini M, Belletrutti PJ, et al. Peroral endoscopic septotomy for short-septum Zenker's diverticulum. Endoscopy. 2020; 52:563–568.43. Yang J, Novak S, Ujiki M, et al. An international study on the use of peroral endoscopic myotomy in the management of Zenker's diverticulum. Gastrointest Endosc. 2020; 91:163–168.44. Budnicka A, Januszewicz W, Białek AB, et al. Peroral endoscopic myotomy in the management of Zenker's diverticulum: a retrospective multicenter study. J Clin Med. 2021; 10:187.45. Elkholy S, El-Sherbiny M, Delano-Alonso R, et al. Peroral endoscopic myotomy as treatment for Zenker's diverticulum (Z-POEM): a multi-center international study. Esophagus. 2021; 18:693–699.46. Sanaei O, Ichkhanian Y, Mondragón OV, et al. Impact of prior treatment on feasibility and outcomes of Zenker's peroral endoscopic myotomy (Z-POEM). Endoscopy. 2021; 53:722–726.47. Mittal C, Diehl DL, Draganov PV, et al. Practice patterns, techniques, and outcomes of flexible endoscopic myotomy for Zenker's diverticulum: a retrospective multicenter study. Endoscopy. 2021; 53:346–353.48. Al Ghamdi SS, Farha J, Moran RA, et al. Zenker's peroral endoscopic myotomy, or flexible or rigid septotomy for Zenker's diverticulum: a multicenter retrospective comparison. Endoscopy. 2022; 54:345–351.49. Kahaleh M, Mahpour NY, Tyberg A, et al. Per oral endoscopic myotomy for Zenker's diverticulum: a novel and superior technique compared with septotomy? J Clin Gastroenterol. 2022; 56:224–227.50. Yang J, Zeng X, Yuan X, et al. An international study on the use of peroral endoscopic myotomy (POEM) in the management of esophageal diverticula: the first multicenter D-POEM experience. Endoscopy. 2019; 51:346–349.51. Basile P, Gonzalez JM, Le Mouel JP, et al. Per-oral endoscopic myotomy with septotomy for the treatment of distal esophageal diverticula (D-POEM). Surg Endosc. 2020; 34:2321–2325.52. Nabi Z, Chavan R, Asif S, et al. Per-oral endoscopic myotomy with division of septum (D-POEM) in epiphrenic esophageal diverticula: outcomes at a median follow-up of two years. Dysphagia. 2022; 37:839–847.53. Demeter M, Ďuriček M, Vorčák M, et al. S-POEM in treatment of achalasia and esophageal epiphrenic diverticula - single center experience. Scand J Gastroenterol. 2020; 55:509–514.54. Kinoshita M, Tanaka S, Kawara F, et al. Peroral endoscopic myotomy alone is effective for esophageal motility disorders and esophageal epiphrenic diverticulum: a retrospective single-center study. Surg Endosc. 2020; 34:5447–5454.55. Samanta J, Nabi Z, Dhar J, et al. Peroral endoscopic myotomy (POEM) for esophageal diverticula. Minerva Gastroenterol (Torino). 2021; Sep. 13. [Epub]. https://doi.org/10.23736/S2724-5985.21.02984-3.56. Wagh MS, Yang D, Chavalitdhamrong D, et al. Per-oral endoscopic tunneling for restoration of the esophagus (POETRE). Gastrointest Endosc. 2014; 80:330.57. Wagh MS, Draganov PV. Per-oral endoscopic tunneling for restoration of the esophagus: a novel endoscopic submucosal dissection technique for therapy of complete esophageal obstruction. Gastrointest Endosc. 2017; 85:722–727.58. Félix C, Barreiro P, Rodrigues Azevedo J, et al. Per-oral endoscopic tunneling for restoration of the esophagus (POETRE) in the management of a complete esophageal obstruction. Endosc Int Open. 2021; 9:E1084–E1085.59. Toro JP, Lytle NW, Patel AD, et al. Efficacy of laparoscopic pyloroplasty for the treatment of gastroparesis. J Am Coll Surg. 2014; 218:652–660.60. Shada AL, Dunst CM, Pescarus R, et al. Laparoscopic pyloroplasty is a safe and effective first-line surgical therapy for refractory gastroparesis. Surg Endosc. 2016; 30:1326–1332.61. Brown AM, Pryor AD, Docimo S Jr. Per oral pyloromyotomy utilizing a lesser curvature approach: how we do it. Surg Endosc. 2020; 34:5168–5171.62. Abdelfatah MM, Li B, Kapil N, et al. Short-term outcomes of double versus single pyloromyotomy at peroral endoscopic pyloromyotomy in the treatment of gastroparesis (with video). Gastrointest Endosc. 2020; 92:603–609.63. Ichkhanian Y, Vosoughi K, Aghaie Meybodi M, et al. Comprehensive analysis of adverse events associated with gastric peroral endoscopic myotomy: an international multicenter study. Surg Endosc. 2021; 35:1755–1764.64. Mekaroonkamol P, Patel V, Shah R, et al. Association between duration or etiology of gastroparesis and clinical response after gastric per-oral endoscopic pyloromyotomy. Gastrointest Endosc. 2019; 89:969–976.65. Gregor L, Wo J, DeWitt J, et al. Gastric peroral endoscopic myotomy for the treatment of refractory gastroparesis: a prospective single-center experience with mid-term follow-up (with video). Gastrointest Endosc. 2021; 94:35–44.66. Abdelfatah MM, Noll A, Kapil N, et al. Long-term outcome of gastric per-oral endoscopic pyloromyotomy in treatment of gastroparesis. Clin Gastroenterol Hepatol. 2021; 19:816–824.67. Ragi O, Jacques J, Branche J, et al. One-year results of gastric peroral endoscopic myotomy for refractory gastroparesis: a French multicenter study. Endoscopy. 2021; 53:480–490.68. Vosoughi K, Ichkhanian Y, Benias P, et al. Gastric per-oral endoscopic myotomy (G-POEM) for refractory gastroparesis: results from an international prospective trial. Gut. 2022; 71:25–33.69. Labonde A, Lades G, Debourdeau A, et al. Gastric peroral endoscopic myotomy in refractory gastroparesis: long-term outcomes and predictive score to improve patient selection. Gastrointest Endosc. 2022; 96:500–508.70. Spadaccini M, Maselli R, Chandrasekar VT, et al. Gastric peroral endoscopic pyloromyotomy for refractory gastroparesis: a systematic review of early outcomes with pooled analysis. Gastrointest Endosc. 2020; 91:746–752.71. Pioppo L, Reja D, Gaidhane M, et al. Gastric per-oral endoscopic myotomy versus pyloromyotomy for gastroparesis: an international comparative study. J Gastroenterol Hepatol. 2021; 36:3177–3182.72. Mohan BP, Chandan S, Jha LK, et al. Clinical efficacy of gastric per-oral endoscopic myotomy (G-POEM) in the treatment of refractory gastroparesis and predictors of outcomes: a systematic review and meta-analysis using surgical pyloroplasty as a comparator group. Surg Endosc. 2020; 34:3352–3367.73. Shen S, Luo H, Vachaparambil C, et al. Gastric peroral endoscopic pyloromyotomy versus gastric electrical stimulation in the treatment of refractory gastroparesis: a propensity score-matched analysis of long term outcomes. Endoscopy. 2020; 52:349–358.74. Lv XH, Wang CH, Xie Y. Efficacy and safety of submucosal tunneling endoscopic resection for upper gastrointestinal submucosal tumors: a systematic review and meta-analysis. Surg Endosc. 2017; 31:49–63.75. Chen Y, Wang M, Zhao L, et al. The retrospective comparison between submucosal tunneling endoscopic resection and endoscopic submucosal excavation for managing esophageal submucosal tumors originating from the muscularis propria layer. Surg Endosc. 2020; 34:417–428.76. Ponte Neto FL, de Moura DT, Sagae VM, et al. Endoscopic resection of esophageal and gastric submucosal tumors from the muscularis propria layer: submucosal tunneling endoscopic resection versus endoscopic submucosal excavation: a systematic review and meta-analysis. Surg Endosc. 2021; 35:6413–6426.77. Lu J, Jiao T, Li Y, et al. Heading toward the right direction: solution package for endoscopic submucosal tunneling resection in the stomach. PLoS One. 2015; 10:e0119870.78. Tan Y, Lv L, Duan T, et al. Comparison between submucosal tunneling endoscopic resection and video-assisted thoracoscopic surgery for large esophageal leiomyoma originating from the muscularis propria layer. Surg Endosc. 2016; 30:3121–3127.79. Chai N, Du C, Gao Y, et al. Comparison between submucosal tunneling endoscopic resection and video-assisted thoracoscopic enucleation for esophageal submucosal tumors originating from the muscularis propria layer: a randomized controlled trial. Surg Endosc. 2018; 32:3364–3372.80. Onimaru M, Inoue H, Bechara R, et al. Clinical outcomes of per-oral endoscopic tumor resection for submucosal tumors in the esophagus and gastric cardia. Dig Endosc. 2020; 32:328–336.81. Bapaye A, Dashatwar P, Biradar V, et al. Initial experience with per-rectal endoscopic myotomy for Hirschsprung's disease: medium and long term outcomes of the first case series of a novel third-space endoscopy procedure. Endoscopy. 2021; 53:1256–1260.82. Nabi Z, Shava U, Sekharan A, et al. Diagnosis of Hirschsprung's disease in children: preliminary evaluation of a novel endoscopic technique for rectal biopsy. JGH Open. 2018; 2:322–326.83. Nabi Z, Chavan R, Shava U, et al. A novel endoscopic technique to obtain rectal biopsy specimens in children with suspected Hirschsprung's disease. VideoGIE. 2018; 3:157–158.84. Li L, Chai N, Linghu E, et al. Safety and efficacy of using a short tunnel versus a standard tunnel for peroral endoscopic myotomy for ling type IIc and III achalasia: a retrospective study. Surg Endosc. 2019; 33:1394–1402.85. Huang S, Ren Y, Peng W, et al. Peroral endoscopic shorter versus longer myotomy for the treatment of achalasia: a comparative retrospective study. Esophagus. 2020; 17:477–483.86. Gu L, Ouyang Z, Lv L, et al. Safety and efficacy of peroral endoscopic myotomy with standard myotomy versus short myotomy for treatment-naïve patients with type II achalasia: a prospective randomized trial. Gastrointest Endosc. 2021; 93:1304–1312.87. Nabi Z, Ramchandani M, Sayyed M, et al. Comparison of short versus long esophageal myotomy in cases with idiopathic achalasia: a randomized controlled trial. J Neurogastroenterol Motil. 2021; 27:63–70.88. Repici A, Fuccio L, Maselli R, et al. GERD after per-oral endoscopic myotomy as compared with Heller's myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc. 2018; 87:934–943.89. Sanaka MR, Thota PN, Parikh MP, et al. Peroral endoscopic myotomy leads to higher rates of abnormal esophageal acid exposure than laparoscopic Heller myotomy in achalasia. Surg Endosc. 2019; 33:2284–2292.90. Karyampudi A, Nabi Z, Ramchandani M, et al. Gastroesophageal reflux after per-oral endoscopic myotomy is frequently asymptomatic, but leads to more severe esophagitis: a case-control study. United European Gastroenterol J. 2021; 9:63–71.91. Nabi Z, Ramchandani M, Kotla R, et al. Gastroesophageal reflux disease after peroral endoscopic myotomy is unpredictable, but responsive to proton pump inhibitor therapy: a large, single-center study. Endoscopy. 2020; 52:643–651.92. Nabi Z, Talukdar R, Mandavdhare H, et al. Short versus long esophageal myotomy during peroral endoscopic myotomy: a systematic review and meta-analysis of comparative trials. Saudi J Gastroenterol. 2022; 28:261–267.93. Knowles TB, Jackson AS, Chang SC, et al. Changes in distensibility index during an incremental POEM myotomy. J Gastrointest Surg. 2022; 26:1140–1146.94. Inoue H, Ueno A, Shimamura Y, et al. Peroral endoscopic myotomy and fundoplication: a novel NOTES procedure. Endoscopy. 2019; 51:161–164.95. Nabi Z, Ramchandani M, Reddy DN. Per-oral endoscopic myotomy and gastroesophageal reflux: where do we stand after a decade of "POETRY"? Indian J Gastroenterol. 2019; 38:287–294.96. Tanaka S, Toyonaga T, Kawara F, et al. Novel per-oral endoscopic myotomy method preserving oblique muscle using two penetrating vessels as anatomic landmarks reduces postoperative gastroesophageal reflux. J Gastroenterol Hepatol. 2019; 34:2158–2163.97. Nabi Z, Ramchandani M, Darisetty S, et al. Peroral endoscopic myotomy with endoscopic fundoplication in a patient with idiopathic achalasia. Endoscopy. 2020; 52:74–75.98. Tyberg A, Choi A, Gaidhane M, et al. Transoral incisional fundoplication for reflux after peroral endoscopic myotomy: a crucial addition to our arsenal. Endosc Int Open. 2018; 6:E549–E552.99. Su B, Callahan ZM, Novak S, et al. Using impedance planimetry (EndoFLIP) to evaluate myotomy and predict outcomes after surgery for achalasia. J Gastrointest Surg. 2020; 24:964–971.100. Vosoughi K, Ichkhanian Y, Jacques J, et al. Role of endoscopic functional luminal imaging probe in predicting the outcome of gastric peroral endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2020; 91:1289–1299.101. Chen T, Xu A, Lian J, et al. Transcolonic endoscopic appendectomy: a novel natural orifice transluminal endoscopic surgery (NOTES) technique for the sessile serrated lesions involving the appendiceal orifice. Gut. 2021; 70:1812–1814.102. Liu XY, Li QL, Xu XY, et al. Endoscopic transgastric cholecystectomy: a novel approach for minimally invasive cholecystectomy. Endoscopy. 2021; 53:E50–E51.103. Ikebuchi Y, Kanda T, Ikeda H, et al. Identification of human herpes virus 1 encoded microRNAs in biopsy samples of lower esophageal sphincter muscle during peroral endoscopic myotomy for esophageal achalasia. Dig Endosc. 2020; 32:136–142.104. Chen S, Zhang M, Liang M, et al. The number of interstitial cells of cajal differs among different subtypes of achalasia and is related to patients' prognosis. Clin Transl Gastroenterol. 2021; 12:e00388.105. Reddy CA, Law R, Appelman HD, et al. Per-oral endoscopic myotomy biopsies of achalasia patients reveal schwann cell depletion in the muscularis propria. Clin Gastroenterol Hepatol. 2021; 19:1294–1295.106. Chen H, Calderon LF, Shah R, et al. Simultaneous examination of eosinophil infiltration in esophageal mucosa and muscle in patients with achalasia: direct biopsy of the esophageal muscle at per-oral endoscopic myotomy. Dig Dis Sci. 2022; 67:170–176.107. Steele K, Schweitzer MA, Lyn-Sue J, et al. Flexible transgastric peritoneoscopy and liver biopsy: a feasibility study in human beings (with videos). Gastrointest Endosc. 2008; 68:61–66.108. Qin Z, Linghu EQ, Zhai YQ, et al. Endoscopic transesophageal biopsy in the posterior mediastinum using submucosal tunneling technology and novel homemade instruments. Hepatogastroenterology. 2014; 61:1601–1604.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Future Development of Endoscopic Accessories for Endoscopic Submucosal Dissection
- Comparisons of Gastric Endoscopy and Upper Gastrointestinal Series in The Submucosal Tumor
- Third space endoscopy: Current evidence and future development
- Past, Present, and Future of the Korea-Japan Joint Symposium on Gastrointestinal Endoscopy
- Introduction to Endoscopic Submucosal Surgery