Korean J Orthod.
2023 Jan;53(1):45-53. 10.4041/kjod22.098.
Comparative evaluation of shear bond strength of orthodontic brackets bonded to three-dimensionallyprinted and milled materials after surface treatment and artificial aging
- Affiliations
-
- 1Department of Oral Rehabilitation, The Maurice and Gabriela Goldschleger School of Dental Medicine, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
- 2The Maurice and Gabriela Goldschleger School of Dental Medicine, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
- 3Department of Orthodontics, The Maurice and Gabriela Goldschleger School of Dental Medicine, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
- KMID: 2538712
- DOI: http://doi.org/10.4041/kjod22.098
Abstract
Objective
This study aimed to evaluate the shear bond strength (SBS) of orthodontic brackets bonded to three-dimensionally (3D)-printed materials after various surface treatments and artificial aging compared with that bonded to computer-aided design/ computer-aided manufacturing (CAD-CAM) polymethyl methacrylate (PMMA)-milled materials.
Methods
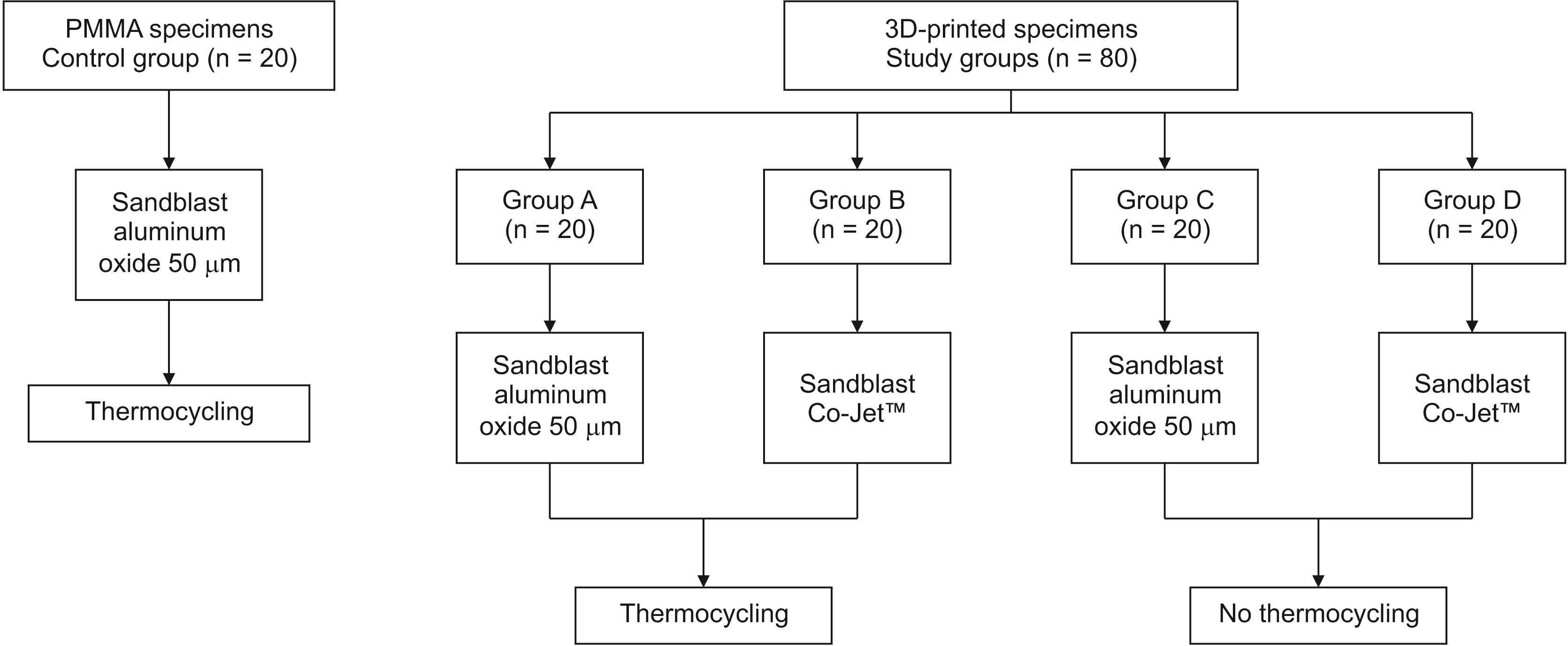
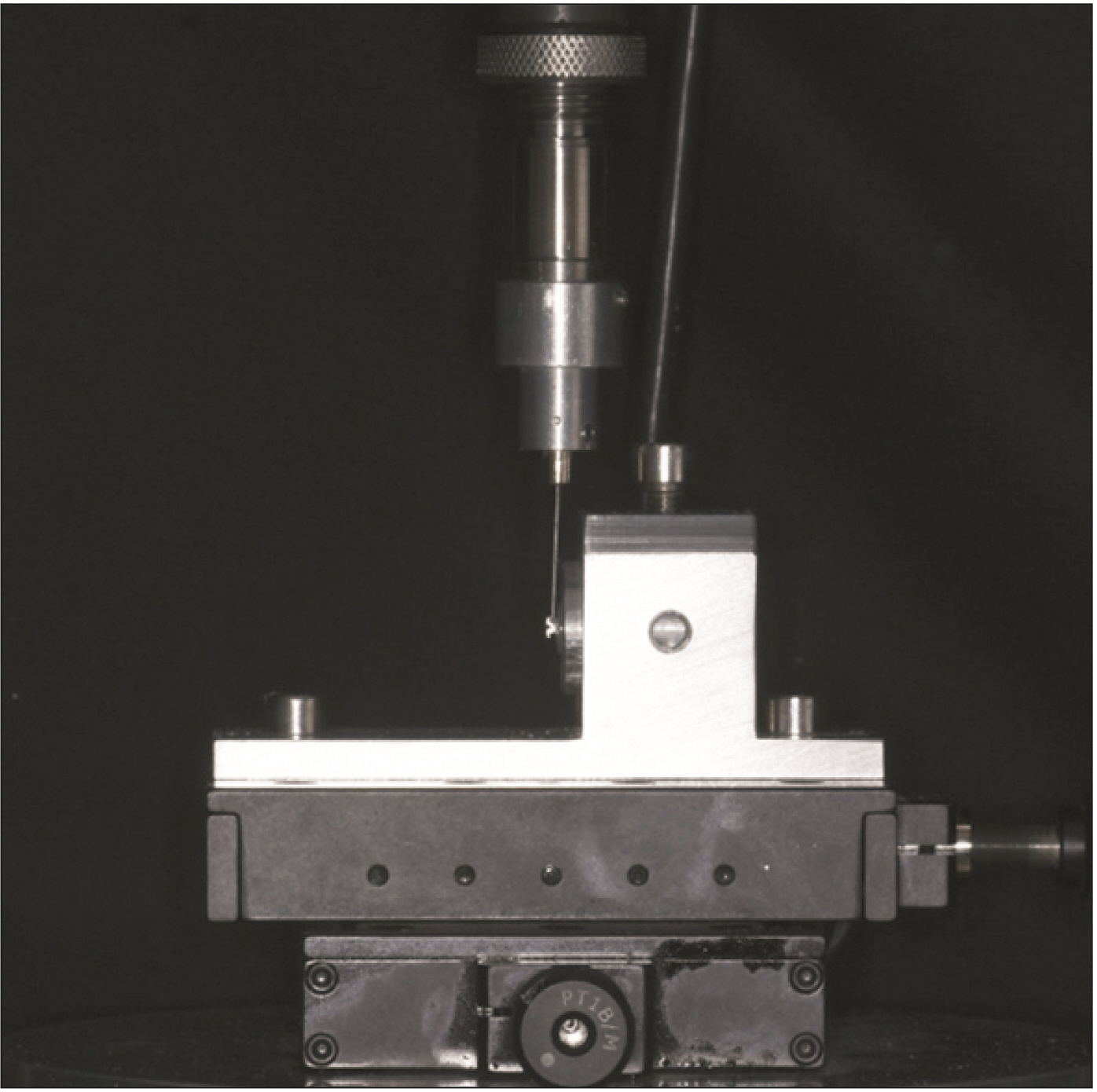
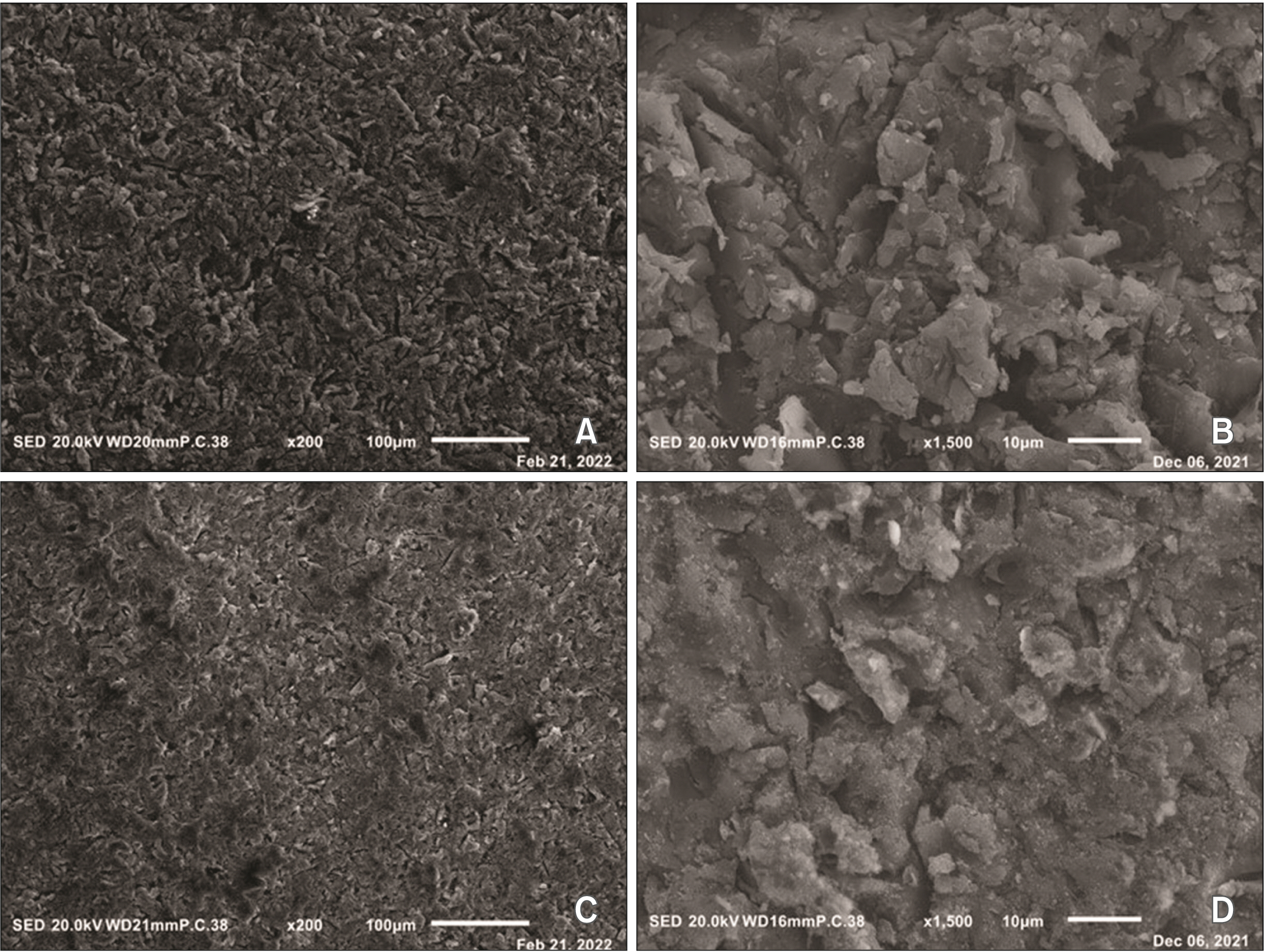
Eighty cylindrical specimens were 3D printed and divided into the following four subgroups (n = 20 each) according to the surface treatment and artificial aging procedure. Group A, sandblasted with 50 µm aluminum oxide particles (SA) and aging; group B, sandblasted with 30 µm silica-coated alumina particles (CO) and aging; group C, SA without aging; and group D, CO without aging. For the control group, 20 CAD-CAM PMMA-milled cylindrical specimens were sandblasted with SA and aged. The SBS was measured using a universal testing machine (0.25 mm/ min), examined at ×2.5 magnification for failure mode classification, and statistically analyzed (p = 0.05).
Results
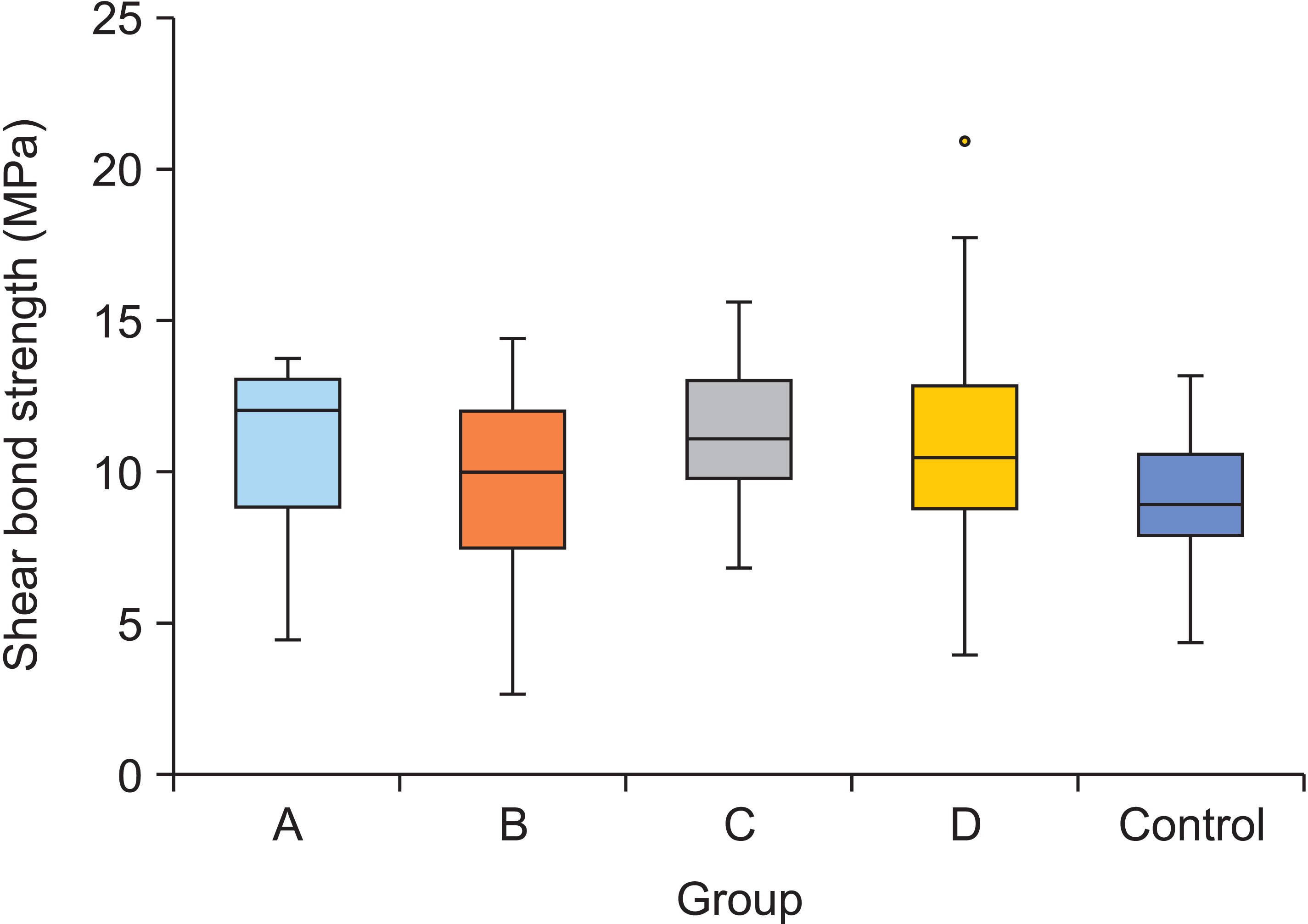
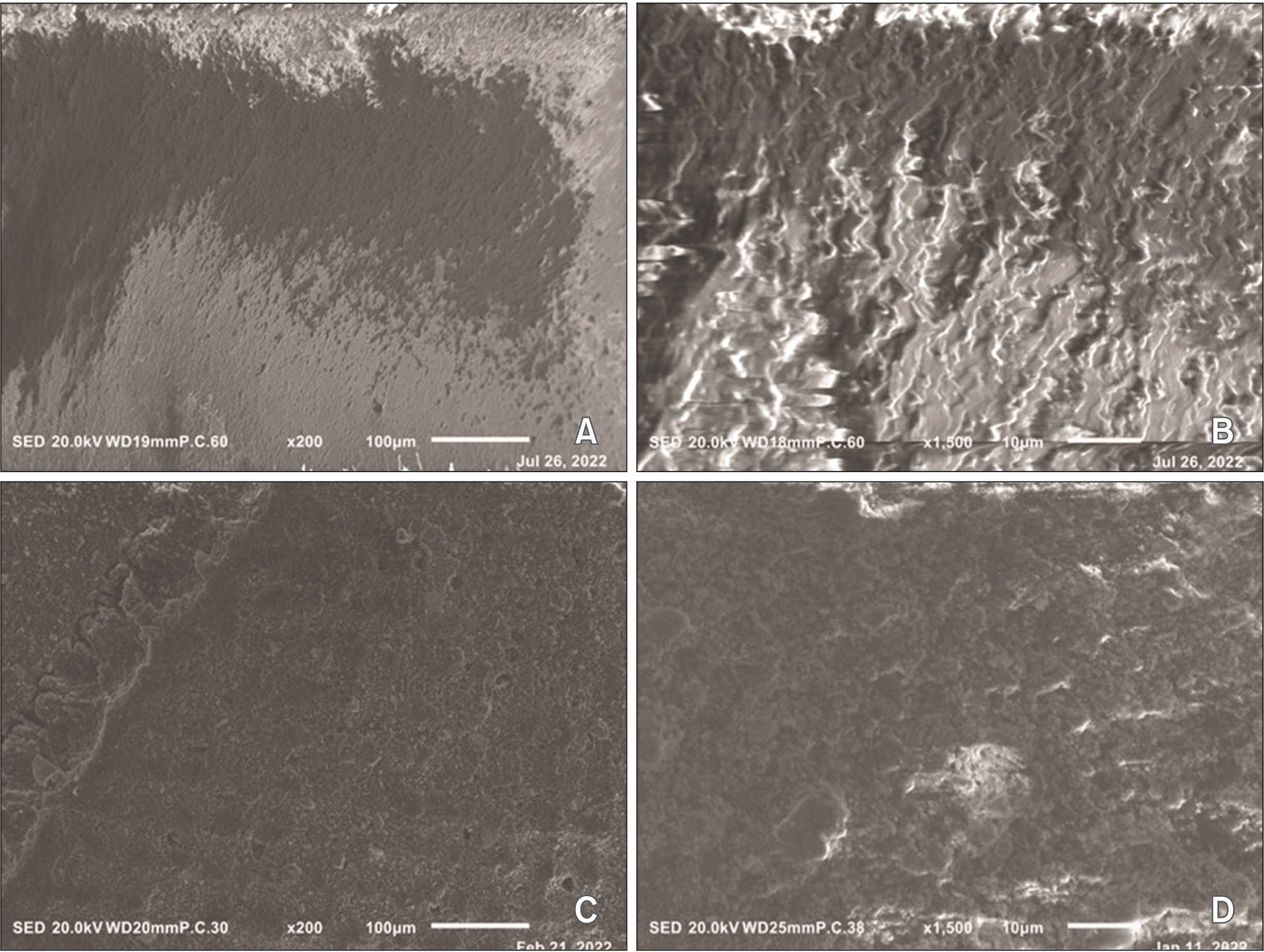
The retention obtained with the 3D-printed materials (groups A–D) was higher than that obtained with the PMMA-milled materials (control group). However, no significant difference was found between the study and control groups, except for group C (SA without aging), which showed significantly higher retention than the control group (PMMA-SA and thermocycling) (p = 0.037). Study groups A–D predominantly exhibited a cohesive specimen mode, indicating specimen fracture.
Conclusions
Orthodontic brackets bonded to 3D-printed materials exhibit acceptable bonding strengths. However, 3D-printed materials are prone to cohesive failure, which may result in crown fractures.
Keyword
Figure
Reference
-
1. Pabari S, Moles DR, Cunningham SJ. 2011; Assessment of motivation and psychological characteristics of adult orthodontic patients. Am J Orthod Dentofacial Orthop. 140:e263–72. DOI: 10.1016/j.ajodo.2011.06.022. PMID: 22133960.
Article2. Huser MC, Baehni PC, Lang R. 1990; Effects of orthodontic bands on microbiologic and clinical parameters. Am J Orthod Dentofacial Orthop. 97:213–8. DOI: 10.1016/S0889-5406(05)80054-X. PMID: 2309668.
Article3. Goracci C, Özcan M, Franchi L, Di Bello G, Louca C, Vichi A. 2019; Bracket bonding to polymethylmethacrylate-based materials for computer-aided design/manufacture of temporary restorations: influence of mechanical treatment and chemical treatment with universal adhesives. Korean J Orthod. 49:404–12. DOI: 10.4041/kjod.2019.49.6.404. PMID: 31815108. PMCID: PMC6883210.
Article4. Katreva I, Dikova T, Tonchev T. 2018; 3D Printing- an alternative of conventional crown fabrication: a case report. J IMAB. 24:2048–54. DOI: 10.5272/jimab.2018242.2048.5. Tahayeri A, Morgan M, Fugolin AP, Bompolaki D, Athirasala A, Pfeifer CS, et al. 2018; 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater. 34:192–200. DOI: 10.1016/j.dental.2017.10.003. PMID: 29110921. PMCID: PMC5801146.
Article6. Scotti CK, Velo MMAC, Rizzante FAP, Nascimento TRL, Mondelli RFL, Bombonatti JFS. 2020; Physical and surface properties of a 3D-printed composite resin for a digital workflow. J Prosthet Dent. 124:614.e1–614.e5. DOI: 10.1016/j.prosdent.2020.03.029. PMID: 32636072.
Article7. Hannig C, Laubach S, Hahn P, Attin T. 2006; Shear bond strength of repaired adhesive filling materials using different repair procedures. J Adhes Dent. 8:35–40. PMID: 16536343.8. Major PW, Koehler JR, Manning KE. 1995; 24-hour shear bond strength of metal orthodontic brackets bonded to porcelain using various adhesion promoters. Am J Orthod Dentofacial Orthop. 108:322–9. DOI: 10.1016/S0889-5406(95)70028-5. PMID: 7661151.
Article9. Newman GV, Newman RA, Sun BI, Ha JL, Ozsoylu SA. 1995; Adhesion promoters, their effect on the bond strength of metal brackets. Am J Orthod Dentofacial Orthop. 108:237–41. DOI: 10.1016/S0889-5406(95)70015-3. PMID: 7661138.
Article10. Gale MS, Darvell BW. 1999; Thermal cycling procedures for laboratory testing of dental restorations. J Dent. 27:89–99. DOI: 10.1016/S0300-5712(98)00037-2. PMID: 10071465.
Article11. Heller H, Arieli A, Beitlitum I, Pilo R, Levartovsky S. 2019; Load-bearing capacity of zirconia crowns screwed to multi-unit abutments with and without a titanium base: an in vitro pilot study. Materials (Basel). 12:3056. DOI: 10.3390/ma12193056. PMID: 31547045. PMCID: PMC6803877.
Article12. Elsaka SE. 2016; Influence of surface treatments on bond strength of metal and ceramic brackets to a novel CAD/CAM hybrid ceramic material. Odontology. 104:68–76. DOI: 10.1007/s10266-014-0188-8. PMID: 25585677.
Article13. Cozza P, Martucci L, De Toffol L, Penco SI. 2006; Shear bond strength of metal brackets on enamel. Angle Orthod. 76:851–6. DOI: 10.1043/0003-3219(2006)076[0851:SBSOMB]2.0.CO;2. PMID: 17029521.14. de Pulido LG, Powers JM. 1983; Bond strength of orthodontic direct-bonding cement-plastic bracket systems in vitro. Am J Orthod. 83:124–30. DOI: 10.1016/S0002-9416(83)90297-X. PMID: 6337499.
Article15. Özcan M, Pekkan G. 2013; Effect of different adhesion strategies on bond strength of resin composite to composite-dentin complex. Oper Dent. 38:63–72. DOI: 10.2341/11-482-L. PMID: 22812912.
Article16. Brosh T, Pilo R, Bichacho N, Blutstein R. 1997; Effect of combinations of surface treatments and bonding agents on the bond strength of repaired composites. J Prosthet Dent. 77:122–6. DOI: 10.1016/S0022-3913(97)70224-5. PMID: 9051597.
Article17. Cardoso RM, Godinho J, Jardim L. 2021; Bond strength of orthodontic brackets to polymethylmethacrylate: effect of the surface treatment and adhesive system. Rev Port Estomatol Med Dent Cir Maxilofac. 62:16–22. DOI: 10.24873/j.rpemd.2021.01.818.
Article18. Fox NA, McCabe JF, Buckley JG. 1994; A critique of bond strength testing in orthodontics. Br J Orthod. 21:33–43. DOI: 10.1179/bjo.21.1.33. PMID: 8199163.
Article19. Oesterle LJ, Shellhart WC. 2008; Effect of aging on the shear bond strength of orthodontic brackets. Am J Orthod Dentofacial Orthop. 133:716–20. DOI: 10.1016/j.ajodo.2006.04.042. PMID: 18456145.
Article20. Al Jabbari YS, Al Taweel SM, Al Rifaiy M, Alqahtani MQ, Koutsoukis T, Zinelis S. 2014; Effects of surface treatment and artificial aging on the shear bond strength of orthodontic brackets bonded to four different provisional restorations. Angle Orthod. 84:649–55. DOI: 10.2319/090313-649.1. PMID: 24446920. PMCID: PMC8650449.
Article21. Chay SH, Wong SL, Mohamed N, Chia A, Yap AU. 2007; Effects of surface treatment and aging on the bond strength of orthodontic brackets to provisional materials. Am J Orthod Dentofacial Orthop. 132:577.e7–11. DOI: 10.1016/j.ajodo.2004.01.024. PMID: 18005828.
Article22. Klocke A, Kahl-Nieke B. 2005; Influence of cross-head speed in orthodontic bond strength testing. Dent Mater. 21:139–44. DOI: 10.1016/j.dental.2004.03.004. PMID: 15681012.
Article23. Blakey R, Mah J. 2010; Effects of surface conditioning on the shear bond strength of orthodontic brackets bonded to temporary polycarbonate crowns. Am J Orthod Dentofacial Orthop. 138:72–8. DOI: 10.1016/j.ajodo.2008.08.030. PMID: 20620836.
Article24. Albahri R, Yoon HI, Lee JD, Yoon S, Lee SJ. 2021; Shear bond strength of provisional repair materials bonded to 3D printed resin. J Dent Sci. 16:261–7. DOI: 10.1016/j.jds.2020.05.003. PMID: 33384807. PMCID: PMC7770250.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The shear bond strength of two adhesives bonded to composite resin and glass ionomer cement restorations
- Shear bond strength of orthodontic adhesive to amalgam surface using light-cured resin
- Shear bond strength of metal brackets bonded with light-cured adhesive: an in vitro comparative study
- Effect of applying adhesive after enamel etching on the shear bond strength of orthodontic brackets using light curing resin cements
- A comparative study of bond strength of recycled brackets