Lab Med Online.
2022 Oct;12(4):235-243. 10.47429/lmo.2022.12.4.235.
Clinical Application of Circulating Tumor DNA Analysis
- Affiliations
-
- 1Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2538611
- DOI: http://doi.org/10.47429/lmo.2022.12.4.235
Abstract
- Liquid biopsy using circulating tumor DNA helps overcome the limitations of conventional tissue testing. Non-invasive molecular profiling using circulating tumor DNA is increasingly being used to diagnose cancer, stratify risk, and select targeted treatments. By understanding the biological characteristics of circulating tumor DNA and patient factors that can affect concentrations of circulating tumor DNA as well as optimizing the techniques, the clinical utilization of circulating tumor DNA tests can be improved. It is also necessary to formulate guidelines for the administration and reporting of circulating tumor DNA tests.
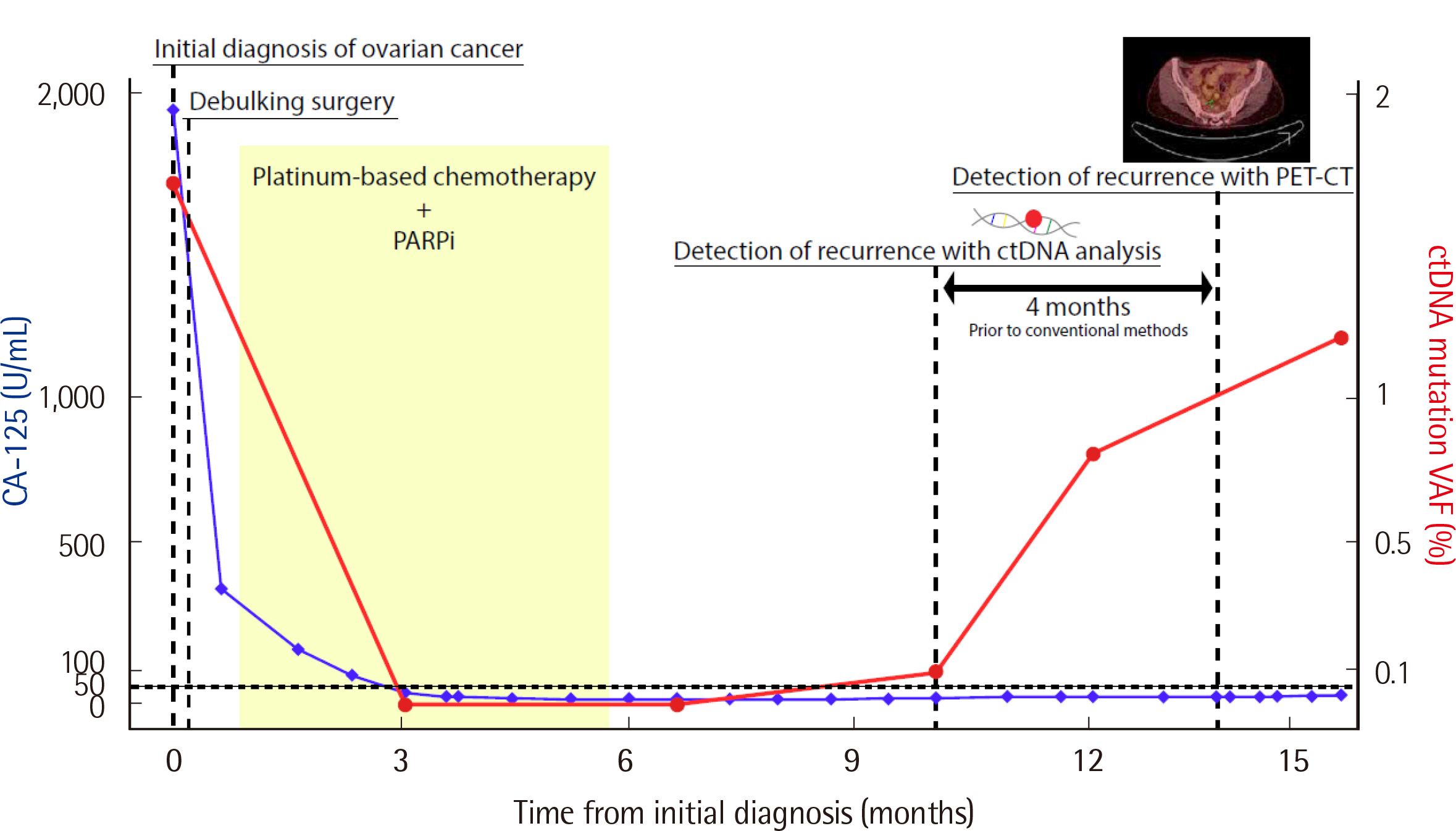
Figure
Reference
-
1. Mandel P, Metais P. 1948; Nuclear acids in human blood plasma. C R Seances Soc Biol Fil. 142:241–3.2. Leon SA, Shapiro B, Sklaroff DM, Yaros MJ. 1977; Free DNA in the serum of cancer patients and the effect of therapy. Cancer Res. 37:646–50.3. Siravegna G, Mussolin B, Buscarino M, Corti G, Cassingena A, Crisafulli G, et al. 2015; Clonal evolution and resistance to EGFR blockade in the blood of colorectal cancer patients. Nat Med. 21:795–801. DOI: 10.1038/nm.3870. PMID: 26030179. PMCID: PMC4868598.
Article4. Ulz P, Belic J, Graf R, Auer M, Lafer I, Fischereder K, et al. 2016; Whole-genome plasma sequencing reveals focal amplifications as a driving force in metastatic prostate cancer. Nat Commun. 7:12008. DOI: 10.1038/ncomms12008. PMID: 27328849. PMCID: PMC4917969.
Article5. De Mattos-Arruda L, Weigelt B, Cortes J, Won HH, Ng CKY, Nuciforo P, et al. 2014; Capturing intra-tumor genetic heterogeneity by de novo mutation profiling of circulating cell-free tumor DNA: a proof-of-principle. Ann Oncol. 25:1729–35. DOI: 10.1093/annonc/mdu239. PMID: 25009010. PMCID: PMC6276937.
Article6. Andersson D, Kristiansson H, Kubista M, Ståhlberg A. 2021; Ultrasensitive circulating tumor DNA analysis enables precision medicine: experimental workflow considerations. Expert Rev Mol Diagn. 21:299–310. DOI: 10.1080/14737159.2021.1889371. PMID: 33683971.
Article7. Galarza Fortuna GM, Dvir K. 2020; Circulating tumor DNA: Where are we now? A mini review of the literature. World J Clin Oncol. 11:723–31. DOI: 10.5306/wjco.v11.i9.723. PMID: 33033694. PMCID: PMC7522544.
Article8. Heitzer E, Ulz P, Geigl JB. 2015; Circulating tumor DNA as a liquid biopsy for cancer. Clin Chem. 61:112–23. DOI: 10.1373/clinchem.2014.222679. PMID: 25388429.
Article9. Lin C, Liu X, Zheng B, Ke R, Tzeng CM. 2021; Liquid biopsy, ctDNA diagnosis through NGS. Life (Basel). 11:890. DOI: 10.3390/life11090890. PMID: 34575039. PMCID: PMC8468354.
Article10. Wan JCM, Massie C, Garcia-Corbacho J, Mouliere F, Brenton JD, Caldas C, et al. 2017; Liquid biopsies come of age: towards implementation of circulating tumour DNA. Nat Rev Cancer. 17:223–38. DOI: 10.1038/nrc.2017.7. PMID: 28233803.
Article11. Hu Z, Chen H, Long Y, Li P, Gu Y. 2021; The main sources of circulating cell-free DNA: Apoptosis, necrosis and active secretion. Crit Rev Oncol Hematol. 157:103166. DOI: 10.1016/j.critrevonc.2020.103166. PMID: 33254039.
Article12. Stroun M, Lyautey J, Lederrey C, Olson-Sand A, Anker P. 2001; About the possible origin and mechanism of circulating DNA apoptosis and active DNA release. Clin Chim Acta. 313:139–42. DOI: 10.1016/S0009-8981(01)00665-9.13. Luger K, Mäder AW, Richmond RK, Sargent DF, Richmond TJ. 1997; Crystal structure of the nucleosome core particle at 2.8 A resolution. Nature. 389:251–60. DOI: 10.1038/38444. PMID: 9305837.
Article14. Bronkhorst AJ, Ungerer V, Holdenrieder S. 2019; The emerging role of cell-free DNA as a molecular marker for cancer management. Biomol Detect Quantif. 17:100087. DOI: 10.1016/j.bdq.2019.100087. PMID: 30923679. PMCID: PMC6425120.
Article15. Mouliere F, Chandrananda D, Piskorz AM, Moore EK, Morris J, Ahlborn LB, et al. 2018; Enhanced detection of circulating tumor DNA by fragment size analysis. Sci Transl Med. 10:eaat4921. DOI: 10.1126/scitranslmed.aat4921. PMID: 30404863. PMCID: PMC6483061.
Article16. Mouliere F, Robert B, Arnau Peyrotte E, Del Rio M, Ychou M, Molina F, et al. 2011; High fragmentation characterizes tumour-derived circulating DNA. PLoS One. 6:e23418. DOI: 10.1371/journal.pone.0023418. PMID: 21909401. PMCID: PMC3167805.
Article17. Abbosh C, Birkbak NJ, Wilson GA, Jamal-Hanjani M, Constantin T, Salari R, et al. 2017; Phylogenetic ctDNA analysis depicts early-stage lung cancer evolution. Nature. 545:446–51. DOI: 10.1038/nature22364. PMID: 28445469. PMCID: PMC5812436.18. Kamat AA, Bischoff FZ, Dang D, Baldwin MF, Han LY, Lin YG, et al. 2006; Circulating cell-free DNA: a novel biomarker for response to therapy in ovarian carcinoma. Cancer Biol Ther. 5:1369–74. DOI: 10.4161/cbt.5.10.3240. PMID: 16969071.
Article19. Bettegowda C, Sausen M, Leary RJ, Kinde I, Wang Y, Agrawal N, et al. 2014; Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 6:224ra24.20. Zhang Y, Yao Y, Xu Y, Li L, Gong Y, Zhang K, et al. 2021; Pan-cancer circulating tumor DNA detection in over 10,000 Chinese patients. Nat Commun. 12:11. DOI: 10.1038/s41467-020-20162-8. PMID: 33397889. PMCID: PMC7782482.
Article21. Grabuschnig S, Soh J, Heidinger P, Bachler T, Hirschböck E, Rosales Rodriguez I, et al. 2020; Circulating cell-free DNA is predominantly composed of retrotransposable elements and non-telomeric satellite DNA. J Biotechnol. 313:48–56. DOI: 10.1016/j.jbiotec.2020.03.002. PMID: 32165241.
Article22. Fleischhacker M, Schmidt B. 2007; Circulating nucleic acids (CNAs) and cancer -a survey. Biochim Biophys Acta. 1775:181–232. DOI: 10.1016/j.bbcan.2006.10.001. PMID: 17137717.23. Meddeb R, Pisareva E, Thierry AR. 2019; Guidelines for the preanalytical conditions for analyzing circulating cell-free DNA. Clin Chem. 65:623–33. DOI: 10.1373/clinchem.2018.298323. PMID: 30792266.
Article24. Shin S, Woo HI, Kim JW, Kim Y, Lee KA. 2022; Clinical practice guidelines for pre-analytical procedures of plasma epidermal growth factor receptor variant testing. Ann Lab Med. 42:141–9. DOI: 10.3343/alm.2022.42.2.141. PMID: 34635607. PMCID: PMC8548242.
Article25. El Messaoudi S, Rolet F, Mouliere F, Thierry AR. 2013; Circulating cell free DNA: Preanalytical considerations. Clin Chim Acta. 424:222–30. DOI: 10.1016/j.cca.2013.05.022. PMID: 23727028.
Article26. Martignano F. 2019; Cell-free DNA: An overview of sample types and isolation procedures. Methods Mol Biol. 1909:13–27. DOI: 10.1007/978-1-4939-8973-7_2. PMID: 30580420.
Article27. Melkonyan HS, Feaver WJ, Meyer E, Scheinker V, Shekhtman EM, Xin Z, et al. 2008; Transrenal nucleic acids: from proof of principle to clinical tests. Ann N Y Acad Sci. 1137:73–81. DOI: 10.1196/annals.1448.015. PMID: 18837928.
Article28. Tsui NB, Jiang P, Chow KC, Su X, Leung TY, Sun H, et al. 2012; High resolution size analysis of fetal DNA in the urine of pregnant women by paired-end massively parallel sequencing. PLoS One. 7:e48319. DOI: 10.1371/journal.pone.0048319. PMID: 23118982. PMCID: PMC3485143.
Article29. Yao W, Mei C, Nan X, Hui L. 2016; Evaluation and comparison of in vitro degradation kinetics of DNA in serum, urine and saliva: A qualitative study. Gene. 590:142–8. DOI: 10.1016/j.gene.2016.06.033. PMID: 27317895.
Article30. Bobillo S, Crespo M, Escudero L, Mayor R, Raheja P, Carpio C, et al. 2021; Cell free circulating tumor DNA in cerebrospinal fluid detects and monitors central nervous system involvement of B-cell lymphomas. Haematologica. 106:513–21. DOI: 10.3324/haematol.2019.241208. PMID: 32079701. PMCID: PMC7849551.
Article31. De Mattos-Arruda L, Mayor R, Ng CKY, Weigelt B, Martínez-Ricarte F, Torrejon D, et al. 2015; Cerebrospinal fluid-derived circulating tumour DNA better represents the genomic alterations of brain tumours than plasma. Nat Commun. 6:8839. DOI: 10.1038/ncomms9839. PMID: 26554728. PMCID: PMC5426516.
Article32. Kim Y, Shin S, Lee KA. 2021; Exosome-based detection of EGFR T790M in plasma and pleural fluid of prospectively enrolled non-small cell lung cancer patients after first-line tyrosine kinase inhibitor therapy. Cancer Cell Int. 21:50. DOI: 10.1186/s12935-021-01761-x. PMID: 33435996. PMCID: PMC7802208.33. Asano H, Toyooka S, Tokumo M, Ichimura K, Aoe K, Ito S, et al. 2006; Detection of EGFR gene mutation in lung cancer by mutant-enriched polymerase chain reaction assay. Clin Cancer Res. 12:43–8. DOI: 10.1158/1078-0432.CCR-05-0934. PMID: 16397022.34. Azuara D, Ginesta MM, Gausachs M, Rodriguez-Moranta F, Fabregat J, Busquets J, et al. 2012; Nanofluidic digital PCR for KRAS mutation detection and quantification in gastrointestinal cancer. Clin Chem. 58:1332–41. DOI: 10.1373/clinchem.2012.186577. PMID: 22745110.35. Taly V, Pekin D, Benhaim L, Kotsopoulos SK, Le Corre D, Li X, et al. 2013; Multiplex picodroplet digital PCR to detect KRAS mutations in circulating DNA from the plasma of colorectal cancer patients. Clin Chem. 59:1722–31. DOI: 10.1373/clinchem.2013.206359. PMID: 23938455.36. Kinde I, Wu J, Papadopoulos N, Kinzler KW, Vogelstein B. 2011; Detection and quantification of rare mutations with massively parallel sequencing. Proc Natl Acad Sci U S A. 108:9530–5. DOI: 10.1073/pnas.1105422108. PMID: 21586637. PMCID: PMC3111315.
Article37. Mosele F, Remon J, Mateo J, Westphalen CB, Barlesi F, Lolkema MP, et al. 2020; Recommendations for the use of next-generation sequencing (NGS) for patients with metastatic cancers: a report from the ESMO Precision Medicine Working Group. Ann Oncol. 31:1491–505. DOI: 10.1016/j.annonc.2020.07.014. PMID: 32853681.
Article38. Filipska M, Rosell R. 2021; Mutated circulating tumor DNA as a liquid biopsy in lung cancer detection and treatment. Mol Oncol. 15:1667–82. DOI: 10.1002/1878-0261.12983. PMID: 33969622. PMCID: PMC8169447.
Article39. Rolfo C, Mack P, Scagliotti GV, Aggarwal C, Arcila ME, Barlesi F, et al. 2021; Liquid Biopsy for Advanced NSCLC: A Consensus Statement From the International Association for the Study of Lung Cancer. J Thorac Oncol. 16:1647–62. DOI: 10.1016/j.jtho.2021.06.017. PMID: 34246791.
Article40. Litwin MS, Tan HJ. 2017; The diagnosis and treatment of prostate cancer: A review. JAMA. 317:2532–42. DOI: 10.1001/jama.2017.7248. PMID: 28655021.41. de Bono J, Mateo J, Fizazi K, Saad F, Shore N, Sandhu S, et al. 2020; Olaparib for metastatic castration-resistant prostate cancer. N Engl J Med. 382:2091–102. DOI: 10.1056/NEJMoa1911440. PMID: 32343890.
Article42. Berruti A, Dogliotti L, Bitossi R, Fasolis G, Gorzegno G, Bellina M, et al. 2000; Incidence of skeletal complications in patients with bone metastatic prostate cancer and hormone refractory disease: predictive role of bone resorption and formation markers evaluated at baseline. J Urol. 164:1248–53. DOI: 10.1016/S0022-5347(05)67149-2.
Article43. Bubendorf L, Schöpfer A, Wagner U, Sauter G, Moch H, Willi N, et al. 2000; Metastatic patterns of prostate cancer: an autopsy study of 1,589 patients. Hum Pathol. 31:578–83. DOI: 10.1053/hp.2000.6698. PMID: 10836297.
Article44. Dang HX, Chauhan PS, Ellis H, Feng W, Harris PK, Smith G, et al. 2020; Cell-free DNA alterations in the AR enhancer and locus predict resistance to AR-directed therapy in patients with metastatic prostate cancer. JCO Precis Oncol. 4:680–713. DOI: 10.1200/PO.20.00047. PMID: 32903952. PMCID: PMC7446541.45. Lau E, McCoy P, Reeves F, Chow K, Clarkson M, Kwan EM, et al. 2020; Detection of ctDNA in plasma of patients with clinically localised prostate cancer is associated with rapid disease progression. Genome Med. 12:72. DOI: 10.1186/s13073-020-00770-1. PMID: 32807235. PMCID: PMC7430029.
Article46. Shaya J, Nonato T, Cabal A, Randall JM, Millard F, Stewart T, et al. 2021; Analysis of the prognostic significance of circulating tumor DNA in metastatic castrate resistant prostate cancer. Clin Genitourin Cancer. 19:564.e1–e10. DOI: 10.1016/j.clgc.2021.07.012. PMID: 34452870.
Article47. Hong S, Won YJ, Lee JJ, Jung KW, Kong HJ, Im JS, et al. 2021; Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2018. Cancer Res Treat. 53:301–15. DOI: 10.4143/crt.2021.291. PMID: 33735559. PMCID: PMC8053867.
Article48. Kim Y, Jun JK, Choi KS, Lee HY, Park EC. 2011; Overview of the national cancer screening programme and the cancer screening status in Korea. Asian Pac J Cancer Prev. 12:725–30.49. Dasari A, Morris VK, Allegra CJ, Atreya C, Benson AB 3rd, Boland P, et al. 2020; ctDNA applications and integration in colorectal cancer: an NCI Colon and Rectal-Anal Task Forces whitepaper. Nat Rev Clin Oncol. 17:757–70. DOI: 10.1038/s41571-020-0392-0. PMID: 32632268. PMCID: PMC7790747.
Article50. Flamini E, Mercatali L, Nanni O, Calistri D, Nunziatini R, Zoli W, et al. 2006; Free DNA and carcinoembryonic antigen serum levels: an important combination for diagnosis of colorectal cancer. Clin Cancer Res. 12:6985–8. DOI: 10.1158/1078-0432.CCR-06-1931. PMID: 17145818.
Article51. Luo H, Zhao Q, Wei W, Zheng L, Yi S, Li G, et al. 2020; Circulating tumor DNA methylation profiles enable early diagnosis, prognosis prediction, and screening for colorectal cancer. Sci Transl Med. 12:eaax7533. DOI: 10.1126/scitranslmed.aax7533. PMID: 31894106.
Article52. Tie J, Wang Y, Springer S, Kinde I, Wong HL, Kosmider S, et al. 2016; Serial circulating tumor DNA (ctDNA) and recurrence risk in patients (pts) with resectable colorectal liver metastasis (CLM). J Clin Oncol. 34(S):e15131–e15131. DOI: 10.1200/JCO.2016.34.15_suppl.e15131.
Article53. Venook AP, Niedzwiecki D, Lenz HJ, Innocenti F, Fruth B, Meyerhardt JA, et al. 2017; Effect of first-line chemotherapy combined with cetuximab or bevacizumab on overall survival in patients with KRAS wild-type advanced or metastatic colorectal cancer: A randomized clinical trial. JAMA. 317:2392–401. DOI: 10.1001/jama.2017.7105. PMID: 28632865. PMCID: PMC5545896.
Article54. Kopetz S, Grothey A, Yaeger R, Van Cutsem E, Desai J, Yoshino T, et al. 2019; Encorafenib, binimetinib, and cetuximab in BRAF V600E-mutated colorectal cancer. N Engl J Med. 381:1632–43. DOI: 10.1056/NEJMoa1908075. PMID: 31566309.
Article55. Meric-Bernstam F, Hurwitz H, Raghav KPS, McWilliams RR, Fakih M, VanderWalde A, et al. 2019; Pertuzumab plus trastuzumab for HER2-amplified metastatic colorectal cancer (MyPathway): an updated report from a multicentre, open-label, phase 2a, multiple basket study. Lancet Oncol. 20:518–30. DOI: 10.1016/S1470-2045(18)30904-5.56. Tay TKY, Tan PH. 2021; Liquid biopsy in breast cancer: A focused review. Arch Pathol Lab Med. 145:678–86. DOI: 10.5858/arpa.2019-0559-RA. PMID: 32045277.
Article57. Magbanua MJM, Swigart LB, Wu HT, Hirst GL, Yau C, Wolf DM, et al. 2021; Circulating tumor DNA in neoadjuvant-treated breast cancer reflects response and survival. Ann Oncol. 32:229–39. DOI: 10.1016/j.annonc.2020.11.007. PMID: 33232761. PMCID: PMC9348585.
Article58. Chopra N, Tovey H, Pearson A, Cutts R, Toms C, Proszek P, et al. 2020; Homologous recombination DNA repair deficiency and PARP inhibition activity in primary triple negative breast cancer. Nat Commun. 11:2662. DOI: 10.1038/s41467-020-16142-7. PMID: 32471999. PMCID: PMC7260192.
Article59. Rose M, Burgess JT, O'Byrne K, Richard DJ, Bolderson E. PARP inhibitors: Clinical relevance, mechanisms of action and tumor resistance. Front Cell Dev Biol. 2020; 8:564601. DOI: 10.3389/fcell.2020.564601. PMID: 33015058. PMCID: PMC7509090.
Article60. Weigelt B, Comino-Méndez I, de Bruijn I, Tian L, Meisel JL, García-Murillas I, et al. 2017; Diverse BRCA1 and BRCA2 reversion mutations in circulating cell-free DNA of therapy-resistant breast or ovarian cancer. Clin Cancer Res. 23:6708–20. DOI: 10.1158/1078-0432.CCR-17-0544. PMID: 28765325. PMCID: PMC5728372.61. Cheng ML, Pectasides E, Hanna GJ, Parsons HA, Choudhury AD, Oxnard GR. 2021; Circulating tumor DNA in advanced solid tumors: Clinical relevance and future directions. CA Cancer J Clin. 71:176–90. DOI: 10.3322/caac.21650. PMID: 33165928.
Article62. Ballehaninna UK, Chamberlain RS. 2012; The clinical utility of serum CA 19-9 in the diagnosis, prognosis and management of pancreatic adenocarcinoma: An evidence based appraisal. J Gastrointest Oncol. 3:105–19.63. Sivapalan L, Kocher HM, Ross-Adams H, Chelala C. 2021; Molecular profiling of ctDNA in pancreatic cancer: Opportunities and challenges for clinical application. Pancreatology. 21:363–78. DOI: 10.1016/j.pan.2020.12.017. PMID: 33451936. PMCID: PMC7994018.
Article64. Grunvald MW, Jacobson RA, Kuzel TM, Pappas SG, Masood A. 2020; Current status of circulating tumor DNA liquid biopsy in pancreatic cancer. Int J Mol Sci. 21:7651. DOI: 10.3390/ijms21207651. PMID: 33081107. PMCID: PMC7589736.
Article65. Giornelli GH. 2016; Management of relapsed ovarian cancer: a review. Springerplus. 5:1197. DOI: 10.1186/s40064-016-2660-0. PMID: 27516935. PMCID: PMC4963348.
Article66. Asante DB, Calapre L, Ziman M, Meniawy TM, Gray ES. 2020; Liquid biopsy in ovarian cancer using circulating tumor DNA and cells: Ready for prime time? Cancer Lett. 468:59–71. DOI: 10.1016/j.canlet.2019.10.014. PMID: 31610267.
Article67. Vargas AN. 2014; Natural history of ovarian cancer. Ecancermedicalscience. 8:465.68. Bogani G, Matteucci L, Tamberi S, Ditto A, Sabatucci I, Murgia F, et al. 2019; RECIST 1.1 criteria predict recurrence-free survival in advanced ovarian cancer submitted to neoadjuvant chemotherapy. Eur J Obstet Gynecol Reprod Biol. 237:93–9. DOI: 10.1016/j.ejogrb.2019.04.007. PMID: 31029972.
Article69. Charkhchi P, Cybulski C, Gronwald J, Wong FO, Narod SA, Akbari MR. 2020; CA125 and ovarian cancer: A comprehensive review. Cancers (Basel). 12:3730. DOI: 10.3390/cancers12123730. PMID: 33322519. PMCID: PMC7763876.
Article70. Hentze JL, Høgdall C, Kjær SK, Blaakær J, Høgdall E. 2017; Searching for new biomarkers in ovarian cancer patients: Rationale and design of a retrospective study under the Mermaid III project. Contemp Clin Trials Commun. 8:167–74. DOI: 10.1016/j.conctc.2017.10.003. PMID: 29696206. PMCID: PMC5898550.
Article71. Asaoka Y, Ijichi H, Koike K. 2015; PD-1 Blockade in tumors with mismatch-repair deficiency. N Engl J Med. 373:1979. DOI: 10.1056/NEJMc1510353.
Article72. Georgiadis A, Durham JN, Keefer LA, Bartlett BR, Zielonka M, Murphy D, et al. 2019; Non-invasive detection of microsatellite instability and high tumor mutation burden in cancer patients treated with PD-1 blockade. Clin Cancer Res. 25:7024–34. DOI: 10.1158/1078-0432.CCR-19-1372. PMID: 31506389. PMCID: PMC6892397.
Article73. Friedlaender A, Nouspikel T, Christinat Y, Ho L, McKee T, Addeo A. 2020; Tissue-plasma TMB comparison and plasma TMB monitoring in patients with metastatic non-small cell lung cancer receiving immune checkpoint inhibitors. Front Oncol. 10:142. DOI: 10.3389/fonc.2020.00142. PMID: 32117779. PMCID: PMC7028749.
Article74. Qiu P, Poehlein CH, Marton MJ, Laterza OF, Levitan D. 2019; Measuring tumor mutational burden (TMB) in plasma from mCRPC patients using two commercial NGS assays. Sci Rep. 9:114. DOI: 10.1038/s41598-018-37128-y. PMID: 30643180. PMCID: PMC6331610.
Article75. Miyazawa H, Tanaka T, Nagai Y, Matsuoka M, Sutani A, Udagawa K, et al. 2008; Peptide nucleic acid-locked nucleic acid polymerase chain reaction clamp-based detection test for gefitinib-refractory T790M epidermal growth factor receptor mutation. Cancer Sci. 99:595–600. DOI: 10.1111/j.1349-7006.2007.00706.x. PMID: 18271876.
Article76. Freidin MB, Freydina DV, Leung M, Montero Fernandez A, Nicholson AG, Lim E. 2015; Circulating tumor DNA outperforms circulating tumor cells for KRAS mutation detection in thoracic malignancies. Clin Chem. 61:1299–304. DOI: 10.1373/clinchem.2015.242453. PMID: 26272233.77. Sefrioui D, Sarafan-Vasseur N, Beaussire L, Baretti M, Gangloff A, Blan-chard F, et al. 2015; Clinical value of chip-based digital-PCR platform for the detection of circulating DNA in metastatic colorectal cancer. Dig Liver Dis. 47:884–90. DOI: 10.1016/j.dld.2015.05.023. PMID: 26160500.
Article78. Taniguchi K, Uchida J, Nishino K, Kumagai T, Okuyama T, Okami J, et al. 2011; Quantitative detection of EGFR mutations in circulating tumor DNA derived from lung adenocarcinomas. Clin Cancer Res. 17:7808–15. DOI: 10.1158/1078-0432.CCR-11-1712. PMID: 21976538.79. Newman AM, Bratman SV, To J, Wynne JF, Eclov NCW, Modlin LA, et al. 2014; An ultrasensitive method for quantitating circulating tumor DNA with broad patient coverage. Nat Med. 20:548–54. DOI: 10.1038/nm.3519. PMID: 24705333. PMCID: PMC4016134.
Article80. Gale D, Lawson ARJ, Howarth K, Madi M, Durham B, Smalley S, et al. 2018; Development of a highly sensitive liquid biopsy platform to detect clinically-relevant cancer mutations at low allele fractions in cell-free DNA. PLoS One. 13:e0194630. DOI: 10.1371/journal.pone.0194630. PMID: 29547634. PMCID: PMC5856404.
Article81. Narayan A, Carriero NJ, Gettinger SN, Kluytenaar J, Kozak KR, Yock TI, et al. 2012; Ultrasensitive measurement of hotspot mutations in tumor DNA in blood using error-suppressed multiplexed deep sequencing. Cancer Res. 72:3492–8. DOI: 10.1158/0008-5472.CAN-11-4037. PMID: 22581825. PMCID: PMC3426449.
Article82. Dai P, Wu LR, Chen SX, Wang MX, Cheng LY, Zhang JX, et al. 2021; Calibration-free NGS quantitation of mutations below 0.01% VAF. Nat Commun. 12:6123. DOI: 10.1038/s41467-021-26308-6. PMID: 34675197. PMCID: PMC8531361.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Circulating Tumor DNA Testing for Precision Oncology
- Current Methods of Circulating Tumor Cell Detection
- Circulating Tumor Cell and Cell-free Circulating Tumor DNA in Lung Cancer
- Exploring the prognostic value of ultra-low-pass whole-genome sequencing of circulating tumor DNA in hepatocellular carcinoma
- Circulating Tumor Cells: Detection Methods and Potential Clinical Application in Breast Cancer