J Korean Diabetes.
2022 Dec;23(4):266-277. 10.4093/jkd.2022.23.4.266.
Validation of Foot Pressure Variables during Walking according to Glycated Hemoglobin Levels
- Affiliations
-
- 1Graduate School in Division of Kinesiology & Sports Studies, College of Science & Industry Convergence, Ewha Womans University, Seoul, Korea
- 2College of Nursing, Ewha Womans University, Seoul, Korea
- 3Department of Endocrinology, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea
- 4Department of Nutritional Science & Food Management, College of Science & Industry Convergence, Ewha Womans University, Seoul, Korea
- 5Graduate School in Division of Kinesiology & Sports Studies, Graduate Program in System Health Science and Engineering, Ewha Womans University, Seoul, Korea
- 6Graduate Program in System Health Science and Engineering, Ewha Womans University, Seoul, Korea
- KMID: 2538098
- DOI: http://doi.org/10.4093/jkd.2022.23.4.266
Abstract
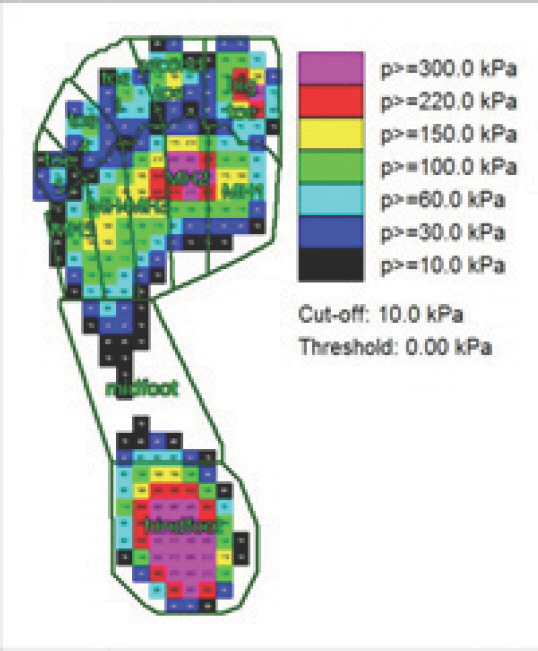
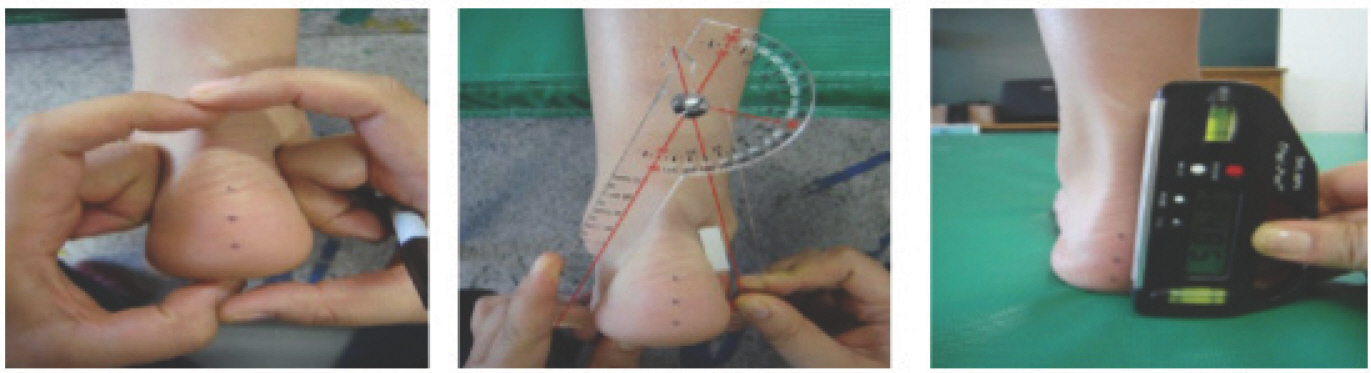
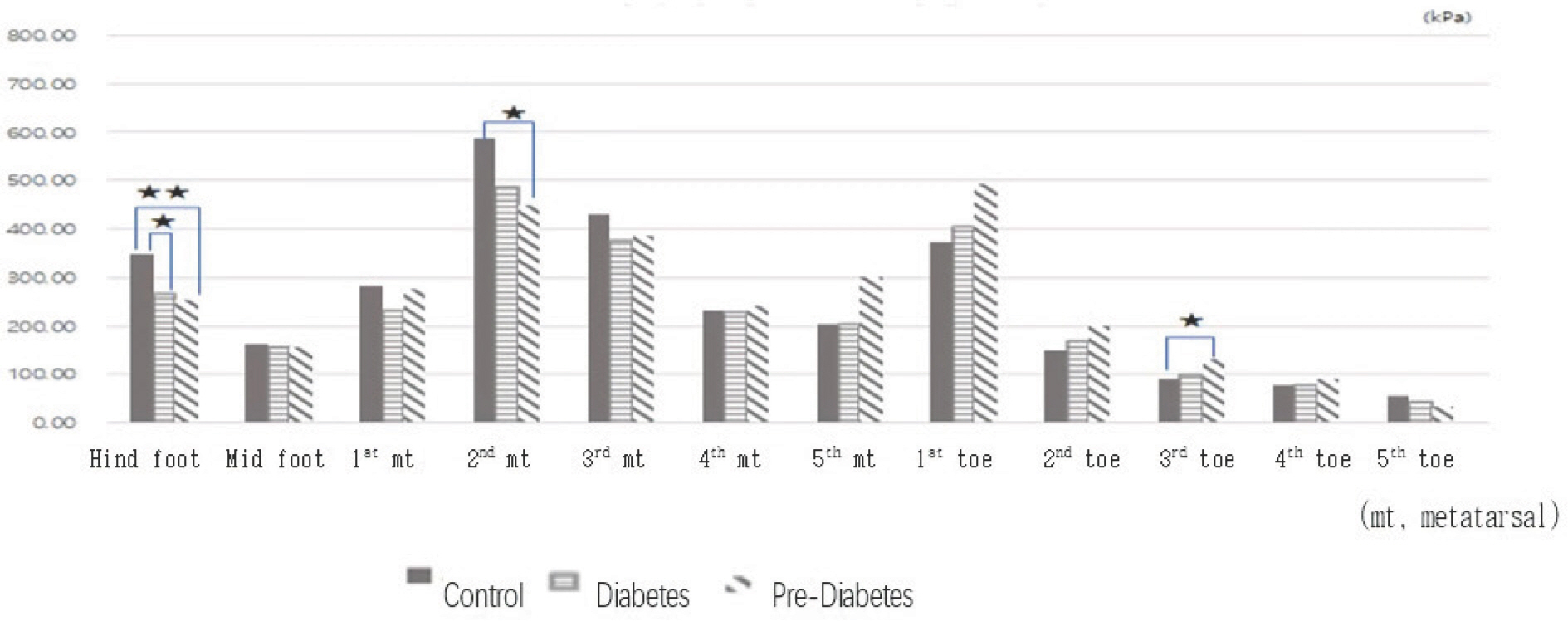
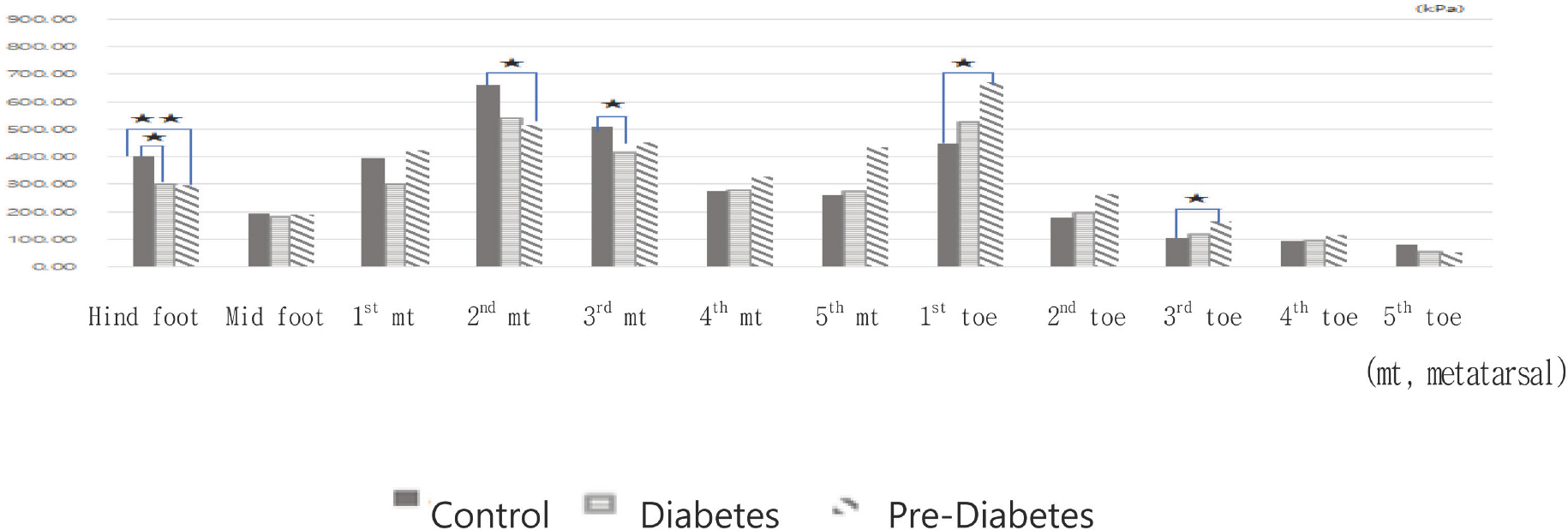
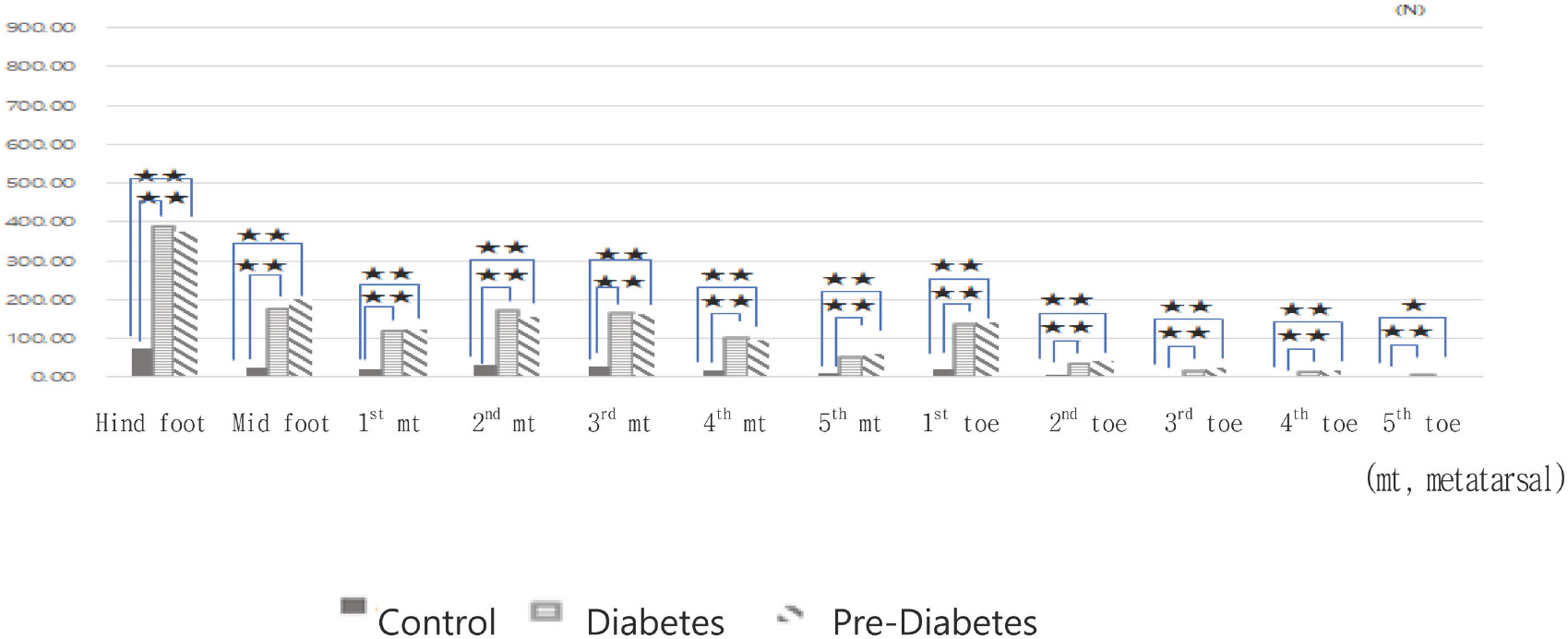
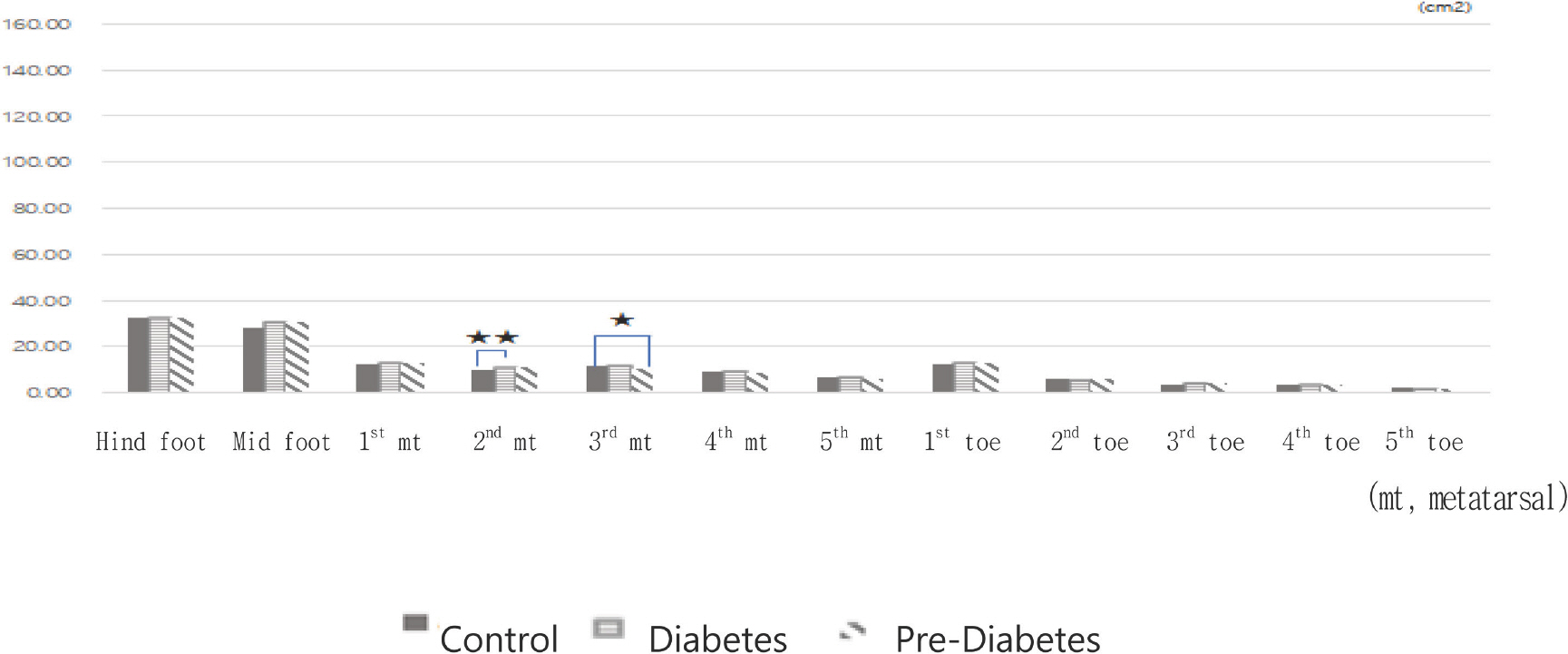
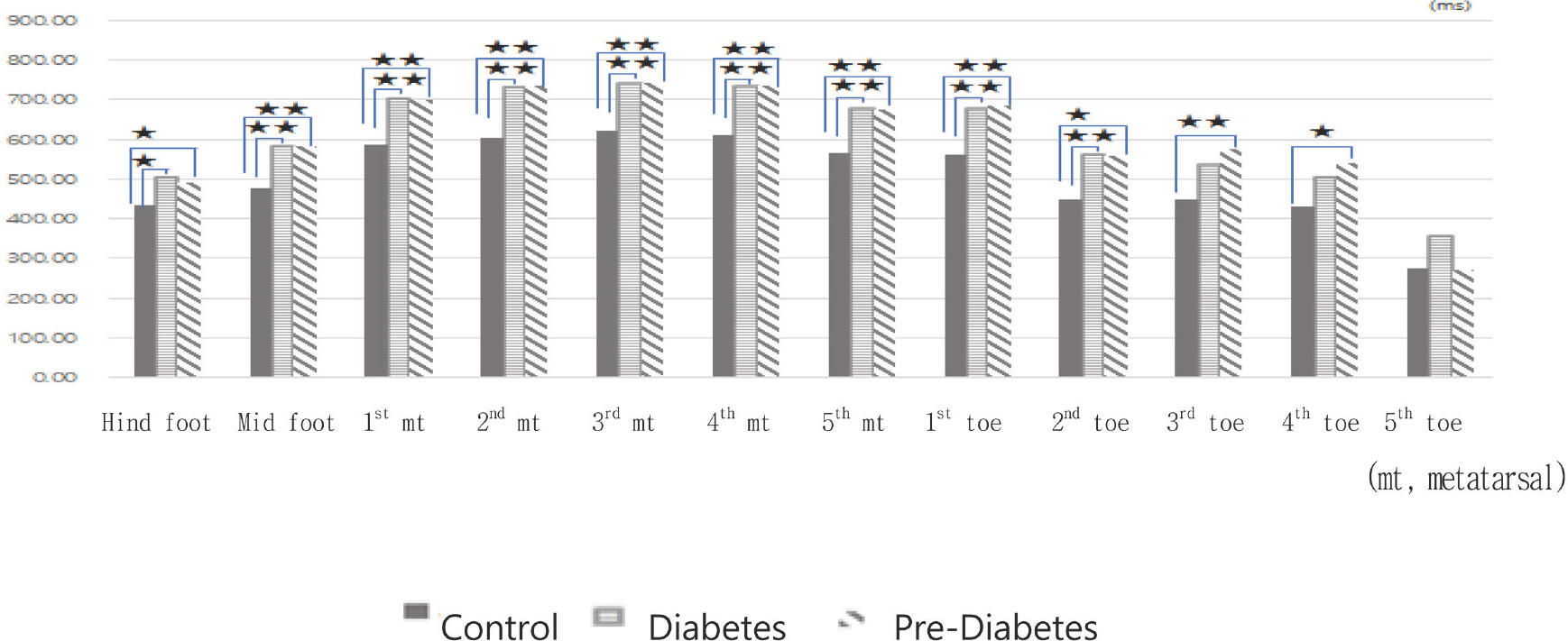
- The purpose of this study was to explore the variables of foot pressure according to glycated hemoglobin level during walking in diabetic patients with pes rectus. The subjects of this study were 39 people (78 feet) in their 40s and 60s, and they were divided into 11 pre-diabetic patients (22 feet) and 14 diabetic patients (28 feet) based on glycated hemoglobin; 14 patients without diabetes (28 feet) was used as a control. Foot pressure was measured using the EMED-LE Measurement system. The sole of the foot was divided into 12 parts, each of which was analyzed for pressure, force, contact area, and grounding time. For statistics, nonparametric Kruskal–Wallis and Wilcoxon signed rank test were used. Prediabetic and diabetic patients had lower hindfoot and second and third metatarsal foot pressure but higher first and third toe pressure compared to those without diabetes. In addition, the maximum and minimum force were high in all parts of the sole, and the contact time was long, signifying strong downward force for a long duration. Measurement of foot pressure by parts allowed detailed analysis of abnormal foot pressure and is valuable as basic data for diagnosis, prediction, and treatment of diabetic foot. Based on these data, maximum and minimum pressure better explain the problem of plantar pressure distribution rather than mean maximum pressure.
Keyword
Figure
Reference
-
1.Dornan J., Fernie GR., Holliday PJ. Visual input: its im-portance in the control of postural sway. Arch Phys Med Rehabil. 1978. 59:586–91.2.Horak FB. Clinical measurement of postural control in adults. Phys Ther. 1987. 67:1881–5.3.Kay AD., Tideiksaar R. Falls and gait disorders. Abrams WB, Berkow R, editors. The Merck manual of geriatrics. Rah-way: Merck and Co., Inc.;1990. p. 52–68.4.Yu X., Yu GR., Chen YX., Liu XC. The characteristics and clinical significance of plantar pressure distribution in patients with diabetic toe deformity: a dynamic plantar pressure analysis. J Int Med Res. 2011. 39:2352–9.5.Wafai L., Zayegh A., Woulfe J., Aziz SM., Begg R. Identification of foot pathologies based on plantar pressure asym-metry. Sensors (Basel). 2015. 15:20392–408.6.Wrobel JS., Najafi B. Diabetic foot biomechanics and gait dysfunction. J Diabetes Sci Technol. 2010. 4:833–45.7.Boulton AJ., Hardisty CA., Betts RP., Franks CI., Worth RC., Ward JD, et al. Dynamic foot pressure and other studies as diagnostic and management aids in diabetic neuropathy. Diabetes Care. 1983. 6:26–33.8.Cavanagh PR., Bus SA. Off-loading the diabetic foot for ulcer prevention and healing. J Vasc Surg. 2010. 52(3 Suppl):37S–43S.9.Bus SA. Priorities in offloading the diabetic foot. Diabetes Metab Res Rev. 2012. 28(Suppl 1):54–9.10.Bus SA., Haspels R., Busch-Westbroek TE. Evaluation and optimization of therapeutic footwear for neuropathic diabetic foot patients using in-shoe plantar pressure analysis. Diabetes Care. 2011. 34:1595–600.11.Bus SA., Ulbrecht JS., Cavanagh PR. Pressure relief and load redistribution by custom-made insoles in diabetic patients with neuropathy and foot deformity. Clin Biomech (Bristol, Avon). 2004. 19:629–38.12.Hwang AH. Differences in plantar pressure according to t ankle instability, foot shape, and type of socks during walking [master's thesis]. Seoul: Ewha Womans University;2021.13.Yi KO. The effect of shoe type on plantar pressure distri-butions. J Korean Phys Educ Assoc Girls Women. 2010. 24:1–11.14.Seo DK., Lee HS. Management of diabetic foot ulcer. J Korean Foot Ankle Soc. 2014. 18:1–7.15.Castro MP., Soares D., Mendes E., Machado L. Plantar pressures and ground reaction forces during walking of individuals with unilateral transfemoral amputation. PM R. 2014. 6:698–707.e1.16.Fawzy OA., Arafa AI., El Wakeel MA., Abdul Kareem SH. Plantar pressure as a risk assessment tool for diabetic foot ulceration in Egyptian patients with diabetes. Clin Med Insights Endocrinol Diabetes. 2014. 7:31–9.17.Lin TL., Sheen HM., Chung CT., Yang SW., Lin SY., Luo HJ, et al. The effect of removing plugs and adding arch sup-port to foam based insoles on plantar pressures in people with diabetic peripheral neuropathy. J Foot Ankle Res. 2013. 6:29.18.Melai T., IJzerman TH., Schaper NC., de Lange TL., Wil-lems PJ., Meijer K, et al. Calculation of plantar pressure time integral, an alternative approach. Gait Posture. 2011. 34:379–83.19.Bus SA., Maas M., de Lange A., Michels RP., Levi M. Elevat-ed plantar pressures in neuropathic diabetic patients with claw/hammer toe deformity. J Biomech. 2005. 38:1918–25.20.Veves A., Fernando DJS., Walewski P., Boulton AJM. A study of plantar pressures in a diabetic clinic population. The Foot. 1991. 1:89–92.21.Deschamps K., Matricali GA., Roosen P., Desloovere K., Bruyninckx H., Spaepen P, et al. Classification of forefoot plantar pressure distribution in persons with diabetes: a novel perspective for the mechanical management of diabetic foot? PLoS One. 2013. 8:e79924.22.Park K., Kwon O., Kim Y. Effects of walking speed on foot joint motion and peak plantar pressure in healthy subjects. KAUTPT. 2003. 10:77–95.23.Brach JS., Perera S., Studenski S., Newman AB. The reliabil-ity and validity of measures of gait variability in communi-ty-dwelling older adults. Arch Phys Med Rehabil. 2008. 89:2293–6.24.de Cesar Netto C., Kunas GC., Soukup D., Marinescu A., Ellis SJ. Correlation of clinical evaluation and radiograph-ic hindfoot alignment in stage II adult-acquired flatfoot deformity. Foot Ankle Int. 2018. 39:771–9.25.Yi KO., Kim NH., Kim YR. The differences in foot type according to major in left and right foot for female college students. Korean J Sport Biomech. 2012. 22:229–36.26.Tang UH., Zügner R., Lisovskaja V., Karlsson J., Hagberg K., Tranberg R. Foot deformities, function in the lower ex-tremities, and plantar pressure in patients with diabetes at high risk to develop foot ulcers. Diabet Foot Ankle. 2015. 6:27593.27.Lee S., Kim H., Choi S., Park Y., Kim Y., Cho B. Clinical use-fulness of the two-site Semmes-Weinstein monofilament test for detecting diabetic peripheral neuropathy. J Korean Med Sci. 2003. 18:103–7.28.Feng Y., Schlösser FJ., Sumpio BE. The Semmes Weinstein monofilament examination as a screening tool for diabetic peripheral neuropathy. J Vasc Surg. 2009. 50:675–82. 82.e1.29.Boffeli TJ., Bean JK., Natwick JR. Biomechanical abnor-malities and ulcers of the great toe in patients with diabetes. J Foot Ankle Surg. 2002. 41:359–64.30.Ko M., Hughes L., Lewis H. Walking speed and peak plantar pressure distribution during barefoot walking in persons with diabetes. Physiother Res Int. 2012. 17:29–35.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Asymmetrical Weight Bearing during Straight and Circular Walking in Hemiplegic Patients
- Hemoglobin A1c, Not Glycated Albumin, Can Independently Reflect the Ankylosing Spondylitis Disease Activity Score
- Relationship between Depression and Glycated Hemoglobin: Analysis Based on the 2019 Korea National Health and Nutrition Examination Survey
- Characteristics of Foot Pressure Distribution with or without Partial Prosthetic Foot in Transmetartarsal Amputee
- The Effect of Ballet Shoes on Plantar Foot during Ambulation