Pediatr Emerg Med J.
2022 Dec;9(2):82-89. 10.22470/pemj.2022.00500.
Changes in pediatric injury-related visits during coronavirus disease 2019 pandemic at a single regional emergency medical center in Korea
- Affiliations
-
- 1Department of Emergency Medicine, Myongji Hospital, Goyang, Republic of Korea
- 2Department of Emergency Medicine, Myongji Hospital, Hanyang University College of Medicine, Seoul, Republic of Korea
- KMID: 2538068
- DOI: http://doi.org/10.22470/pemj.2022.00500
Abstract
- Purpose
This study was aimed to investigate the changes in pediatric injury-related visits at an emergency department (ED) during coronavirus disease 2019 pandemic.
Methods
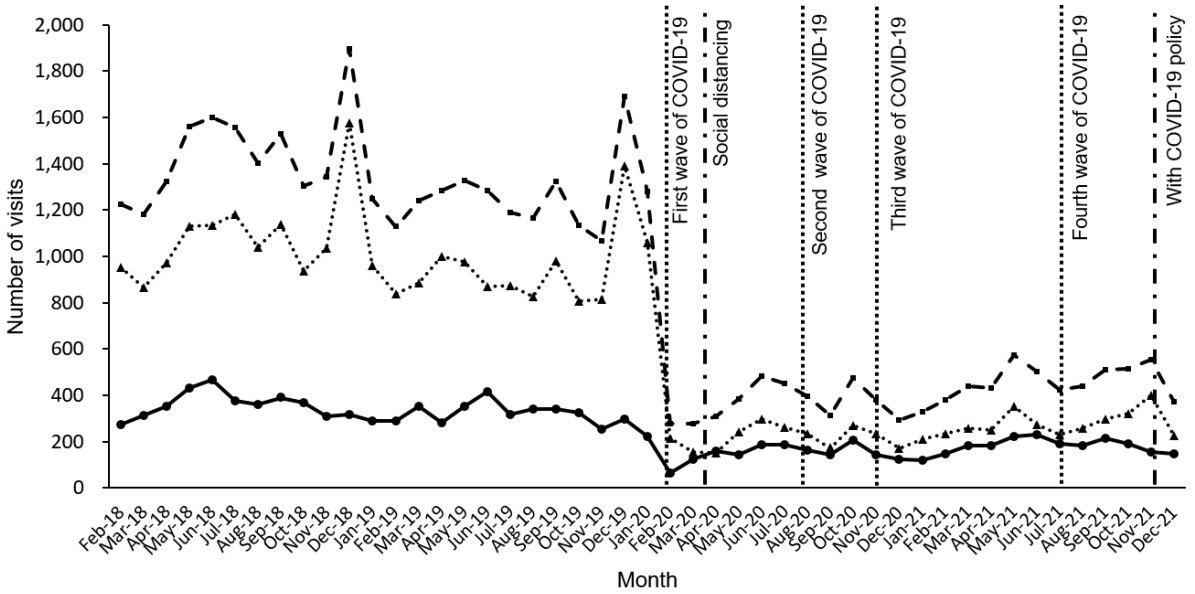
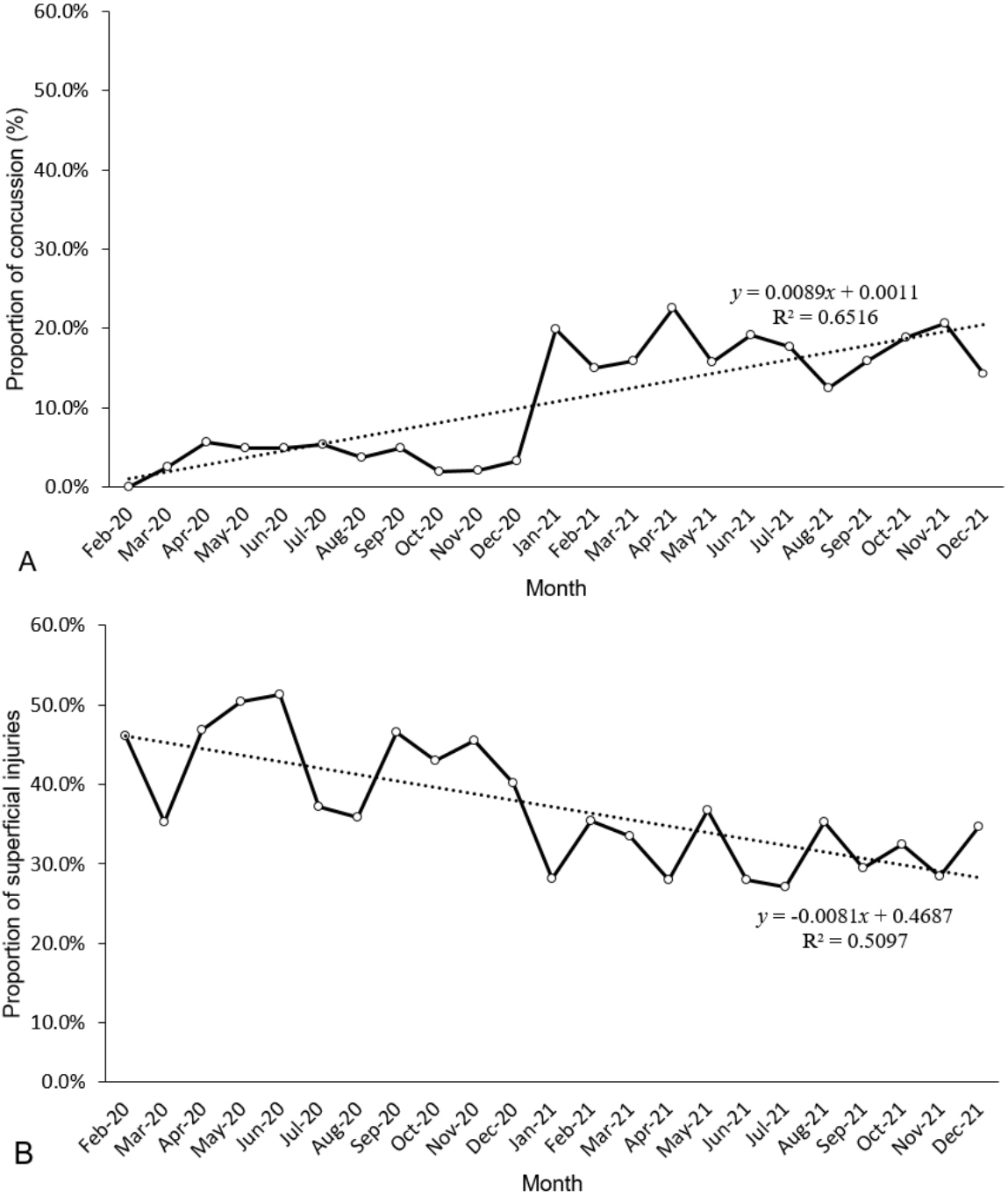
We retrospectively compared injury-related visits to an ED in Korea by children aged 15 years or younger during February 2020-December 2021 (pandemic period), and the visits during February 2018-December 2019. Clinical characteristics, injury mechanisms, diagnostic codes, and ED outcomes were noted. We performed 2 sub-analyses of the pandemic period: biannual changes in the visits, and monthly trends of proportions of concussion and superficial injury as diagnostic codes using linear regression.
Results
Despite a 51.2% reduction in injury-related visits during the pandemic, the proportion of the visits increased (25.2% vs. 40.0%; P < 0.001). Overall, increases were noted in proportions of use of emergency medical services and high acuity (P < 0.001). Among the diagnostic codes, brain injuries, fracture and dislocation, and laceration increased while superficial injuries, burn, intoxication, and foreign body ingestion decreased (P < 0.001). As the pandemic prolonged, injury-to-ED time shortened and ED length of stay lengthened while the abovementioned trends remained unchanged. Linear regression showed that the proportions of concussion and superficial injury respectively increased and decreased by 0.01% per month (P < 0.001).
Conclusion
The changes in pediatric injury-related visits at the ED during the coronavirus disease 2019 pandemic may serve as a basis for distributing emergency medicine resources in future infectious disease outbreaks.
Keyword
Figure
Reference
-
References
1. U.S. Centers for Disease Control and Prevention (CDC). COVID-19 [Internet]. Atlanta: CDC;2020. [cited 2022 Jul 12]. Available from https://www.cdc.gov/coronavirus/2019-ncov.2. Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020; 133:81–8.3. Scheier E, Levick N, Guri A, Balla U. The injury-illness dichotomy of COVID-19 on the pediatric ED. Am J Emerg Med. 2022; 52:244–8.4. Chaudhari PP, Anderson M, Ourshalimian S, Goodhue C, Sudharshan R, Valadez S, et al. Epidemiology of pediatric trauma during the coronavirus disease-2019 pandemic. J Pediatr Surg. 2022; 57:284–90.5. Choi DH, Jung JY, Suh D, Choi JY, Lee SU, Choi YJ, et al. Impact of the COVID-19 outbreak on trends in emergency department utilization in children: a multicenter retrospective observational study in Seoul metropolitan area, Korea. J Korean Med Sci. 2021; 36:e44.6. Jang KM, Ahn JY, Choi HJ, Lee S, Kim D, Lee DW, et al. Pediatric emergency department utilization and coronavirus disease in Daegu, Korea. J Korean Med Sci. 2021; 36:e32.7. Hwang Y, Jo HY, Yoo HW, Kim YM, Kim HY. Characteristics of children with trauma compared to those with disease in the emergency department: a Korean single regional emergency medical center study. Pediatr Emerg Med J. 2020; 7:108–13. Korean.8. Hwang SY, Lee JK, Rye HS, Park SS, Choi JY, Lee HJ, et al. Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea. Pediatr Emerg Med J. 2021; 8:57–65. Korean.9. Vital Statistics Division Statistics Korea, Shin HY, Lee JY, Kim JE, Lee S, Youn H, et al. Cause-of-death statistics in 2016 in the Republic of Korea. J Korean Med Assoc. 2018; 61:573–84.10. Choi A, Bae W, Kim K, Kim S. Impact of Covid-19 on the Visit of Pediatric Patients with Injuries to the Emergency Department in Korea. Children (Basel). 2021; 8:568.11. Mantica G, Riccardi N, Terrone C, Gratarola A. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Public Health. 2020; 183:40–1.12. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020; 4:e10–1.13. Chung HS, Lee DE, Kim JK, Yeo IH, Kim C, Park J, et al. Revised triage and surveillance protocols for temporary emergency department closures in tertiary hospitals as a response to COVID-19 crisis in Daegu Metropolitan City. J Korean Med Sci. 2020; 35:e189.14. Office for Government Policy Coordination. Prime Minister’s Secretariat [Internet]. Sejong (Korea): Prime Minister’s Secretariat;2020. [cited 2022 Jul 12]. Available from https://www.opm.go.kr/flexer/view.do?ftype=hwp&attachNo=103482. Korean.15. Jang WM, Jang DH, Lee JY. Social distancing and transmission-reducing practices during the 2019 coronavirus disease and 2015 Middle East respiratory syndrome coronavirus outbreaks in Korea. J Korean Med Sci. 2020; 35:e220.16. Kim MC, Park JH, Choi SH, Chung JW. Rhinovirus incidence rates indicate we are Tired of non-pharmacological interventions against coronavirus disease 2019. J Korean Med Sci. 2022; 37:e15.17. Lelak KA, Vohra V, Neuman MI, Farooqi A, Toce MS, Sethuraman U. COVID-19 and pediatric ingestions. Pediatrics. 2021; 148:e2021051001.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in pediatric psychiatric emergency during the coronavirus disease 2019 pandemic
- Coronavirus disease 2019 pandemic-related change in children’s visits to the emergency department
- Effect of coronavirus disease 2019 pandemic on children’s visits to the emergency department
- Impact of coronavirus disease 2019 pandemic on pediatric poisoning in a single emergency department in Korea
- Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea