Ann Surg Treat Res.
2023 Jan;104(1):27-33. 10.4174/astr.2023.104.1.27.
National trend of the treatment for chronic venous diseases in Korea between 2010 and 2020
- Affiliations
-
- 1Department of Surgery, Kyung Hee University Hospital at Gangdong, Kyung Hee University School of Medicine, Seoul, Korea
- KMID: 2537625
- DOI: http://doi.org/10.4174/astr.2023.104.1.27
Abstract
- Purpose
Limited data are available on the nationwide trend of treatments for chronic venous disease (CVD). The aim of the present study was to identify the nationwide trends of CVD treatments in Korea.
Methods
A serial, cross-sectional study was conducted with the use of time trends to analyze patients with CVD between 2010 and 2020. The trends in the number of patients and procedures were analyzed including sclerotherapy, open surgery, and endovenous thermal ablation (ETA). Health Insurance Review and Assessment Service data were used to analyze the trends. For the statistical analysis, MedCalc Statistical software was used. P < 0.05 was considered statistically significant.
Results
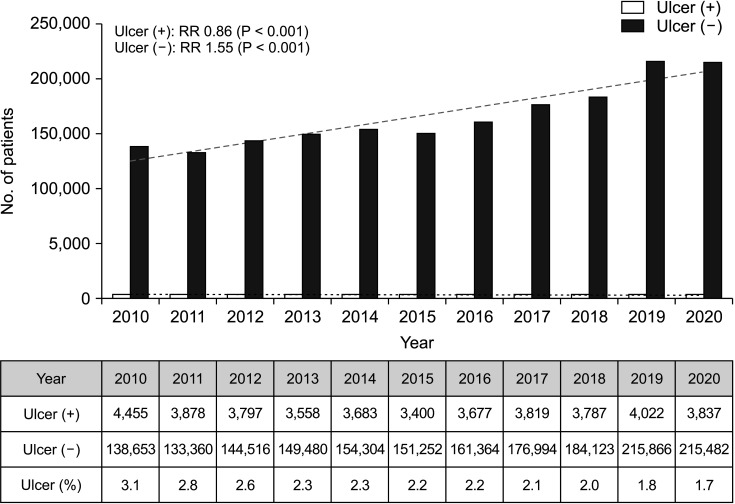
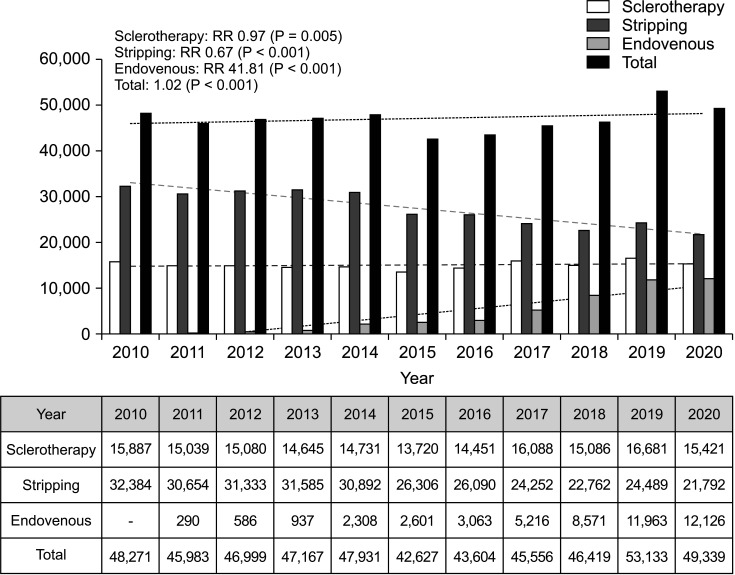
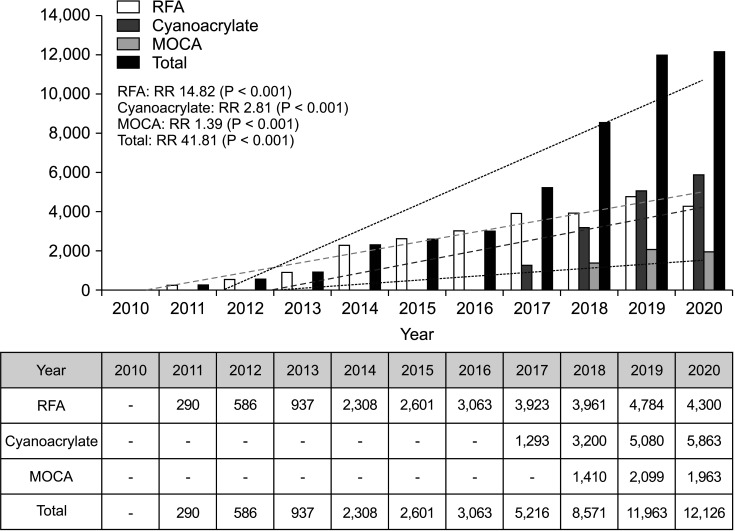
A total of 1,867,307 patients with CVD were managed in Korea between 2010 and 2020. The annual number of patients with CVD increased from 143,108 in 2010 to 219,319 in 2020 (risk ratio [RR], 1.53; P < 0.001). The percentage of patients with CVD who had venous ulcer gradually decreased from 3.1% in 2010 to 1.7% in 2020 (RR, 0.86; P < 0.001). The number of conventional surgeries including stripping and local resection of varicose veins decreased from 32,384 in 2010 to 21,792 in 2020 (RR, 0.67; P < 0.001). The number of ETAs performed increased, from 290 in 2011 to 12,126 procedures in 2020 (RR, 41.81; P < 0.001).
Conclusion
The total number of patients with CVD increased during the last 11 years. The number of conventional open surgery and sclerotherapy procedures decreased. On the contrary, the number of ETAs significantly increased in Korea.
Keyword
Figure
Reference
-
1. White JV, Ryjewski C. Chronic venous insufficiency. Perspect Vasc Surg Endovasc Ther. 2005; 17:319–327. PMID: 16389426.2. Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation. 2005; 111:2398–2409. PMID: 15883226.3. Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005; 15:175–184. PMID: 15723761.4. Durkin MT, Turton EP, Wijesinghe LD, Scott DJ, Berridge DC. Long saphenous vein stripping and quality of life: a randomised trial. Eur J Vasc Endovasc Surg. 2001; 21:545–549. PMID: 11397030.5. Perkins JM. Standard varicose vein surgery. Phlebology. 2009; 24 Suppl 1:34–41. PMID: 19307439.6. Joh JH, Kim WS, Jung IM, Park KH, Lee T, Kang JM. Consensus for the treatment of varicose vein with radiofrequency ablation. Vasc Specialist Int. 2014; 30:105–112. PMID: 26217628.7. Kanwar A, Hansrani M, Lees T, Stansby G. Trends in varicose vein therapy in England: radical changes in the last decade. Ann R Coll Surg Engl. 2010; 92:341–346. PMID: 20501021.8. Almeida J, Kabnick L, Wakefield T, Raffetto J, McLafferty R, Pappas P, et al. Management trends for chronic venous insufficiency across the United States: a report from the American Venous Registry. J Vasc Surg Venous Lymphat Disord. 2013; 1:100.9. Kim L, Kim JA, Kim S. A guide for the utilization of health insurance review and assessment service national patient samples. Epidemiol Health. 2014; 36:e2014008. PMID: 25078381.10. Kroeger K, Ose C, Rudofsky G, Roesener J, Hirche H. Risk factors for varicose veins. Int Angiol. 2004; 23:29–34. PMID: 15156127.11. Callam MJ. Epidemiology of varicose veins. Br J Surg. 1994; 81:167–173. PMID: 8156326.12. Park J, Kim SG, Park JS, Han B, Kim KB, Kim Y. Hazards and health problems in occupations dominated by aged workers in South Korea. Ann Occup Environ Med. 2017; 29:27. PMID: 28670457.13. Lee AJ, Evans CJ, Allan PL, Ruckley CV, Fowkes FG. Lifestyle factors and the risk of varicose veins: Edinburgh Vein Study. J Clin Epidemiol. 2003; 56:171–179. PMID: 12654412.14. Segiet OA, Brzozowa-Zasada M, Piecuch A, Dudek D, Reichman-Warmusz E, Wojnicz R. Biomolecular mechanisms in varicose veins development. Ann Vasc Surg. 2015; 29:377–384. PMID: 25449990.15. Sugerman HJ, Sugerman EL, Wolfe L, Kellum JM, Schweitzer MA, DeMaria EJ. Risks and benefits of gastric bypass in morbidly obese patients with severe venous stasis disease. Ann Surg. 2001; 234:41–46. PMID: 11460821.16. Han K, Park S, Symanzik J, Choi S, Ahn J. Trends in obesity at the national and local level among South Korean adolescents. Geospat Health. 2016; 11:381. PMID: 27245793.17. Oh MD, Park WB, Park SW, Choe PG, Bang JH, Song KH, et al. Middle East respiratory syndrome: what we learned from the 2015 outbreak in the Republic of Korea. Korean J Intern Med. 2018; 33:233–246. PMID: 29506344.18. Lee SI. Costly lessons from the 2015 Middle East respiratory syndrome coronavirus outbreak in Korea. J Prev Med Public Health. 2015; 48:274–276. PMID: 26639740.19. Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, et al. Prospective randomized study of endovenous radiofrequency obliteration (closure procedure) versus ligation and stripping in a selected patient population (EVOLVeS Study). J Vasc Surg. 2003; 38:207–214. PMID: 12891099.20. Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, et al. Prospective randomised study of endovenous radiofrequency obliteration (closure) versus ligation and vein stripping (EVOLVeS): two-year follow-up. Eur J Vasc Endovasc Surg. 2005; 29:67–73. PMID: 15570274.21. Goode SD, Chowdhury A, Crockett M, Beech A, Simpson R, Richards T, et al. Laser and radiofrequency ablation study (LARA study): a randomised study comparing radiofrequency ablation and endovenous laser ablation (810 nm). Eur J Vasc Endovasc Surg. 2010; 40:246–253. PMID: 20537570.22. Nordon IM, Hinchliffe RJ, Brar R, Moxey P, Black SA, Thompson MM, et al. A prospective double-blind randomized controlled trial of radiofrequency versus laser treatment of the great saphenous vein in patients with varicose veins. Ann Surg. 2011; 254:876–881. PMID: 21934487.23. Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings A, Eklof B. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg. 2011; 98:1079–1087. PMID: 21725957.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis and treatment of varicose veins and chronic venous insufficiency
- Clinical Implications of Venous Hypertension in the Management of Chronic Venous Disease
- Changes in the management of hypertension, diabetes mellitus, and hypercholesterolemia in Korean adults before and during the COVID-19 pandemic: data from the 2010-2020 Korea National Health and Nutrition Examination Survey
- Clarifying Misnomers in Venous Diseases
- Chronic Venous Disease is a Progressive Disease that Requires Early Intervention