Korean J Pain.
2023 Jan;36(1):106-112. 10.3344/kjp.22249.
Risk analysis of musculoskeletal pain intervention using corticosteroid during COVID-19 pandemic: a cohort study
- Affiliations
-
- 1Sports Medicine Department, University Malaya Medical Centre, Kuala Lumpur, Malaysia
- 2Sports Medicine Unit, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia
- KMID: 2537617
- DOI: http://doi.org/10.3344/kjp.22249
Abstract
- Background
Most international bodies recommended against musculoskeletal steroid injection during the COVID-19 pandemic, fearing that the immunosuppressive effects of the steroid could worsen COVID-19 infection, thus prolonging the suffering of patients with severe musculoskeletal disease. The authors’ aim is to analyze the risk of COVID-19 infection after musculoskeletal injections.
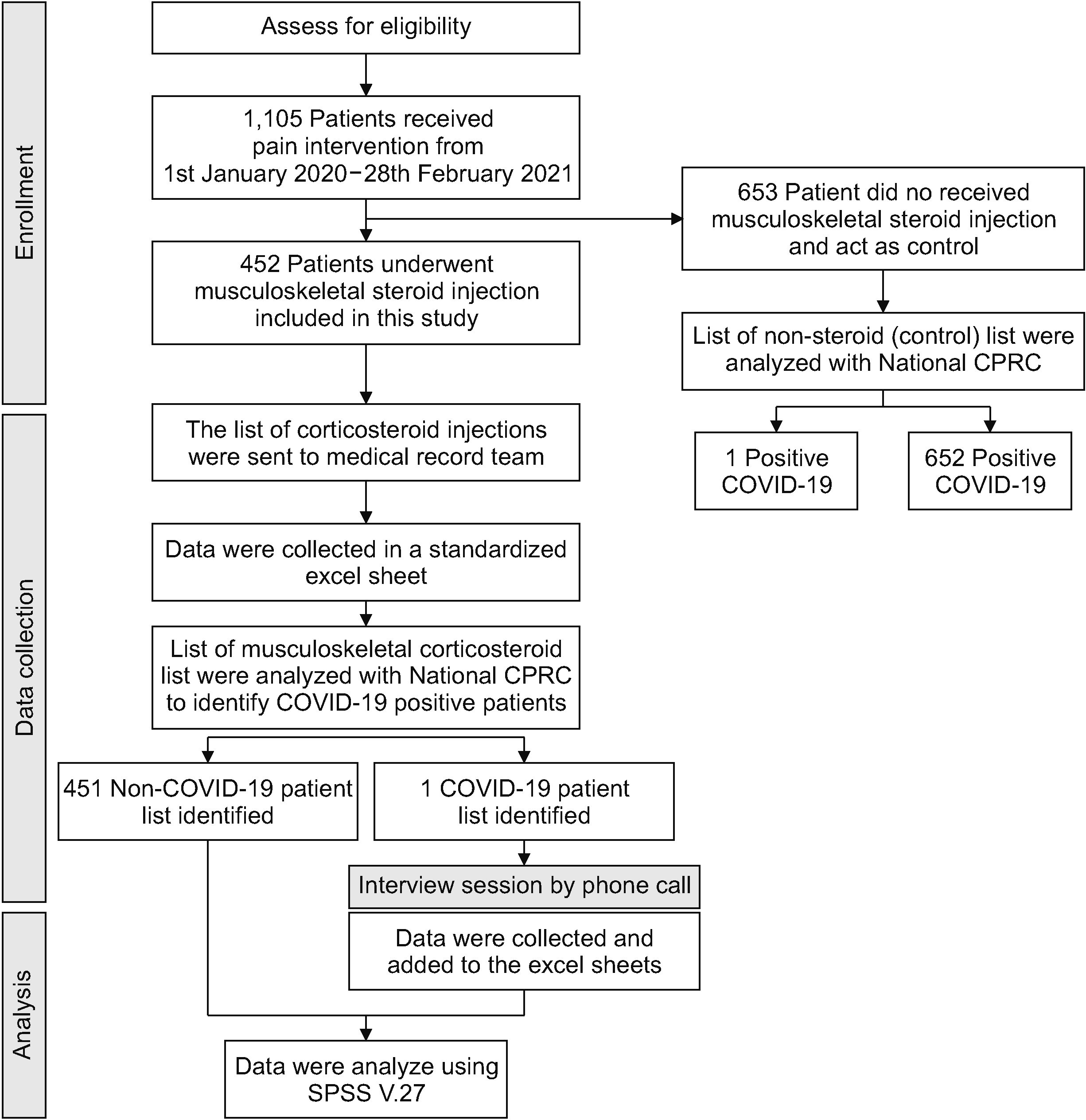
Methods
This is a retrospective study of patients who visited a sports medicine clinic and received musculoskeletal steroid injections between January 1, 2020 and February 28, 2021. The collected data was compared with the national COVID-19 registry to identify positive COVID-19 patients. The patients were only considered positive for COVID-19 following corticosteroid injection within 3 months after injection.
Results
Out of 502 steroid injections; 79.7% (n = 400) received a single injection in one day, 19.1% (n = 96) received steroid injections at 2 sites in one day, and 1.2% (n = 6) received steroid injections at 3 sites in one day. Using the Fisherʼs exact test, there was no statistically significant association of COVID-19 infection between the steroid group and control group (relative risk, 1.44; 95% confidence interval, 0.9–23.1, P = 0.654). Only one patient contracted mild COVID-19 with no post COVID complications.
Conclusions
The authors recommend the use of musculoskeletal steroid injections in clinically indicated situation without having increased risk of COVID-19.
Keyword
Figure
Reference
-
1. Stephens MB, Beutler AI, O'Connor FG. 2008; Musculoskeletal injections: a review of the evidence. Am Fam Physician. 78:971–6. PMID: 18953975.2. MacMahon PJ, Eustace SJ, Kavanagh EC. 2009; Injectable corticosteroid and local anesthetic preparations: a review for radiologists. Radiology. 252:647–61. DOI: 10.1148/radiol.2523081929. PMID: 19717750.3. Ericson-Neilsen W, Kaye AD. 2014; Steroids: pharmacology, complications, and practice delivery issues. Ochsner J. 14:203–7. PMID: 24940130. PMCID: PMC4052587.4. Sytsma TT, Greenlund LK, Greenlund LS. 2018; Joint corticosteroid injection associated with increased influenza risk. Mayo Clin Proc Innov Qual Outcomes. 2:194–8. DOI: 10.1016/j.mayocpiqo.2018.01.005. PMID: 30225449. PMCID: PMC6124339.5. National Health Service. 2020. Clinical guide for the management of patients with musculoskeletal and rheumatic conditions on corticosteroids during the coronavirus pandemic [Internet]. National Health Service;London: Available at: https://www.csp.org.uk/media/1264903.6. Shanthanna H, Cohen SP, Strand N, Lobo CA, Eldabe S, Bhatia A, et al. Recommendations on chronic pain practice during the COVID-19 pandemic. ASRA/ESRA COVID-19 guidance for chronic pain practice [Internet]. American Society of Regional Anesthesia and Pain Medicine;Pittsburgh (PA): Available at: https://www.hlz.hr/wp-content/uploads/2020/04/asra_esra_covid-19_and_chronic_pain-1.pdf.7. Dalili D, Fairhead R, Mermekli A, Papanikitas J, Teh J, Hughes R, et al. 2021; Impact of the COVID-19 pandemic on corticosteroid injection services: a national survey of members of the British Society of Skeletal Radiologists (BSSR). Br J Radiol. 94:20210327. DOI: 10.1259/bjr.20210327. PMID: 34520669. PMCID: PMC9328042.8. Friedly JL, Comstock BA, Heagerty PJ, Bauer Z, Rothman MS, Suri P, et al. 2018; Systemic effects of epidural steroid injections for spinal stenosis. Pain. 159:876–83. DOI: 10.1097/j.pain.0000000000001158. PMID: 29394207.9. Abdul AJ, Ghai B, Bansal D, Sachdeva N, Bhansali A, Dhatt SS. 2017; Hypothalamic pituitary adrenocortical axis suppression following a single epidural injection of methylprednisolone acetate. Pain Physician. 20:E991–1001. DOI: 10.36076/ppj/2017.7.E991. PMID: 29149147.10. Iranmanesh A, Gullapalli D, Singh R, Veldhuis JD. 2017; Hypothalamo-pituitary-adrenal axis after a single epidural triamcinolone injection. Endocrine. 57:308–13. DOI: 10.1007/s12020-017-1357-7. PMID: 28674775. PMCID: PMC5554884.11. Jayaraj VJ, Rampal S, Ng CW, Chong DWQ. 2021; The epidemiology of COVID-19 in Malaysia. Lancet Reg Health West Pac. 17:100295. DOI: 10.1016/j.lanwpc.2021.100295. PMID: 34704083. PMCID: PMC8529946.12. Bugeja M, Mariani J, Dowling J, Stringaro G, Portelli JL, Sant K, et al. 2021; Musculoskeletal steroid injections during the COVID-19 pandemic. J Orthop. 26:103–6. DOI: 10.1016/j.jor.2021.07.017. PMID: 34312576. PMCID: PMC8294711.13. McKean D, Chung SL, Fairhead R, Bannister O, Magliano M, Papanikitas J, et al. 2020; Corticosteroid injections during the COVID-19 pandemic: experience from a UK centre. Bone Jt Open. 1:605–11. DOI: 10.1302/2633-1462.19.BJO-2020-0130.R1. PMID: 33215158. PMCID: PMC7659632.14. Azwan Aziz M, Abu Hanifah R, Mohd Nahar AM. 2021; Musculoskeletal corticosteroid injection during COVID-19 pandemic in Sabah: is it safe? Adv Orthop. 2021:8863210. DOI: 10.1155/2021/8863210. PMID: 33824767. PMCID: PMC8006753.15. Chang CY, Prabhakar A, Staffa SJ, Husseini JS, Kheterpal AB, Simeone FJ, et al. 2021; Symptomatic COVID-19 infections in outpatient image-guided corticosteroid injection patients during the lockdown phase. Skeletal Radiol. 50:1117–23. DOI: 10.1007/s00256-020-03656-w. PMID: 33108512. PMCID: PMC7590247.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Did the COVID-19 pandemic impact the surgical treatment of febrile acute appendicitis at a single center in Korea, a country not under lockdown? Observational cohort study
- The profile of musculoskeletal pain and its associations with sleep quality and depression during the COVID-19 in Turkey
- The impact of the COVID-19 pandemic on in-hospital mortality in patients admitted through the emergency department
- The Management of Thyroid Disease in COVID-19 Pandemic
- Depression in pregnant and postpartum women during COVID-19 pandemic: systematic review and meta-analysis