J Cerebrovasc Endovasc Neurosurg.
2022 Dec;24(4):366-371. 10.7461/jcen.2022.E2021.07.011.
Hemiballism, a rare complication of coil embilization
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Gumi Hospital, Gumi, Korea
- KMID: 2537321
- DOI: http://doi.org/10.7461/jcen.2022.E2021.07.011
Abstract
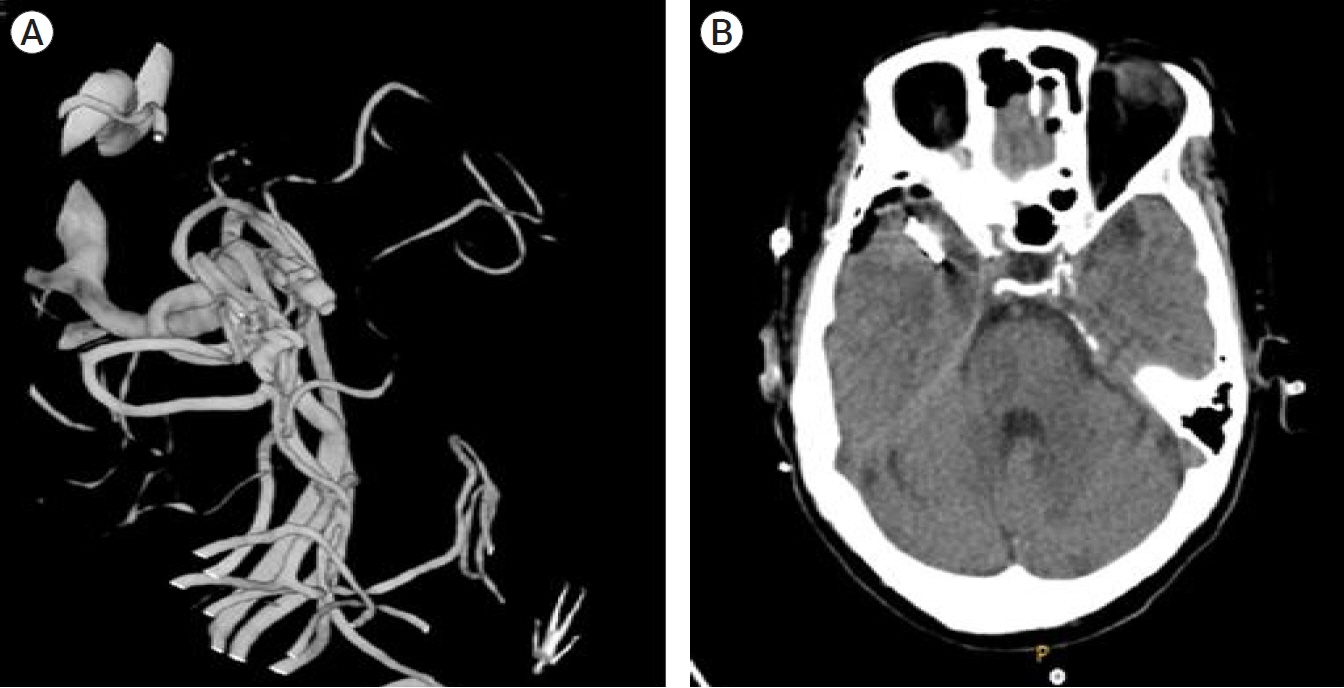
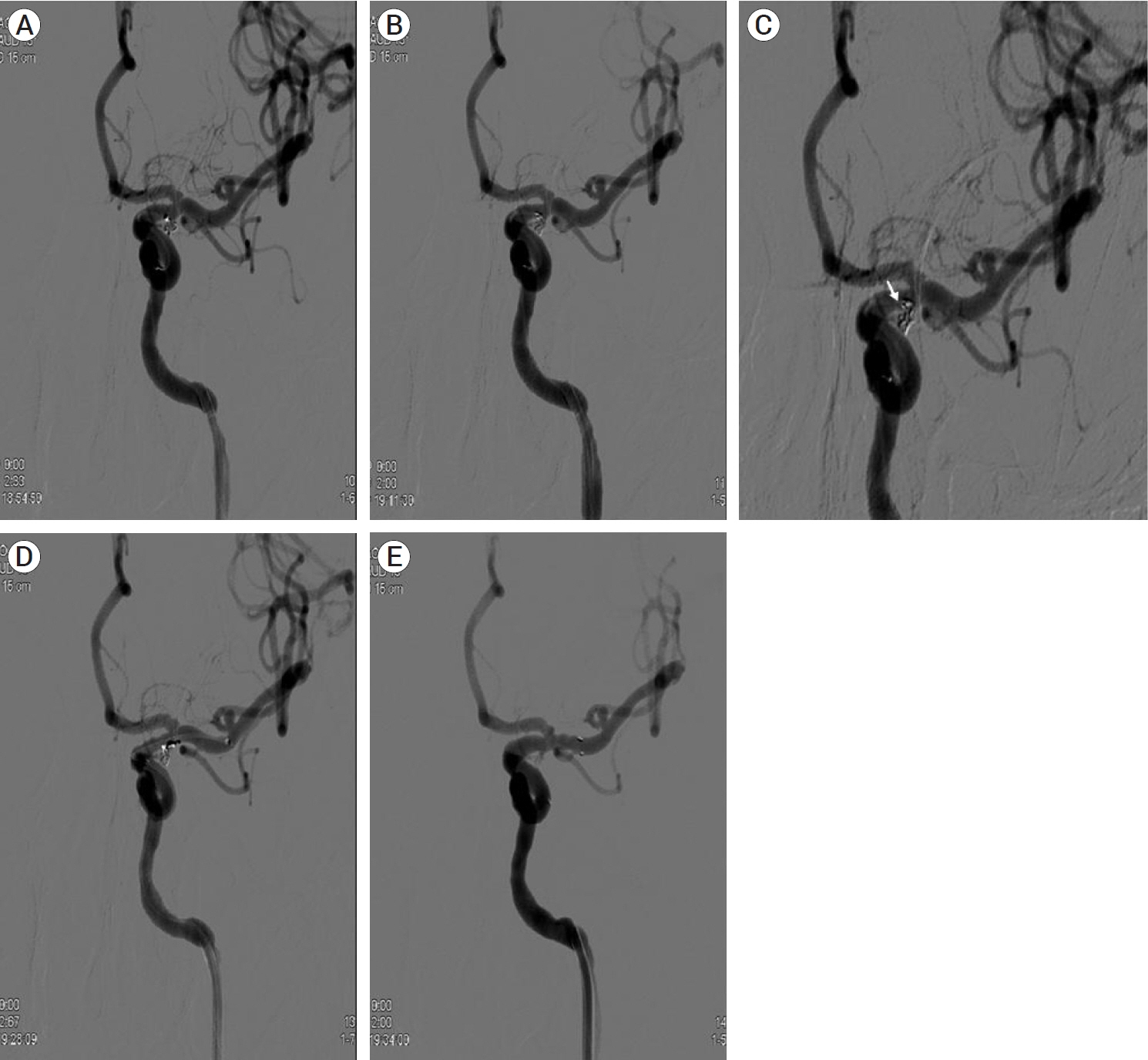
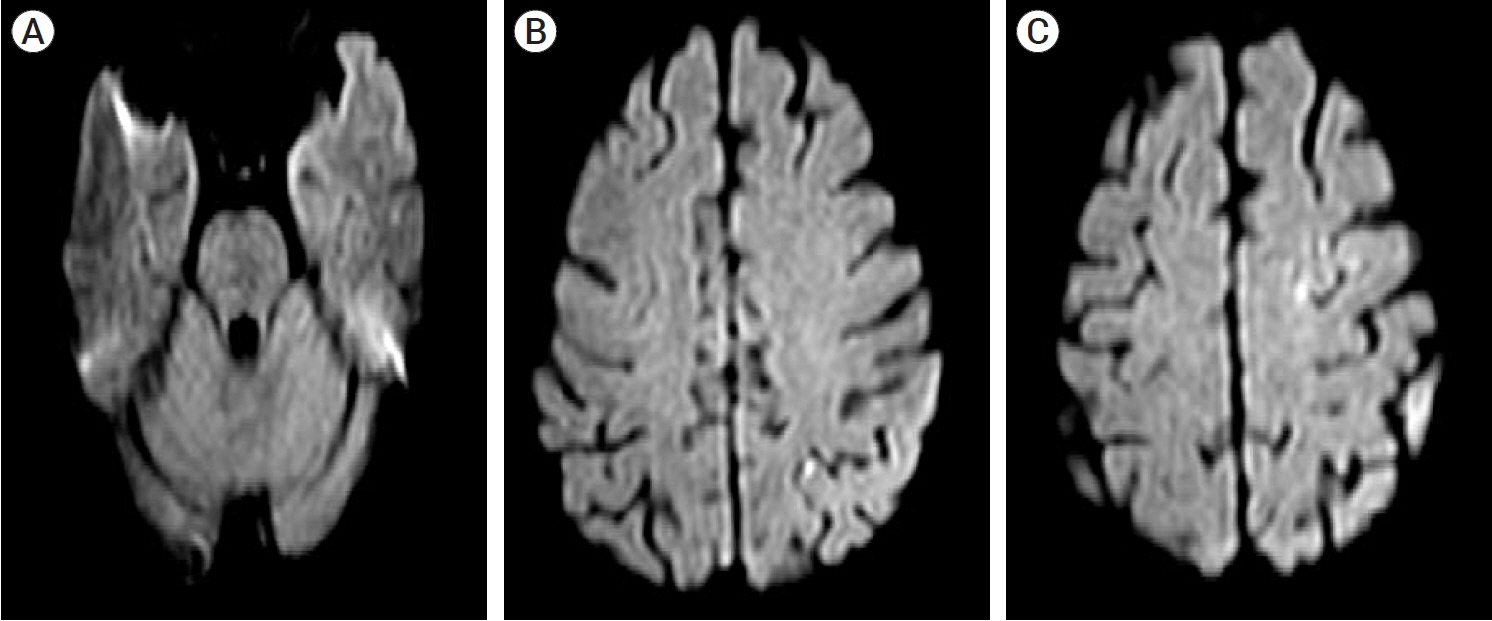
- Thromboembolism is one of the major complications during coil embolization of an aneurysm, which usually causes familiar neurological deficits, such as, weakness, aphasia, etc. We report a rare complication by thromboembolism after coil embolization causing hemiballism. A 69-year-old female presented with unruptured posterior communicating artery aneurysm and was treated by coil embolization. After the procedure, the patient showed global aphasia and right hemiparesis, and there were small multiple, scattered infarctions on the left middle cerebral artery territory. The neurologic deficit subsided after five days, but hemballism occurred thereafter. There was no other medical history to explain the hemiballism. The patient was treated with clonazepam and antiepileptics and the hemiballism subsided at postoperative day 20. We report a case of rare complication, hemiballism, during coil embolization.
Figure
Reference
-
1. Chung SJ, Im JH, Lee MC, Kim JS. Hemichorea after stroke: clinical-radiological correlation. J Neurol. 2004; Jun. 251(6):725–9.
Article2. Ghika-Schmid F, Ghika J, Regli F, Bogousslavsky J. Hyperkinetic movement disorders during and after acute stroke: the Lausanne Stroke Registry. J Neurol Sci. 1997; Mar. 146(2):109–16.
Article3. Morigaki R, Uno M, Matsubara S, Satoh K, Nagahiro S. Choreoathetosis due to rupture of a distal accessory anterior cerebral artery aneurysm. Cerebrovasc Dis. 2008; 25(3):285–7.
Article4. Morigaki R, Uno M, Suzue A, Nagahiro S. Hemichorea due to hemodynamic ischemia associated with extracranial carotid artery stenosis. Report of two cases. J Neurosurg. 2006; Jul. 105(1):142–7.5. Sakai K, Kyoshima K, Ohigashi Y, Unoki T, Kobayashi S, Meguro M. Generalized choreic movement associated with subarachnoid hemorrhage. No To Shinkei. 1991; 43(9):875–80.6. Scott BL, Jankovic J. Delayed-onset progressive movement disorders after static brain lesions. Neurology. 1996; Jan. 46(1):68–74.
Article7. Shrestha P, Adhikari J, Poudel D, Pathak R, Karmacharya P. Cortical hemiballism: a case of hemiballismus associated with parietal lobe infarct. N Am J Med Sci. 2015; Dec. 7(12):572–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hemiballism as First Isolated Manifestation Following Caudate Infarction
- A Case of Hemiballism in Elderly Stroke Improved by Conventional Rehabilitation Therapy and Low Dose Quetiapine
- Migrated coil and damaged stent removal during coil embolization, using an additional, retrievable stent: A case report
- A Case of Hemiballism-Hemichorea Movement Disorder
- A Case of Hemiballism