Ann Pediatr Endocrinol Metab.
2022 Dec;27(4):289-299. 10.6065/apem.2142230.115.
Cardiometabolic risk factors and metabolic syndrome based on severity of obesity in Korean children and adolescents: data from the Korea National Health and Nutrition Examination Survey 2007–2018
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2537241
- DOI: http://doi.org/10.6065/apem.2142230.115
Abstract
- Purpose
Data regarding cardiometabolic risk factors (CMRFs) and metabolic syndrome (MetS) by body mass index (BMI) category in Korean youth are sparse.
Methods
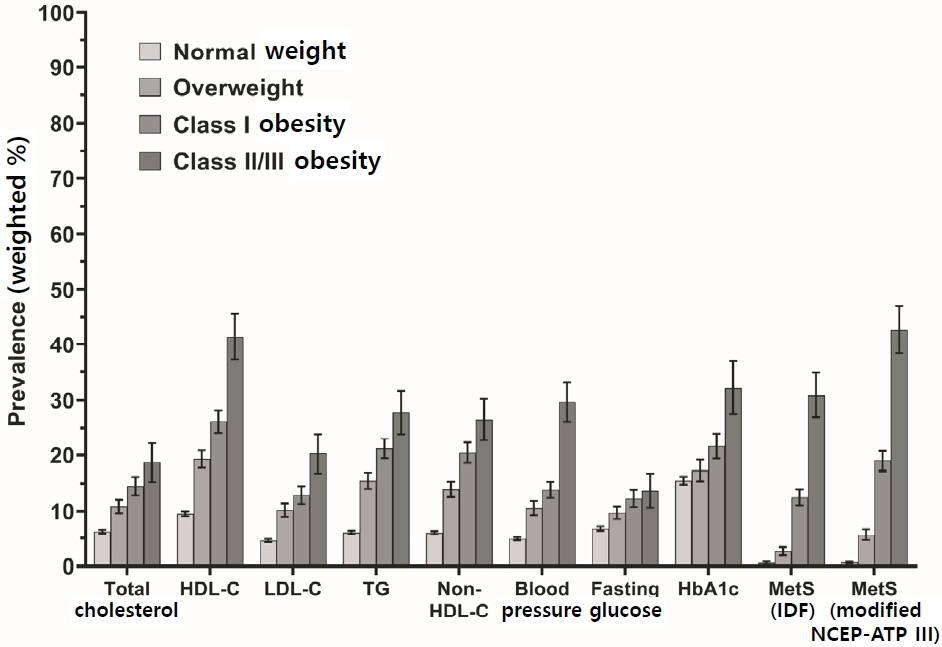
Among the participants of the Korea National Health and Nutrition Examination Survey 2007–2018, 9,984 youth aged 10–18 years were included in the study. Participants were classified into 4 groups based on BMI status: normal weight, overweight, class I, and class II/III obesity. CMRF prevalence, including total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides, blood pressure, fasting glucose, glycated hemoglobin, and MetS, were determined using the International Diabetes Federation (IDF) and modified National Cholesterol Education Program-Adult Treatment Panel (NCEP-ATP) III criteria based on BMI category.
Results
The prevalence of overweight, class I, class II, and class III obesity was 9.52%, 7.73%, 2.10%, and 0.32%, respectively. Mean CMRF values increased with BMI, except high-density lipoprotein cholesterol. Age- and sex-adjusted odds ratios (ORs) for prediction of CMRFs also increased with BMI. Adjusted ORs for MetS among overweight, class I, and class II/II obesity were 54.2, 283.3, and 950.3 for IDF criteria and 9.56, 37.9, and 126.8 for NCEP-ATP III criteria, respectively (all p<0.001).
Conclusion
Class II and III obesity in Korean children and adolescents was associated with significantly increased CMRF and MetS prevalence. Therefore, it can be useful to measure CMRFs in obese children and adolescents. Further studies are required to establish screening guidelines based on obesity severity.
Keyword
Figure
Cited by 2 articles
-
Glycated albumin may have a complementary role to glycated hemoglobin in glucose monitoring in childhood acute leukemia
Soo Yeun Sim, Su Jin Park, Jae Won Yoo, Seongkoo Kim, Jae Wook Lee, Nack-Gyun Chung, Bin Cho, Byung-Kyu Suh, Moon Bae Ahn
Ann Pediatr Endocrinol Metab. 2024;29(4):266-275. doi: 10.6065/apem.2346100.050.Association between metabolically healthy obesity and carotid intima-media thickness in Korean adolescents with overweight and obesity
Sohyun Shin, Hwa Young Kim, Joowon Lee, Young Jin Ryu, Ji Young Kim, Jaehyun Kim
Ann Pediatr Endocrinol Metab. 2024;29(4):227-233. doi: 10.6065/apem.2346192.096.
Reference
-
References
1. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017; 390:2627–42.2. Kim JH, Moon JS. Secular trends in pediatric overweight and obesity in Korea. J Obes Metab Syndr. 2020; 29:12–7.3. Lim S, Jang HC, Park KS, Cho SI, Lee MG, Joung H, et al. Changes in metabolic syndrome in American and Korean youth, 1997-2008. Pediatrics. 2013; 131:e214–22.4. Park MJ, Boston BA, Oh M, Jee SH. Prevalence and trends of metabolic syndrome among Korean adolescents: from the Korean NHANES survey, 1998-2005. J Pediatr. 2009; 155:529–34.5. Park SI, Suh J, Lee HS, Song K, Choi Y, Oh JS, et al. Tenyear trends of metabolic syndrome prevalence and nutrient intake among Korean children and adolescents: a population-based study. Yonsei Med J. 2021; 62:344–51.6. Oh K, Jang MJ, Lee NY, Moon JS, Lee CG, Yoo MH, et al. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Korean J Pediatr. 2008; 51:950–5.7. Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr. 2014; 168:561–6.8. Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. 2015; 373:1307–17.9. Valerio G, Maffeis C, Balsamo A, Del Giudice EM, Brufani C, Grugni G, et al. Severe obesity and cardiometabolic risk in children: comparison from two international classification systems. PLoS One. 2013; 8:e83793.10. US Preventive Services Task Force, Barton M. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2010; 125:361–7.11. Kassi E, Pervanidou P, Kaltsas G, Chrousos G. Metabolic syndrome: definitions and controversies. BMC Med. 2011; 9:48.12. DeFronzo RA, Ferrannini E. Insulin resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care. 1991; 14:173–94.13. Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR, et al. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation. 2010; 122:1604–11.14. Morrison JA, Friedman LA, Wang P, Glueck CJ. Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. J Pediatr. 2008; 152:201–6.15. Reisinger C, Nkeh-Chungag BN, Fredriksen PM, Goswami N. The prevalence of pediatric metabolic syndrome-a critical look on the discrepancies between definitions and its clinical importance. Int J Obes (Lond). 2021; 45:12–24.16. Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009; 9:322–9.17. Cho WK, Han K, Ahn MB, Park YM, Jung MH, Suh BK, et al. Metabolic risk factors in Korean adolescents with severe obesity: results from the Korea National Health and Nutrition Examination Surveys (K-NHANES) 2007-2014. Diabetes Res Clin Pract. 2018; 138:169–76.18. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77.19. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61:135–49.20. Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, et al. Pediatric obesity-assessment, treatment, and prevention: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2017; 102:709–57.21. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011; 128 Suppl 5(Suppl 5):S213–56.22. Lim JS, Kim EY, Kim JH, Yoo JH, Yi KH, Chae HW, et al. 2017 Clinical practice guidelines for dyslipidemia of Korean children and adolescents. Clin Exp Pediatr. 2020; 63:454–62.23. Kim SH, Park Y, Song YH, An HS, Shin JI, Oh JH, et al. Blood pressure reference values for normal weight Korean children and adolescents: data from the Korea National Health and Nutrition Examination Survey 1998-2016: The Korean Working Group of Pediatric Hypertension. Korean Circ J. 2019; 49:1167–80.24. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care. 2021; 44(Suppl 1):S15–33.25. Zimmet P, Alberti KG, Kaufman F, Tajima N, Silink M, Arslanian S, et al. The metabolic syndrome in children and adolescents - an IDF consensus report. Pediatr Diabetes. 2007; 8:299–306.26. Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003; 157:821–7.27. Czeczelewski M, Czeczelewski J, Czeczelewska E, Galczak-Kondraciuk A. Association of body composition indexes with cardio-metabolic risk factors. Obes Med. 2020; 17:100171.28. Inge TH, King WC, Jenkins TM, Courcoulas AP, Mitsnefes M, Flum DR, et al. The effect of obesity in adolescence on adult health status. Pediatrics. 2013; 132:1098–104.29. Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013; 128:1689–712.30. Chu SY, Jung JH, Park MJ, Kim SH. Risk assessment of metabolic syndrome in adolescents using the triglyceride/ high-density lipoprotein cholesterol ratio and the total cholesterol/high-density lipoprotein cholesterol ratio. Ann Pediatr Endocrinol Metab. 2019; 24:41–8.31. Lee SH, Ahn MB, Choi YJ, Kim SK, Kim SH, Cho WK, et al. Comparison of different criteria for the definition of insulin resistance and its relationship to metabolic risk in children and adolescents. Ann Pediatr Endocrinol Metab. 2020; 25:227–33.32. Geserick M, Vogel M, Gausche R, Lipek T, Spielau U, Keller E, et al. Acceleration of BMI in early childhood and risk of sustained obesity. N Engl J Med. 2018; 379:1303–12.33. Dai XY, Zheng YY, Tang JN, Yang XM, Guo QQ, Zhang JC, et al. Triglyceride to high-density lipoprotein cholesterol ratio as a predictor of long-term mortality in patients with coronary artery disease after undergoing percutaneous coronary intervention: a retrospective cohort study. Lipids Health Dis. 2019; 18:210.34. Castorani V, Polidori N, Giannini C, Blasetti A, Chiarelli F. Insulin resistance and type 2 diabetes in children. Ann Pediatr Endocrinol Metab. 2020; 25:217–26.35. Jeon YJ, Jung IA, Kim SH, Cho WK, Jeong SH, Cho KS, et al. Serum ferritin level is higher in male adolescents with obesity: results from the Korean National Health and Nutrition Examination Survey 2010. Ann Pediatr Endocrinol Metab. 2013; 18:141–7.36. Ward ZJ, Long MW, Resch SC, Giles CM, Cradock AL, Gortmaker SL. Simulation of growth trajectories of childhood obesity into adulthood. N Engl J Med. 2017; 377:2145–53.37. Kim JY, Jeon JY. Role of exercise on insulin sensitivity and beta-cell function: is exercise sufficient for the prevention of youth-onset type 2 diabetes? Ann Pediatr Endocrinol Metab. 2020; 25:208–16.38. Cunningham SA, Kramer MR, Narayan KM. Incidence of childhood obesity in the United States. N Engl J Med. 2014; 370:403–11.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Obesity and Metabolic Syndrome among Children and Adolescents in Korea
- Therapeutic approaches to obesity and metabolic syndrome in children and adolescents
- Handgrip Strength Is Associated with Metabolic Syndrome and Insulin Resistance in Children and Adolescents: Analysis of Korea National Health and Nutrition Examination Survey 2014–2018
- Prevalence of the Metabolic Syndrome in Korean Children and Adolescents according to the International Diabetes Federation Definition in Children and Adolescents
- Prevalence of Metabolic Syndrome and Obesity in Adolescents Aged 12 to 19 Years: Comparison between the United States and Korea