Korean Circ J.
2022 Dec;52(12):865-875. 10.4070/kcj.2022.0143.
Late Outcomes of Pediatric and Congenital Heart Disease Patients Following Cardiac Resynchronization Therapy
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Thoracic and Cardiovascular Surgery, Seoul National University Children’s Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2536788
- DOI: http://doi.org/10.4070/kcj.2022.0143
Abstract
- Background and Objectives
Cardiac resynchronization therapy (CRT) is an effective treatment for heart failure. However, in pediatric and congenital heart disease (CHD) patients, current adult indications cannot be directly applied because of heterogeneity in anatomy and diagnosis. Therefore, CRT responses and clinical outcomes in these patients were investigated to derive possible candidates for CRT.
Methods
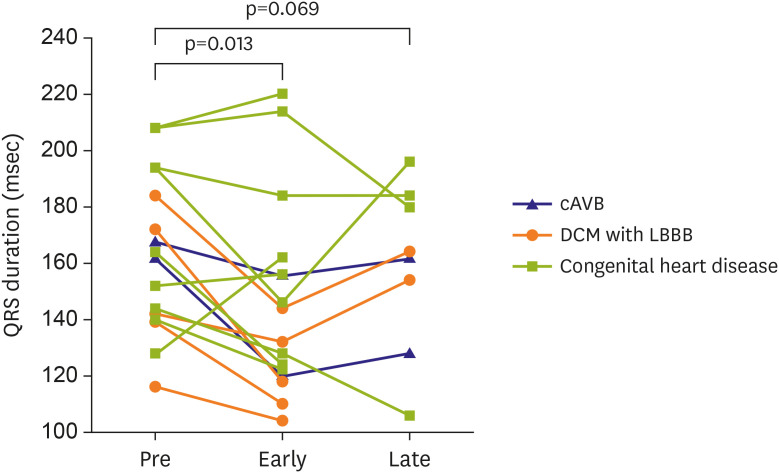
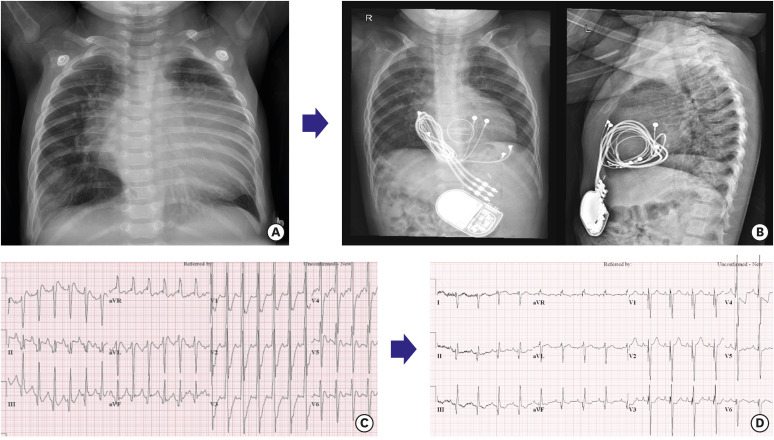
This study retrospectively analyzed 16 pediatric and CHD patients who underwent CRT implantation at a single center in early (0.7±0.2 year) and late (4.7±0.3 years) follow-up period after CRT.
Results
The median age at CRT implantation was 2.5 (0.3–37.2) years, and median follow-up duration was 6.3 (0.1–13.6) years. Thirteen had non-transvenous CRT. Two had congenital complete atrioventricular (AV) block with previous right ventricular pacing, 5 had dilated cardiomyopathy (DCM) with left bundle branch block, and 9 had CHD. The mean ejection fraction of the systemic ventricle increased from 28.1±10.0% to 44.3±21.0% (p=0.003) in early and 51.8±16.3% (p=0.012) in late outcome. The mean functional class improved from 3.1±0.9 to 1.8±1.1 after CRT (p=0.003). Twelve patients (75%) showed improvement in ventricular function or functional class after CRT. Proportion of responders differed between patients without CHD (2/2 patients with complete AV block and 5/5 with DCM, 100%) and those with CHD (5/9, 56%), although statistical significance was not reached (p=0.088).
Conclusions
CRT improved ventricular function and functional status according to the underlying condition in pediatric and CHD patients. However, further large and longer-term studies are needed to establish the guideline for the patient selection of CRT in these patients.
Figure
Reference
-
1. Glikson M, Nielsen JC, Kronborg MB, et al. 2021 ESC guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021; 42:3427–3520. PMID: 34455430.2. Cleland JG, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005; 352:1539–1549. PMID: 15753115.3. Linde C, Ellenbogen K, McAlister FA. Cardiac resynchronization therapy (CRT): clinical trials, guidelines, and target populations. Heart Rhythm. 2012; 9:S3–13. PMID: 22521934.4. Hsu DT, Pearson GD. Heart failure in children: part I: history, etiology, and pathophysiology. Circ Heart Fail. 2009; 2:63–70. PMID: 19808316.5. Kubuš P, Rubáčková Popelová J, Kovanda J, Sedláček K, Janoušek J. Long-term outcome of patients with congenital heart disease undergoing cardiac resynchronization therapy. J Am Heart Assoc. 2021; 10:e018302. PMID: 33719495.6. Marelli AJ, Mackie AS, Ionescu-Ittu R, Rahme E, Pilote L. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007; 115:163–172. PMID: 17210844.7. Diller GP, Kempny A, Alonso-Gonzalez R, et al. Survival prospects and circumstances of death in contemporary adult congenital heart disease patients under follow-up at a large tertiary centre. Circulation. 2015; 132:2118–2125. PMID: 26369353.8. Motonaga KS, Dubin AM. Cardiac resynchronization therapy for pediatric patients with heart failure and congenital heart disease: a reappraisal of results. Circulation. 2014; 129:1879–1891. PMID: 24799504.9. Janousek J, Gebauer RA, Abdul-Khaliq H, et al. Cardiac resynchronisation therapy in paediatric and congenital heart disease: differential effects in various anatomical and functional substrates. Heart. 2009; 95:1165–1171. PMID: 19307198.10. Leon AR, Greenberg JM, Kanuru N, et al. Cardiac resynchronization in patients with congestive heart failure and chronic atrial fibrillation: effect of upgrading to biventricular pacing after chronic right ventricular pacing. J Am Coll Cardiol. 2002; 39:1258–1263. PMID: 11955841.11. Song MK, Kim NY, Bae EJ, et al. Long-term follow-up of epicardial pacing and left ventricular dysfunction in children with congenital heart block. Ann Thorac Surg. 2020; 109:1913–1920. PMID: 31715154.12. Risum N, Jons C, Olsen NT, et al. Simple regional strain pattern analysis to predict response to cardiac resynchronization therapy: rationale, initial results, and advantages. Am Heart J. 2012; 163:697–704. PMID: 22520537.13. Yin Y, Dimopoulos K, Shimada E, et al. Early and late effects of cardiac resynchronization therapy in adult congenital heart disease. J Am Heart Assoc. 2019; 8:e012744. PMID: 31657270.14. Dubin AM, Janousek J, Rhee E, et al. Resynchronization therapy in pediatric and congenital heart disease patients: an international multicenter study. J Am Coll Cardiol. 2005; 46:2277–2283. PMID: 16360058.15. Breithardt OA, Sinha AM, Schwammenthal E, et al. Acute effects of cardiac resynchronization therapy on functional mitral regurgitation in advanced systolic heart failure. J Am Coll Cardiol. 2003; 41:765–770. PMID: 12628720.16. Miyazaki A, Negishi J, Hayama Y, et al. Evaluating the response to cardiac resynchronization therapy performed with a new ventricular morphology-based strategy for congenital heart disease. Heart Vessels. 2019; 34:1340–1350. PMID: 30863899.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiac Resynchronization Therapy in Pediatric Patients and Congenital Heart Disease: What Issues Remain to Solve?
- Cardiac Resynchronization Therapy Defibrillator Treatment in a Child with Heart Failure and Ventricular Arrhythmia
- Resynchronization Therapy in Congenital Heart Disease
- Cardiac Resynchronization Therapy in Infant with Dilated Cardiomyopathy during Extracorporeal Membrane Oxygenator
- Implantable Cardioverter-Defibrillator and Cardiac Resynchronization Therapy