Clin Exp Otorhinolaryngol.
2022 Nov;15(4):364-371. 10.21053/ceo.2022.01053.
Risk Factors and Characteristics of the Recurrence of Juvenile Nasopharyngeal Angiofibroma: A 22-Year Experience With 123 Cases at a Tertiary Center
- Affiliations
-
- 1Department of Otorhinolaryngology Head and Neck Surgery, the First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- 2Institute of Otorhinolaryngology Head and Neck Surgery, Sun Yat-sen University, Guangzhou, China
- 3Guangzhou Key Laboratory of Otorhinolaryngology, Guangzhou, China
- 4Department of Otorhinolaryngology Head and Neck Surgery, the Sixth Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- KMID: 2536535
- DOI: http://doi.org/10.21053/ceo.2022.01053
Abstract
Objectives
. Despite the efficacy of surgical treatments, the high rate of recurrence in juvenile nasopharyngeal angiofibroma (JNA) after surgery remains an unresolved problem. The present study comprehensively analyzed the risk factors and characteristics of JNA recurrence, providing clinical guidance for reducing recurrence.
Methods
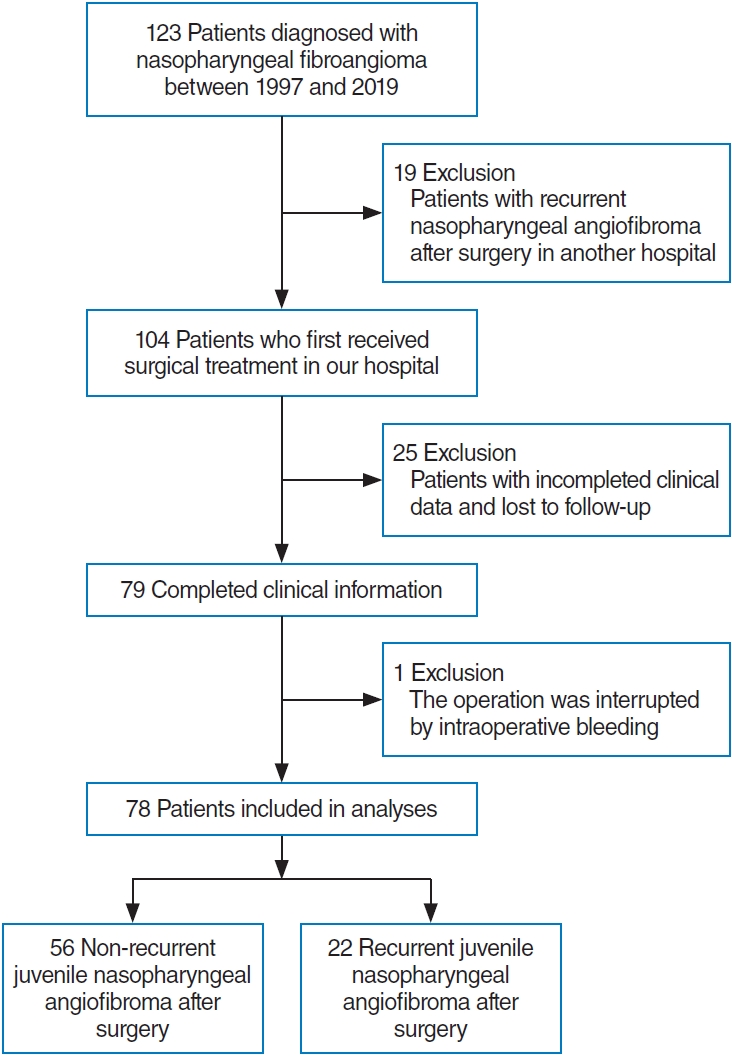
. A total of 123 patients who underwent surgery for JNA between 1997 and 2019 at a single hospital were analyzed retrospectively. Univariate and multivariate analyses were used to assess the clinical risk factors for the recurrence of JNA. The relapse-free survival and annual cumulative recurrence rates were analyzed for subgroups defined according to clinical parameters.
Results
. After screening, 78 of the 123 patients were included in the present study. The main risk factors associated with JNA recurrence included the year of diagnosis, tumor size, sphenoid bone invasion, Radkowski stage, surgical approach, and intraoperative bleeding. Importantly, the surgical approach and sphenoid bone invasion were independent prognostic factors affecting recurrence. Patients who underwent endoscopic surgery without sphenoid bone invasion exhibited longer relapse-free survival. In the present study, the overall cumulative recurrence rate of JNA was 38.7%, and recurrence occurred mainly in the first year after the initial surgery.
Conclusion
. Endoscopic surgery achieved better relapse-free survival in JNA patients, and patients with sphenoid bone invasion should be carefully explored to avoid residual JNA. The recurrence rate of JNA differed among subgroups defined based on clinical parameters and was highest in the first year after surgery. Computed tomography or magnetic resonance imaging, along with close follow-up, should be performed strictly within 1 year after the primary operation.
Figure
Reference
-
1. Lund VJ, Stammberger H, Nicolai P, Castelnuovo P, Beal T, Beham A, et al. European position paper on endoscopic management of tumours of the nose, paranasal sinuses and skull base. Rhinol Suppl. 2010; Jun. 22:1–143.2. Lao WP, Lagabon KJ, Arom GA, Walker PC, Lee SC. Combined endoscopic and transoral resection of a high-staged juvenile nasopharyngeal angiofibroma: a pictorial essay. Head Neck. 2021; Feb. 43(2):719–24.
Article3. Nicolai P, Schreiber A, Bolzoni Villaret A. Juvenile angiofibroma: evolution of management. Int J Pediatr. 2012; 2012:412545.
Article4. Makhasana JA, Kulkarni MA, Vaze S, Shroff AS. Juvenile nasopharyngeal angiofibroma. J Oral Maxillofac Pathol. 2016; May-Aug. 20(2):330.
Article5. Duvall AJ 3rd, Moreano AE. Juvenile nasopharyngeal angiofibroma: diagnosis and treatment. Otolaryngol Head Neck Surg. 1987; Dec. 97(6):534–40.
Article6. Hackman T, Snyderman CH, Carrau R, Vescan A, Kassam A. Juvenile nasopharyngeal angiofibroma: the expanded endonasal approach. Am J Rhinol Allergy. 2009; Jan-Feb. 23(1):95–9.
Article7. Howard DJ, Lloyd G, Lund V. Recurrence and its avoidance in juvenile angiofibroma. Laryngoscope. 2001; Sep. 111(9):1509–11.
Article8. Fyrmpas G, Konstantinidis I, Constantinidis J. Endoscopic treatment of juvenile nasopharyngeal angiofibromas: our experience and review of the literature. Eur Arch Otorhinolaryngol. 2012; Feb. 269(2):523–9.
Article9. Bleier BS, Kennedy DW, Palmer JN, Chiu AG, Bloom JD, O’Malley BW Jr. Current management of juvenile nasopharyngeal angiofibroma: a tertiary center experience 1999-2007. Am J Rhinol Allergy. 2009; May-Jun. 23(3):328–30.
Article10. Liu Z, Hua W, Zhang H, Wang J, Song X, Hu L, et al. The risk factors for residual juvenile nasopharyngeal angiofibroma and the usual residual sites. Am J Otolaryngol. 2019; May-Jun. 40(3):343–6.
Article11. Pamuk AE, Ozer S, Suslu AE, Akgoz A, Onerci M. Juvenile nasopharyngeal angiofibroma: a single centre’s 11-year experience. J Laryngol Otol. 2018; Nov. 132(11):978–83.
Article12. Tan G, Ma Z, Long W, Liu L, Zhang B, Chen W, et al. Efficacy of preoperative transcatheter arterial embolization for nasopharyngeal angiofibroma: a comparative study. Cardiovasc Intervent Radiol. 2017; Jun. 40(6):836–44.
Article13. Desarda KK, Bora MP. Importance of pre-operative embolization in the surgery of nasopharyngeal angiofibroma. Indian J Otolaryngol Head Neck Surg. 1998; Jan. 50(1):36–9.
Article14. Gargula S, Saint-Maurice JP, Labeyrie MA, Eliezer M, Jourdaine C, Kania R, et al. Embolization of internal carotid artery branches in juvenile nasopharyngeal angiofibroma. Laryngoscope. 2021; Mar. 131(3):E775–80.
Article15. Dabholkar JP. Juvenile nasopharyngeal angiofibroma: clinical factors associated with recurrence and proposal of a staging system. J Surg Oncol. 2008; Aug. 98(2):73.
Article16. Sun XC, Wang DH, Yu HP, Wang F, Wang W, Jiang JJ. Analysis of risk factors associated with recurrence of nasopharyngeal angiofibroma. J Otolaryngol Head Neck Surg. 2010; Feb. 39(1):56–61.17. Radkowski D, McGill T, Healy GB, Ohlms L, Jones DT. Angiofibroma: changes in staging and treatment. Arch Otolaryngol Head Neck Surg. 1996; Feb. 122(2):122–9.
Article18. Carrillo JF, Albores O, Ramirez-Ortega MC, Aiello-Crocifoglio V, Onate-Ocana LF. An audit of nasopharyngeal fibromas. Eur J Surg Oncol. 2007; Jun. 33(5):655–61.
Article19. Li W, Ni Y, Lu H, Hu L, Wang D. Current perspectives on the origin theory of juvenile nasopharyngeal angiofibroma. Discov Med. 2019; Jun. 27(150):245–54.20. Roche PH, Paris J, Regis J, Moulin G, Zanaret M, Thomassin JM, et al. Management of invasive juvenile nasopharyngeal angiofibromas: the role of a multimodality approach. Neurosurgery. 2007; Oct. 61(4):768–77.21. Mishra A, Mishra SC. Time trends in recurrence of juvenile nasopharyngeal angiofibroma: experience of the past 4 decades. Am J Otolaryngol. 2016; May-Jun. 37(3):265–71.
Article22. Liu L, Wang R, Huang D, Han D, Ferguson EJ, Shi H, et al. Analysis of intra-operative bleeding and recurrence of juvenile nasopharyngeal angiofibromas. Clin Otolaryngol Allied Sci. 2002; Dec. 27(6):536–40.
Article23. Boghani Z, Husain Q, Kanumuri VV, Khan MN, Sangvhi S, Liu JK, et al. Juvenile nasopharyngeal angiofibroma: a systematic review and comparison of endoscopic, endoscopic-assisted, and open resection in 1047 cases. Laryngoscope. 2013; Apr. 123(4):859–69.
Article24. Lloyd G, Howard D, Phelps P, Cheesman A. Juvenile angiofibroma: the lessons of 20 years of modern imaging. J Laryngol Otol. 1999; Feb. 113(2):127–34.
Article25. Reyes C, Bentley H, Gelves JA, Solares CA, Byrd JK. Recurrence rate after endoscopic vs. open approaches for juvenile nasopharyngeal angiofibroma: a meta-analysis. J Neurol Surg B Skull Base. 2019; Dec. 80(6):577–85.
Article26. Huang Y, Liu Z, Wang J, Sun X, Yang L, Wang D. Surgical management of juvenile nasopharyngeal angiofibroma: analysis of 162 cases from 1995 to 2012. Laryngoscope. 2014; Aug. 124(8):1942–6.
Article27. Liu L, Wang R, Huang D, Han D, Yang W. Multiple factors analysis of intraoperative bleeding and recurrence of juvenile nasopharyngeal angiofibromas. Zhonghua Er Bi Yan Hou Ke Za Zhi. 2001; Jun. 36(3):220–3.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transnasal Endoscopic Resection of Juvenile Nasopharyngeal Angiofibroma: A Case Report
- A Case of Juvenile Nasopharyngeal Angiofibroma-Transnasal Endoscopic Surgery-
- Postoperative Residual Juvenile Nasopharyngeal Angiofibroma Treated with Gamma Knife Surgery
- A Case of Juvenile Nasopharyngeal Angiofibroma Treated by Unilateral Facial Degloving Approach
- A Case of Extranasopharyngeal Angiofibroma Arising from the Inferior Turbinate Removed without Pre-Operative Embolization